Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022 May 3;79(17):e263-e421. doi: 10.1016/j.jacc.2021.12.012. Epub 2022 Apr 1. PMID: 35379503.
Bauersachs J, de Boer RA, Lindenfeld J, Bozkurt B. The year in cardiovascular medicine 2021: heart failure and cardiomyopathies. Eur Heart J. 2022 Feb 3;43(5):367-376. doi: 10.1093/eurheartj/ehab887. PMID: 34974611.
Gevaert AB, Kataria R, Zannad F, et al. Heart failure with preserved ejection fraction: recent concepts in diagnosis, mechanisms and management. Heart. 2022 Jan 12:heartjnl-2021-319605. doi: 10.1136/heartjnl-2021-319605. Epub ahead of print. PMID: 35022210.
Voors A. Empagliflozin in Patients Hospitalized for Acute Heart Failure – EMPULSE presented at: American Heart Association Virtual Annual Scientific Sessions (AHA 2021), November 14, 2021.
McDonagh TA, Metra M, Adamo M, et al; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-3726. doi: 10.1093/eurheartj/ehab368. Erratum in: Eur Heart J. 2021 Oct 14; PMID: 34447992.
Van Spall HGC, Averbuch T, Damman K, Voors AA. Risk and risk reduction in trials of heart failure with reduced ejection fraction: absolute or relative? Eur J Heart Fail. 2021 Sep;23(9):1437-1444. doi: 10.1002/ejhf.2248. Epub 2021 Jun 16. PMID: 34041823.
Jering KS, Claggett B, Pfeffer MA, et al. Prospective ARNI vs. ACE inhibitor trial to Determine Superiority in reducing heart failure Events after Myocardial Infarction (PARADISE-MI): design and baseline characteristics. Eur J Heart Fail. 2021 Jun;23(6):1040-1048. doi: 10.1002/ejhf.2191. PMID: 33847047.
McDonald M, Virani S, Chan M, et al. CCS/CHFS Heart Failure Guidelines Update: Defining a New Pharmacologic Standard of Care for Heart Failure With Reduced Ejection Fraction. Can J Cardiol. 2021 Apr;37(4):531-546. doi: 10.1016/j.cjca.2021.01.017. PMID: 33827756.
Tromp J, Ponikowski P, Salsali A, et al. Sodium-glucose co-transporter 2 inhibition in patients hospitalized for acute decompensated heart failure: rationale for and design of the EMPULSE trial. Eur J Heart Fail. 2021 May;23(5):826-834. doi: 10.1002/ejhf.2137. Epub 2021 Mar 10. PMID: 33609072; PMCID: PMC8358952.
Bozkurt B, Coats AJ, Tsutsui H, et al. Universal Definition and Classification of Heart Failure: A Report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J Card Fail. 2021 Mar 1;S1071-9164(21)00050-6. doi: 10.1016/j.cardfail.2021.01.022. Online ahead of print. PMID: 33663906.
Writing Committee; Maddox TM, Januzzi JL Jr, Allen LA, et al. 2021 Update to the 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment: Answers to 10 Pivotal Issues About Heart Failure With Reduced Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2021 Feb 16;77(6):772-810. doi: 10.1016/j.jacc.2020.11.022. PMID: 33446410.
Ponikowski P, Kirwan BA, Anker SD, et al; AFFIRM-AHF investigators. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double-blind, randomised, controlled trial. Lancet. 2020 Dec 12;396(10266):1895-1904. doi: 10.1016/S0140-6736(20)32339-4. Epub 2020 Nov 13. Erratum in: Lancet. 2021 Nov 27;398(10315):1964. PMID: 33197395.
Dewan P, Jackson A, Lam CSP, et al. Interactions between left ventricular ejection fraction, sex and effect of neurohumoral modulators in heart failure. Eur J Heart Fail. 2020;22(5):898-901. doi: 10.0.3.234/ejhf.1776. PMID: 32115864.
McMurray JJ V, Jackson AM, Lam CSP, et al. Effects of Sacubitril-Valsartan Versus Valsartan in Women Compared With Men With Heart Failure and Preserved Ejection Fraction: Insights From PARAGON-HF. Circulation. 2020;141(5):338-351.doi: 10.0.4.137/circulationaha.119.044491. PMID: 31736337.
