Vahanian A, Beyersdorf F, Praz F, et al; ESC/EACTS Scientific Document Group. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632. doi: 10.1093/eurheartj/ehab395. Erratum in: Eur Heart J. 2022 Feb 18;: PMID: 34453165.
Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e35-e71. doi: 10.1161/CIR.0000000000000932. Epub 2020 Dec 17. Erratum in: Circulation. 2021 Feb 2;143(5):e228. Erratum in: Circulation. 2021 Mar 9;143(10):e784. PMID: 33332149.Definition, Etiology, Pathogenesis Top
Tricuspid regurgitation (TR) is a reversal of blood flow from the right ventricle to the right atrium due to an incomplete closure of tricuspid valve leaflets. Patients with isolated TR (without tricuspid stenosis) usually have functional TR related to pulmonary hypertension (secondary or primary) or coexisting mitral valve disease, particularly stenosis.
Etiology:
1) Structural (organic) TR: Rheumatic fever, infective endocarditis, carcinoid syndrome, Marfan syndrome, Fabry disease, Whipple disease, tricuspid valve prolapse, rheumatoid arthritis, systemic lupus erythematosus, congenital heart disease (Ebstein anomaly and other conditions), papillary muscle dysfunction, drugs (methysergide, fenfluramine).
2) Functional TR (most frequent in patients with acquired valvular disease): Dilation of the tricuspid annulus of an anatomically normal valve secondary to the altered right ventricular geometry most commonly caused by pulmonary hypertension, mitral valve disease, right ventricular myocardial infarction, or congenital heart disease (eg, right ventricular outflow obstruction).
3) TR associated with intracardiac devices: Pacemaker and defibrillator leads can interfere with function of the tricuspid valve and lead to varying degrees of regurgitation, which may be progressive.
Clinical Features Top
Clinical features are usually dominated by symptoms of the coexisting pulmonary hypertension or mitral valve disease.
1. Symptoms: Reduced exercise tolerance, weakness, peripheral edema, right upper abdominal discomfort and distension.
2. Signs: Pulsation of significantly distended neck veins, a positive hepatojugular reflux; in patients with severe TR, pulsations of the vessels of the neck and head, less commonly pulsations of the eyes; right ventricular impulse; pulsations of the liver; in advanced TR, generalized subcutaneous edema, ascites, and cyanotic-yellowish color of the skin; a holosystolic murmur intensified during deep inspiration and diastolic rumble (in severe TR).
Diagnosis Top
1. Electrocardiography (ECG): P pulmonale, features of right ventricular hypertrophy, frequently incomplete right bundle branch block. Atrial fibrillation and atrial flutter are usually seen.
2. Chest radiography (Figure 1): In functional TR, the heart is significantly enlarged and includes a prominent right atrium; pleural effusion and distension of the azygos vein may be seen. Right ventricular enlargement in severe TR.
3. Echocardiography (Figure 2 and Figure 3) is used to assess the morphology of the tricuspid valve and severity of TR, as well as right ventricular systolic pressures (pressures >55 mm Hg suggest secondary TR). Significant TR with a normal tricuspid valve morphology may develop in patients with main pulmonary artery systolic pressures ≥55 mm Hg. TR in patients with pulmonary artery systolic pressures <40 mm Hg suggests structural valve abnormalities. In many healthy individuals, clinically irrelevant TR is seen.
Treatment Top
1. Medical therapy: Diuretics play a major role in symptomatic relief in patients with TR.
2. TR combined with mitral valve disease:
1) Surgical treatment of mitral stenosis alone may significantly reduce the severity of functional TR.
2) Surgical tricuspid valvuloplasty is indicated in patients with severe TR or dilation of the annulus (≥40 mm or >21 mm/m2) accompanied by mitral valve disease requiring surgery.
3) After left-sided valve surgery, tricuspid valve surgery may be considered in symptomatic patients with severe TR who have progressive right ventricular dilation or dysfunction in the absence of left-sided valve dysfunction, severe right or left ventricular dysfunction, and severe pulmonary vascular disease.
3. Severe symptomatic isolated primary TR without severe right ventricular dysfunction: Tricuspid valve repair; if not possible, tricuspid valve replacement is indicated.
4. Severe asymptomatic or mildly symptomatic isolated primary TR with progressive right ventricular dilation or deterioration of right ventricular function: Surgery should be considered.
5. TR with coexisting conduction disturbances: Implantation of an epicardial pacemaker during valve replacement surgery.
Recently developed transcatheter techniques have provided an alternative for patients with severe symptoms and prohibitive surgical risks. These patients should be evaluated in heart valve centers by a multidisciplinary team including surgeons, imaging specialists, and interventional cardiologists for eligibility.
