Macfarlane GJ, Kronisch C, Dean LE, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017 Feb;76(2):318-328. doi: 10.1136/annrheumdis-2016-209724. Epub 2016 Jul 4. Review. PubMed PMID: 27377815.
Wolfe F, Clauw DJ, Fitzcharles MA, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016 Dec;46(3):319-329. doi: 10.1016/j.semarthrit.2016.08.012. Epub 2016 Aug 30. PubMed PMID: 27916278.
Fitzcharles MA, Ste-Marie PA, Goldenberg DL, et al. Canadian Guidelines for the diagnosis and management of fibromyalgia syndrome. Canadian Rheumatology Association. https://rheum.ca/wp-content/uploads/2017/11/2012CanadianFMGuidelines_17August2012.pdf. Published August 2012. Accessed July 12, 2018.
Definition, Etiology, PathogenesisTop
Fibromyalgia (FM) is a pain syndrome of unknown etiology manifesting as chronic widespread musculoskeletal pain that is frequently accompanied by fatigue and multiple somatic and psychosomatic complaints.
Clinical Features and Natural HistoryTop
FM is 8 times more common in women than in men. It primarily affects women between 35 and 55 years of age. Symptoms of FM include chronic widespread muscle and joint pain generalized to multiple body regions, chronic fatigue, nonrestorative sleep, cognitive symptoms, sleep disturbances, headaches, lower abdominal pain or cramping, and depression. Some rheumatologists question the biological basis and concept of this disease.
FM is a common chronic condition and it is not typically degenerative or life-threatening. It is often associated with a high degree of disease burden, with few significant changes over time in the majority of patients. Complete remission, with full resolution of chronic pain, is rare.
DiagnosisTop
No biochemical or radiographic investigations are diagnostic of FM. Screening biochemical tests may include complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), creatine kinase (CK), and thyroid-stimulating hormone (TSH) levels; results should be within normal limits unless a concurrent or alternate process is present. Diagnosis is primarily made clinically.
To satisfy the modified 2016 FM criteria, the following 3 conditions must all be met (see Appendix):
1) Widespread pain index (WPI) ≥7 and symptom severity scale (SSS) score ≥5 or WPI 4 to 6 and SSS score ≥9. See www.pediatriconcall.com for scoring of the items included in those indices.
2) Generalized pain (pain in ≥4 of 5 regions, including left and right upper and lower regions and the axial region) must be present. Jaw, chest, and abdominal pain are not included in the generalized pain definition.
3) Symptoms have been generally present at a similar level for ≥3 months.
The new diagnostic criteria do not include a precise assessment of tender points (Figure 1) and do not take into consideration secondary FM, which may occur in patients with other rheumatologic disorders. A diagnosis of FM may be valid irrespective of other diagnoses and does not exclude the presence of other clinically important conditions. Unlike previous guidance regarding diagnosis, the new criteria have been standardized for both patients and health-care providers to encourage uniformity.
1. Rheumatologic diseases: Rheumatoid arthritis, systemic lupus erythematosus, polymyalgia rheumatica, myositis, myopathies, ankylosing spondylitis.
2. Neurologic disorders: Chronic neuropathic pain.
3. Endocrine disorders: Hypothyroidism.
TreatmentTop
Treatment of FM is primarily symptom-directed and is typically initiated stepwise, starting with nonpharmacologic interventions, including exercise and patient education. While practices vary significantly, the following treatment modalities are considered in recent practice guidelines:
1) Nonpharmacologic interventions: Low-impact aerobic and strengthening exercises are recommended. Supervised exercise or rehabilitation programs and referral to a physiatrist may be considered for patients having difficulty engaging in regular aerobic exercise. Other suggested treatments for patients with refractory symptoms include cognitive behavioral therapy (CBT), acupuncture and hydrotherapy, meditative movement therapies (yoga, tai chi, qigong), and mindfulness therapy. The European League Against Rheumatism (EULAR) guidelines suggested against the use of biofeedback, hypnotherapy, and massage therapy.
2) Pharmacologic interventions: Time-limited trials of low-dose pharmacologic treatments may be considered for severe pain (duloxetine, pregabalin, or tramadol) or severe insomnia (amitriptyline, cyclobenzaprine, and nighttime pregabalin). Those could be tried for several weeks: amitriptyline (dose as low as 10 mg/d),Evidence 1Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to imprecision and risk of bias and increased due to effect size. Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ. Amitriptyline for fibromyalgia in adults. Cochrane Database Syst Rev. 2015;7:CD011824. doi: 10.1002/14651858.CD011824. duloxetine (dose as low as 20 mg) or milnacipran (serotonin-norepinephrine reuptake inhibitors [SNRIs], dose as low as 100 mg/d), tramadol (dose as low as 37.5 mg/d, although recent concerns have been raised about its overall safety),Evidence 2Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to the observational nature of data. Zeng C, Dubreuil M, LaRochelle MR, et al. Association of Tramadol With All-Cause Mortality Among Patients With Osteoarthritis. JAMA. 2019 Mar 12;321(10):969-982. doi: 10.1001/jama.2019.1347. PubMed PMID: 30860559; PubMed Central PMCID: PMC6439672. pregabalin (dose as low as 25 mg/d), and cyclobenzaprine (dose as low as 10 mg/d). The EULAR guidelines issued a strong recommendation against the use of growth hormone and sodium oxybate and suggestions against the use of capsaicin, monoamine oxidase inhibitors, nonsteroidal anti-inflammatory drugs, glucocorticoids, and selective serotonin reuptake inhibitors (SSRIs). No recommendations were issued regarding cannabinoids and antipsychotics. Providers should be aware of the potential for adverse effects with all suggested pharmacologic alternatives.