Hollenberg SM, Warner Stevenson L, Ahmad T, et al. 2019 ACC Expert Consensus Decision Pathway on Risk Assessment, Management, and Clinical Trajectory of Patients Hospitalized With Heart Failure: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2019 Oct 15;74(15):1966-2011. doi: 10.1016/j.jacc.2019.08.001. Epub 2019 Sep 13. Erratum in: J Am Coll Cardiol. 2020 Jan 7;75(1):132. PMID: 31526538.
Kozhuharov N, Goudev A, Flores D, et al. Effect of a Strategy of Comprehensive Vasodilation vs Usual Care on Mortality and Heart Failure Rehospitalization Among Patients With Acute Heart Failure: The GALACTIC Randomized Clinical Trial. JAMA. 2019 Dec 17;322(23):2292-2302. doi: 10.1001/jama.2019.18598. PMID: 31846016; PMCID: PMC6990838.
Van Spall HGC, Lee SF, Xie F, et al. Effect of Patient-Centered Transitional Care Services on Clinical Outcomes in Patients Hospitalized for Heart Failure: The PACT-HF Randomized Clinical Trial. JAMA. 2019;321(8):753–761. doi:10.1001/jama.2019.0710.
Velazquez EJ, Morrow DA, DeVore AD, et al; PIONEER-HF Investigators. Angiotensin-Neprilysin Inhibition in Acute Decompensated Heart Failure. N Engl J Med. 2019 Feb 7;380(6):539-548. doi: 10.1056/NEJMoa1812851. Epub 2018 Nov 11. Erratum in: N Engl J Med. 2019 Mar 14;380(11):1090. PMID: 30415601.
Pfeffer MA, Shah AM, Borlaug BA. Heart Failure With Preserved Ejection Fraction In Perspective. Circ Res. 2019;124(11):1598-1617. doi: 10.0.4.137/circresaha.119.313572. PMID: 31120821; PMCID: PMC6534165.
Seferović PM, Polovina M, Bauersachs J, et al. Heart failure in cardiomyopathies: a position paper from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21(5):553-576. doi: 10.1002/ejhf.1461. PMID: 30989768.
Yancy CW, Januzzi JL Jr, Allen LA, et al. 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment: Answers to 10 Pivotal Issues About Heart Failure With Reduced Ejection Fraction. J Am Coll Cardiol. 2018 Jan 16;71(2):201-230. doi: 10.1016/j.jacc.2017.11.025. PMID: 29277252.
Van Spall HGC, Rahman T, Mytton O, et al. Comparative effectiveness of transitional care services in patients discharged from the hospital with heart failure: a systematic review and network meta-analysis. Eur J Heart Fail. 2017 Nov;19(11):1427-1443. doi: 10.1002/ejhf.765. Epub 2017 Feb 24. PMID: 28233442.
Yancy CW, Jessup M, Bozkurt B, Butler J, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017 Aug 8;136(6):e137-e161. doi: 10.1161/CIR.0000000000000509. Epub 2017 Apr 28. PMID: 28455343.
Etiology and PathogenesisTop
Acute heart failure (AHF) is defined as a severe onset of signs and symptoms of heart failure (HF) requiring medical attention and resulting in urgent hospitalization or an emergency department visit.
AHF may develop de novo, that is, in a person without prior documented heart dysfunction, or as acute decompensation of prior HF.
Patients with AHF should be urgently assessed and started on appropriate medical therapies.
Causes of AHF: Acute coronary syndrome (ACS), mechanical complications of myocardial infarction (MI), acute valvular regurgitation, markedly elevated blood pressure (BP), arrhythmia or conduction disturbances, peripartum cardiomyopathy, cardiac surgical complications, infections (including myocarditis and infective endocarditis), endocrinopathy, high cardiac output states (severe infection [particularly sepsis], thyroid storm, anemia, arteriovenous fistula, Paget disease), nonadherence to medications.
Ischemic heart disease and long-standing poorly controlled hypertension are the most common causes of AHF, especially in the elderly. Predominant etiologies in young patients include dilated cardiomyopathy, arrhythmia, congenital heart disease, valvular heart disease, and myocarditis.