Prognosis Top
Regardless of the underlying condition, severe TR is associated with a poor long-term prognosis due to the progressive right ventricular dysfunction and systemic venous congestion.
FiguresTop
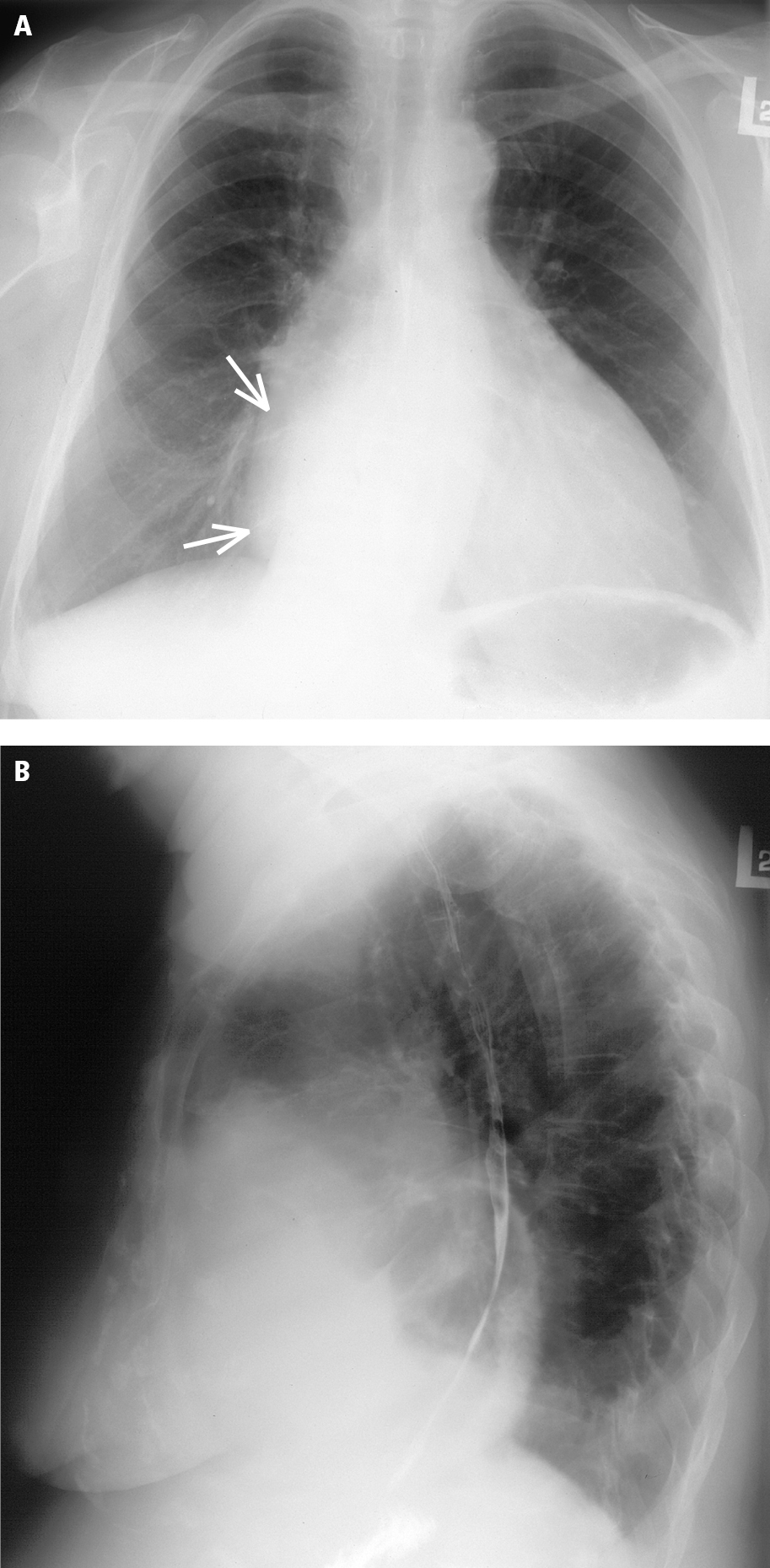
Figure 3.18-9. Chest radiography of a patient with combined tricuspid stenosis and regurgitation in the posteroanterior (PA) (A) and lateral (B) views: cardiomegaly, prominent right atrium (arrows); decreased pulmonary vascularity suggests reduced right ventricular output.