FiguresTop
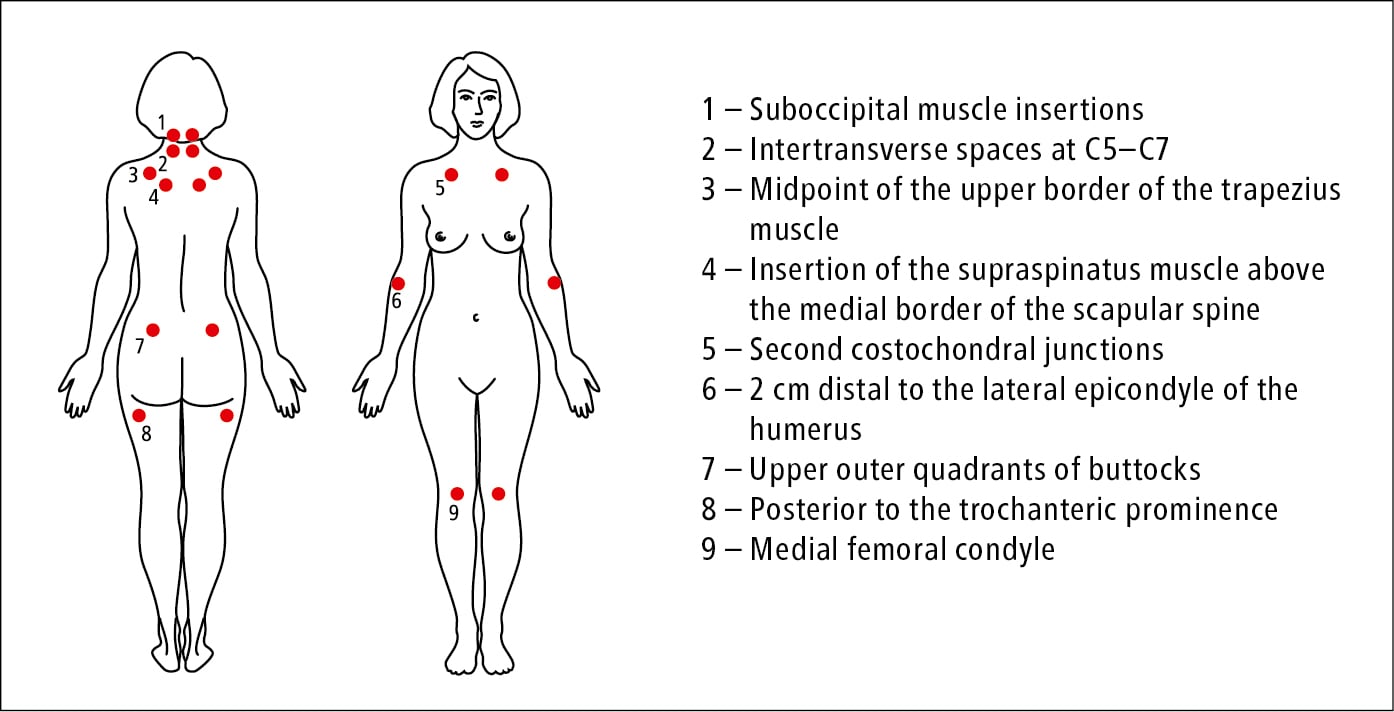
Figure 18.10-1. Tender points in fibromyalgia (no longer part of the diagnostic criteria).
AppendixTop
The widespread pain index (WPI) corresponds to the number of areas in which the patient had pain in the preceding week. Assessed areas include the left upper region (jaw, shoulder girdle, upper arm, lower arm), right upper region (jaw, shoulder girdle, upper arm, lower arm), left lower region (hip, upper leg, lower leg), right lower region (hip, upper leg, lower leg), and axial region (neck, upper back, lower back, chest, abdomen). Scores range from 0 to 19.
The symptom severity scale (SSS) takes into consideration:
1) The severity level of fatigue, waking unrefreshed, and cognitive symptoms, measured on a 0 to 3 scale.
2) The sum of headaches (0-1), pain or cramps in the lower abdomen (0-1), and depression (0-1) that the patient had in the previous 6 months.
The SSS is a sum of 1) and 2). The final score is between 0 and 12.