Clinical Features and Natural HistoryTop
Signs and symptoms:
1) Features of low cardiac output (hypoperfusion) if cardiogenic shock is present: Fatigue; weakness; confusion; drowsiness; pale, cool, and moist extremities, occasionally with peripheral cyanosis; thready pulse; hypotension; oliguria.
2) Congestion:
a) In systemic circulation (right ventricular failure): Peripheral edema (ankle or sacral pitting edema; this may be absent in early AHF); jugular vein distention; epigastric tenderness (caused by liver enlargement); sometimes ascites and pleural and/or pericardial effusions.
b) In pulmonary circulation (left ventricular [LV] failure, which may lead to pulmonary edema): Dyspnea, tachypnea and orthopnea, crackles over lungs.
3) Features of the underlying condition causing AHF.
Based on the features of peripheral hypoperfusion, the patient may be classified as “cold” (with hypoperfusion) or “warm” (without hypoperfusion), and based on the features of pulmonary congestion, as “wet” (with congestion) or “dry” (without congestion).
DiagnosisTop
Diagnosis is made based on signs and symptoms as well as the results of diagnostic tests.
1. Electrocardiography (ECG) usually reveals abnormalities corresponding to the underlying condition, which most frequently are features of myocardial ischemia, arrhythmia, or conduction abnormalities.
2. Chest radiography and lung ultrasound imaging: In addition to features of the underlying condition, they may reveal pulmonary congestion, pleural effusions, and cardiac enlargement. Bilateral prominent B lines may indicate cardiogenic pulmonary edema.
3. Echocardiography reveals cardiac abnormalities, which may be functional (systolic or diastolic myocardial dysfunction, valvular dysfunction) or anatomical (eg, mechanical complications of MI).
4. Laboratory tests: The basic set of tests includes complete blood count; serum levels of creatinine, urea/blood urea nitrogen, sodium, potassium, glucose, cardiac troponin, and liver enzymes; arterial blood gas levels (in patients with mild dyspnea, pulse oximetry may be used, with the exception of patients with shock causing very low cardiac output and peripheral vasoconstriction). Natriuretic peptide levels (B-type natriuretic peptide [BNP]/N-terminal pro–B-type natriuretic peptide [NT-proBNP]) can be useful in differentiating between cardiogenic (higher levels) and noncardiogenic causes of dyspnea. Causes of high-output HF including endocrinopathies should also be considered in the workup, as they may precipitate AHF.
5. Endomyocardial biopsy has a limited role, except in fulminant myocarditis. Indications: see Chronic Heart Failure.
Other causes of dyspnea and edema. Consider also causes of noncardiogenic pulmonary edema (features facilitating differentiation between noncardiogenic and cardiogenic pulmonary edema: Table 1), acute respiratory failure, and (acute) interstitial lung disease.
TreatmentTop
Admissions for HF represent an opportunity to make a diagnosis, modify clinical trajectory, and improve outcomes following hospitalization. Ideally patients with HF should undergo continuous reassessment during admission and should be categorized into one of the following: (1) improving towards target goals, (2) stalled after an initial response, or (3) worsening or not improved.
These trajectories should guide inpatient management and the target goal of decongestion, as indicated by improvement in symptoms and radiologic images, a decrease in biomarker concentration (natriuretic peptides), and a decrease in weight.
1. Short-term treatment goals: Hemodynamic stabilization, decongestion, control of symptoms (primarily of dyspnea), and hemodynamic stabilization of the patient.
2. Treatment of the underlying condition and risk factors.
3. Management of cardiac and noncardiac comorbidities such as dysrhythmias, valve disease, diabetes, hypertension, kidney disease, pulmonary disease, substance misuse, and tobacco use. Ideally the management of comorbidities should be optimized while the patient is in the hospital.
4. Close monitoring of respiratory rate, heart rate, ECG, and BP. Measure these parameters regularly (eg, every 5-10 minutes) or continuously (in unstable patients) until the patient’s condition is stable and drug doses need no further adjustment. Noninvasive automated BP monitors are reliable if there is no severe vasoconstriction or significant tachycardia. ECG monitoring is important in AHF, particularly when caused by ACS or arrhythmia. In patients treated with oxygen, monitor hemoglobin oxygen saturation using a pulse oximeter regularly (eg, every hour) or continuously (preferable approach).