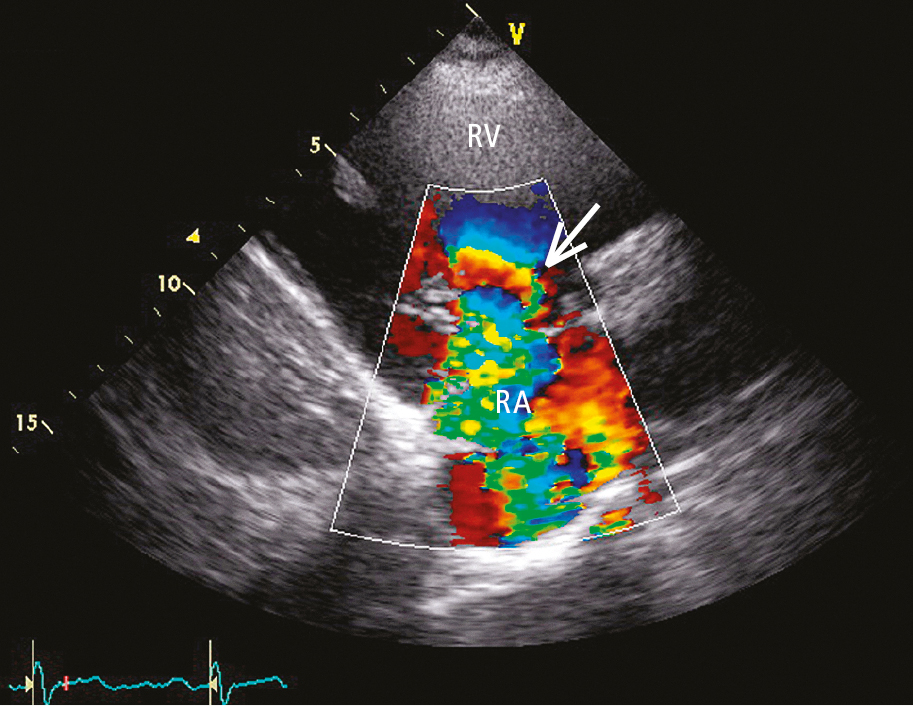
Figure 3.18-10. Transthoracic echocardiography (TTE) with color Doppler (parasternal view on the right ventricular inflow tract): severe tricuspid regurgitation (arrow). RA, right atrium; RV, right ventricle.
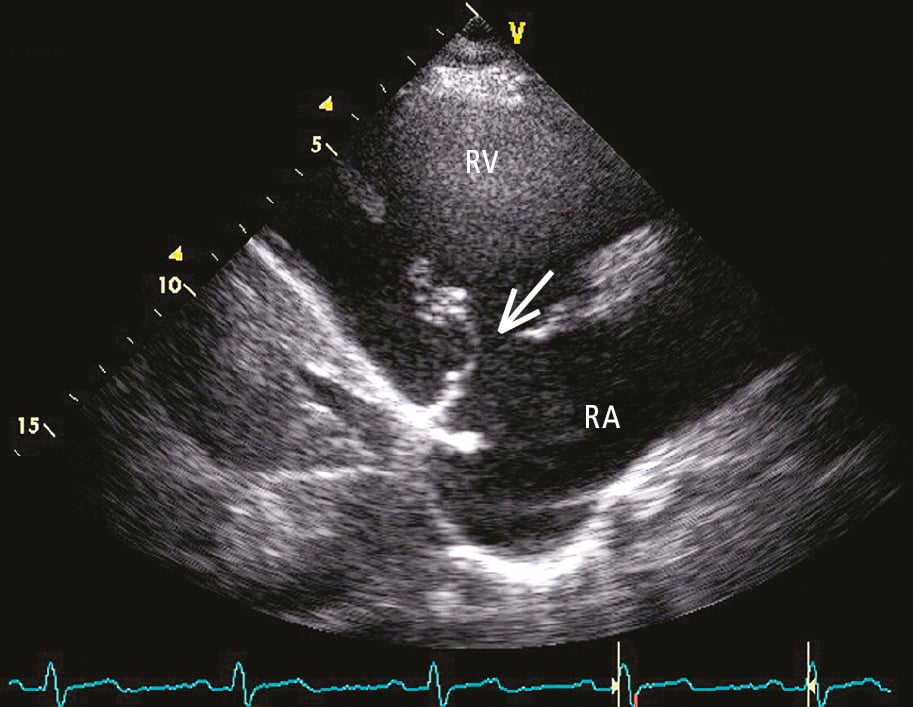
Figure 3.18-11. Transthoracic echocardiography (TTE) (parasternal view on the right ventricular inflow tract): no coaptation of the fibrotic tricuspid valve leaflets (arrow). RA, right atrium; RV, right ventricle.