Occasionally invasive hemodynamic monitoring is necessary, particularly in patients with concomitant congestion, hypoperfusion, and a poor response to pharmacotherapy. It may be helpful in selecting appropriate therapy. Note that the influence of these devices on survival is unclear. In selected scenarios, the following devices may be considered:
1) A Swan-Ganz catheter placed in the main pulmonary artery allows measurement of pressures in the superior vena cava, right atrium, right ventricle, main pulmonary artery, as well as pulmonary capillary wedge pressure, cardiac output (see Shock), and oxygen saturation of mixed venous blood; the use is limited, markedly less common than in the past, and not supported by high-quality evidence.
2) A central venous catheter is used to measure central venous pressure and oxygen saturation of the venous blood (SvO2) in the superior vena cava or in the right atrium and may be helpful in certain cases.
3) A peripheral arterial catheter (usually placed in the radial artery) is used for continuous BP monitoring in shock states.
5. Medication classes that are efficacious in reducing cardiovascular (CV) or all-cause death and HF hospitalizations in patients with HF with reduced ejection fraction (HFrEF) have been less efficacious at higher ranges of left ventricular ejection fraction (LVEF) but are indicated to decrease the risk of HF hospitalization.
6. Treatment of specific types of AHF:
1) Worsening or decompensation of HF: In selected patients there may be a role for vasodilators in combination with IV loop diuretics. Diuretic infusions may facilitate decongestion when patients do not respond to bolus IV doses. Use inotropic agents in patients with hypotension and features of organ hypoperfusion.
There is no evidence to support aggressive vasodilation compared with routine use of guideline-informed therapies. Recent comparison of standard care with rapid, intensive, sustained IV vasodilators did not demonstrate reductions in all-cause mortality or HF hospitalization. Presently there are no recommendations that can be given to favor one regimen over the other.Evidence 1Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to indirectness. Kozhuharov N, Goudev A, Flores D, et al. Effect of a Strategy of Comprehensive Vasodilation vs Usual Care on Mortality and Heart Failure Rehospitalization Among Patients With Acute Heart Failure: The GALACTIC Randomized Clinical Trial. JAMA. 2019 Dec 17;322(23):2292-2302. doi: 10.1001/jama.2019.18598. PMID: 31846016; PMCID: PMC6990838.
2) Pulmonary edema: Figure 1.
3) AHF with hypertensive emergency: Vasodilators (close monitoring is necessary) and/or loop diuretics may be considered in addition to guideline recommendations for hypertensive emergency.
4) Cardiogenic shock: Identification and management of the underlying etiology (eg, ischemia, arrhythmia), maintaining hemodynamics, and preventing organ dysfunction. In patients with hypoxemia consider oxygen, inotropes, and/or short-term mechanical circulatory support if there is no improvement.
5) Isolated right ventricular AHF: Maintain right ventricular preload. If possible, avoid vasodilators (opiates, nitrates, angiotensin-converting enzyme inhibitors [ACEIs], angiotensin receptor blockers [ARBs]) and diuretics. Cautious administration of intravenous fluids may be effective (with careful hemodynamic monitoring). Low-dose dopamine is sometimes used. Consider inotropes, noradrenaline, or both in patients with low cardiac output and those hemodynamically unstable.
6) AHF in the course of ACS: Perform echocardiography to determine the cause of AHF. In patients with ST-segment elevation MI or non–ST-segment elevation MI, perform coronary angiography and revascularization. In patients with mechanical complications of acute MI, urgent surgical treatment is necessary.
1. Vasodilators may be used in patients with features of hypoperfusion and congestion but without hypotension. There is no high-quality evidence to support early aggressive vasodilation over routine oral HF therapies.Evidence 2Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to indirectness. Kozhuharov N, Goudev A, Flores D, et al. Effect of a Strategy of Comprehensive Vasodilation vs Usual Care on Mortality and Heart Failure Rehospitalization Among Patients With Acute Heart Failure: The GALACTIC Randomized Clinical Trial. JAMA. 2019 Dec 17;322(23):2292-2302. doi: 10.1001/jama.2019.18598. PMID: 31846016; PMCID: PMC6990838. They are generally avoided in patients with systolic blood pressure (SBP) <110 mm Hg. Vasodilators lower SBP, left and right ventricular filling pressures, as well as peripheral vascular resistance while improving dyspnea. BP monitoring is mandatory. Use vasodilators with caution in patients with mitral or aortic stenosis.
1) IV nitroglycerin: Start with 10 to 20 microg/min and increase the dose as needed by 5 to 10 microg/min every 3 to 5 minutes up to the maximal hemodynamically tolerated dose (maximum, 200 microg/min); alternatively, nitroglycerin may be administered orally or in the form of translingual spray at a dose of 400 microg every 5 to 10 minutes. Because tolerance develops after 24 to 48 hours of treatment with high-dose nitroglycerin, the drug should be used intermittently. In case of BP dropping <90 mm Hg, reduce the dose of nitroglycerin. If BP continues to fall, discontinue the infusion.
2) IV sodium nitroprusside: Start with 0.3 microg/kg/min, up to a maximum dose of 5 microg/kg/min. Nitroprusside is recommended in patients with severe AHF in the course of hypertension and in patients with AHF caused by mitral insufficiency. Do not use nitroprusside in patients with AHF in the course of ACS, as it may cause a coronary steal effect. In patients receiving long-term treatment with nitroprusside, particularly patients with severe kidney or liver failure, toxicity caused by its metabolites—thiocyanate and cyanide—may occur (abdominal pain, confusion, seizures).
2. Diuretics are mainly used in patients with AHF and features of volume overload, that is, pulmonary congestion or peripheral edema. Diuretics do not prevent disease progression, and high doses of diuretics may cause a transient deterioration in kidney function. Budesonide and torsemide have better bioavailability than the commonly used furosemide. Algorithm of diuretic treatment in patients with AHF: Figure 2. In patients treated with diuretics, monitor urine output (catheterization may be necessary); adjust the dose of diuretics to the clinical response; restrict sodium intake; monitor serum creatinine, potassium, and sodium levels every 1 to 2 days, depending on the urine output; and correct for potassium and magnesium loss.
Transitioning from IV to oral diuretics is an important step in therapy and should be initiated once the patient is stable. Ideally the intended discharge diuretic regimen should be maintained with evidence of response for ≥24 to 48 hours prior to discharge. This has been associated with a clinically significant reduction in mortality at 30 and 90 days following discharge.
3. Inotropes may be used in patients with AHF associated with peripheral hypoperfusion and hypotension (SBP <85 mm Hg) who have not responded to standard treatment. Monitor ECG because of the risk of tachycardia, myocardial ischemia, and arrhythmia. Agents and dosage: see Table 4 in Chronic Heart Failure.
4. Vasopressors are considered in patients with persistent hypotension and hypoperfusion despite appropriate volume status. Agents and dosage: see Table 4 in Chronic Heart Failure.
5. Other agents:
1) Amiodarone is the only antiarrhythmic agent with no negative inotropic effects and not causing significant hypotension. It is effective acutely in most types of supraventricular and ventricular arrhythmia.
2) In patients with HF receiving long-term treatment with beta-blockers who are hospitalized due to HF exacerbation, the beta-blockers generally should be continued unless cardiogenic shock is present. In patients with bradycardia or symptomatic hypotension, reduce the dose of the beta-blocker. If the beta-blocker has been discontinued, resume the treatment once the patient is hemodynamically stable.
3) In patients receiving long-term ACEI/ARB/angiotensin receptor–neprilysin inhibitor (ARNI) treatment, these agents should not be withheld unless unavoidable (eg, in a patient with shock or acute kidney injury). For patients not receiving these therapies, start the treatment before discharge. ARNIs can be started during hospitalization (instead of ACEI/ARB) in patients with HFrEF who are not already treated with these agents (see Chronic Heart Failure). Assess kidney function and serum potassium levels before and following initiation.
4) Add a mineralocorticoid receptor antagonist (MRA) in patients with no contraindications. The role for this class has been established in chronic HFrEF, in post-MI HFrEF, and in HF with preserved ejection fraction (HFpEF). Assess renal function and serum potassium levels before and following initiation.
5) Add a sodium-glucose cotransporter-2 (SGLT-2) inhibitor in hemodynamically stable patients. The benefit for this class has been established in HF across the LVEF spectrum, including among patients hospitalized for HF (see Chronic Heart Failure).
6) IV iron administered to patients stabilized following an AHF episode who have iron deficiency is associated with reduced HF hospitalizations. Consider initiating IV ferric carboxymaltose in patients with an LVEF <50%, serum ferritin <100 ng/mL, or serum ferritin of 100 to 299 ng/mL with transferrin saturation <20%.Evidence 3Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to imprecision and indirectness. Ponikowski P, Kirwan BA, Anker SD, et al; AFFIRM-AHF investigators. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double-blind, randomised, controlled trial. Lancet. 2020 Dec 12;396(10266):1895-1904. doi: 10.1016/S0140-6736(20)32339-4. Epub 2020 Nov 13. Erratum in: Lancet. 2021 Nov 27;398(10315):1964. PMID: 33197395.
7) Opiates are not recommended for routine use given their association with prolonged hospitalization and increased mortality, unless in patients demonstrating severe anxiety or intractable pain.
1. Ventilatory support: Consider this in patients with persistent SaO2 <90% despite maintained airway and oxygen treatment. Generally start with noninvasive support (continuous positive airway pressure [CPAP], bilevel positive airway pressure [BiPAP]), but invasive support may also be needed if patients experience prohibitive work of breathing or difficult-to-control hypoxia (see Respiratory Support).
2. Circulatory support, such as extracorporeal membrane oxygenation (ECMO) or Impella pump, may be considered in patients with AHF resistant to pharmacologic treatment (except for those with increased cardiac output). There is no evidence from randomized control trials to support ECMO or Impella in acute cardiogenic shock. This may be considered if improvement in cardiac function is expected or as a bridging therapy before heart transplant or another intervention that may restore cardiac function (see Mechanical Circulatory Support).
Indications:
1) Multivessel ischemic heart disease causing severe myocardial ischemia.
2) Acute mechanical complications of MI.
3) Acute mitral or aortic regurgitation caused by endocarditis, trauma, or aortic dissection (in the case of aortic insufficiency).
4) Some complications of percutaneous coronary intervention.
Transition care that closes gaps during the transition from hospital to home, a high-risk period, may improve outcomes. Postdischarge visits should focus on reassessing clinical trajectories, optimizing HF medications, monitoring for adverse effects or pharmacotherapies, addressing comorbidities, and modifying possible risk factors. Ideally the visit should occur within 7 to 14 days following discharge (see Chronic Heart Failure). A review of indications and the use of medications, including diuretics, beta-blockers, MRAs, SGLT-2 inhibitors, and ARB/ACEI/ARNI should be performed. There is high-quality evidence that multidisciplinary HF clinics and nurse home visits improve clinical and patient-reported outcomes, including quality of life, following hospitalization for HF.
Special ConsiderationsTop
1. Prosthetic valve thrombosis is often fatal. If this is suspected, perform echocardiography immediately.
1) In patients with a thrombosed prosthetic pulmonary or tricuspid valve or at high surgical risk, use fibrinolytic agents: alteplase (10 mg IV bolus followed by an IV infusion of 90 mg over 90 minutes) or streptokinase (250,000-500,000 IU administered IV over 20 minutes followed by an IV infusion of 1-1.5 million IU over 10 hours and then by unfractionated heparin treatment).
2) In patients with a thrombosed prosthetic mitral or aortic valve, the preferred treatment is valve replacement.
2. Acute kidney injury in the course of AHF leads to nonrespiratory acidosis and electrolyte disturbances that may cause arrhythmia, reduce the effectiveness of treatment, and affect the prognosis. Moderate to severe renal failure (serum creatinine levels >190 micromol/L [2.5 mg/dL]) is associated with an impaired response to diuretics. In patients with persistent volume overload despite appropriate pharmacotherapy, consider continuous venous hemofiltration with ultrafiltration.
3. Consider a palliative care approach/consultation if the patient’s clinical trajectory is unfavorable and if further discussion surrounding prognosis and management is needed with the patient and their family.
Tables and FiguresTop
|
Clinical features |
Pulmonary edema | |
|
Cardiogenic |
Noncardiogenic | |
|
Skin (extremities) |
Cold |
Usually warm |
|
Gallop |
Present |
Usually absent |
|
Electrocardiography |
Features of myocardial ischemia or myocardial infarction |
Usually normal |
|
Chest radiography |
Hilar pulmonary venous congestion and edema |
Initially peripheral pulmonary venous congestion and edema |
|
Blood levels of cardiac troponins |
May be increased |
Usually normal |
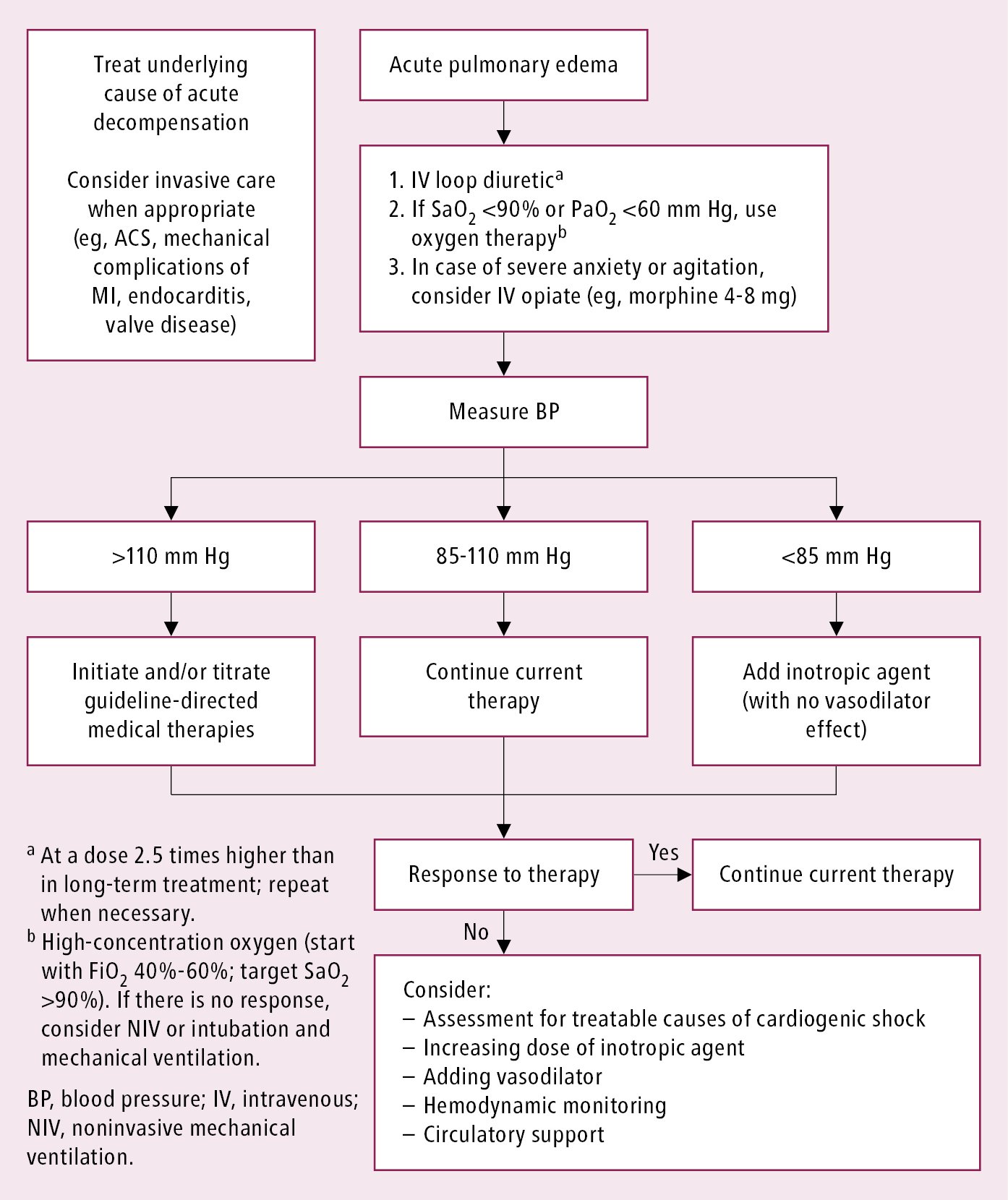
Figure 3.8-1. Management algorithm in patients with acute pulmonary edema. Based on Eur J Heart Fail. 2016;18(8):891-975.
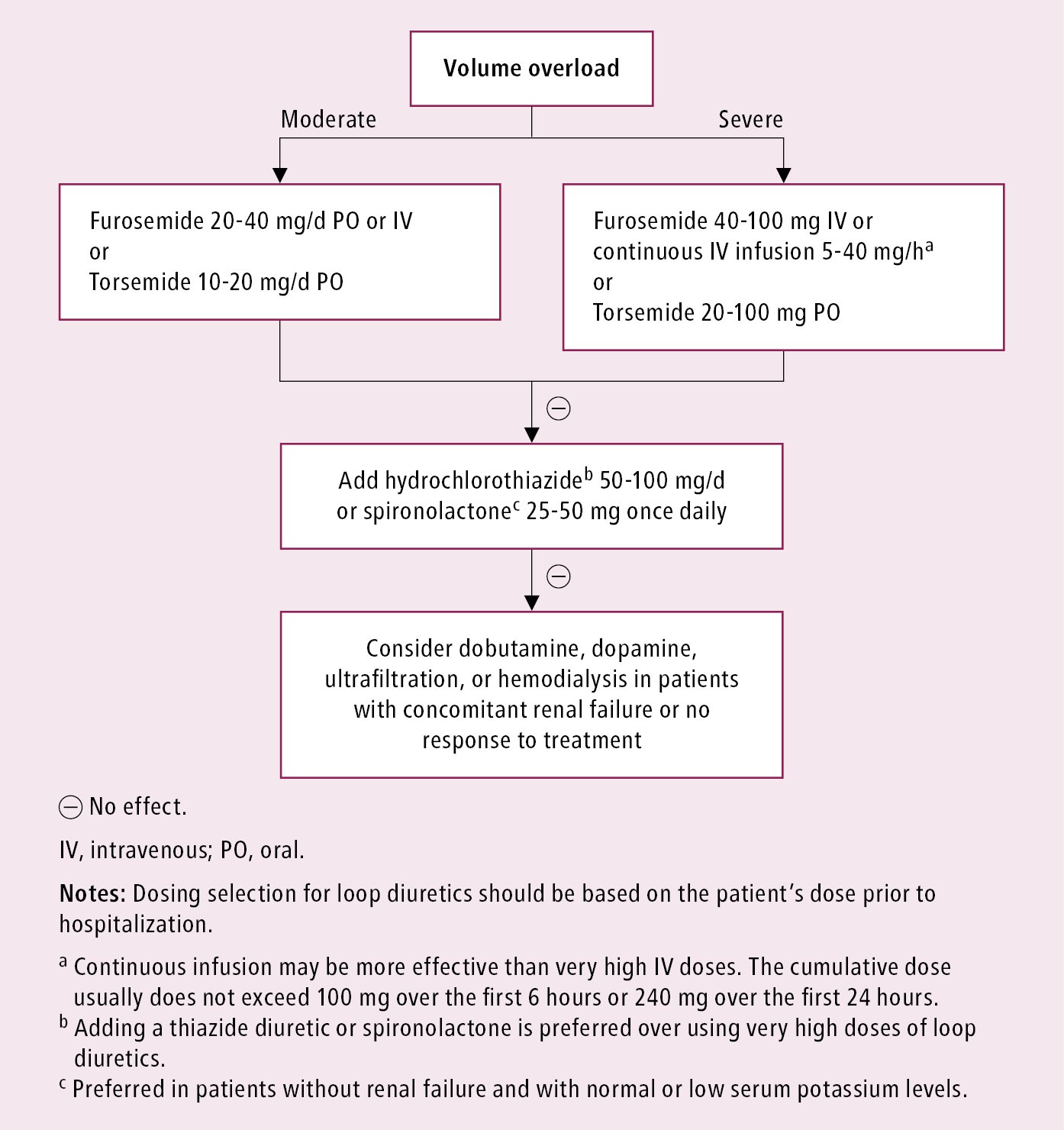
Figure 3.8-2. Algorithm of diuretic therapy in patients with acute heart failure. Based on Eur J Heart Fail. 2016;18(8):891-975.