MacDuff A, Arnold A, Harvey J; BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010 Aug;65 Suppl 2:ii18-31. doi: 10.1136/thx.2010.136986. PubMed PMID: 20696690.
Baumann MH, Strange C, Heffner JE, et al; AACP Pneumothorax Consensus Group. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001 Feb;119(2):590-602. Review. PubMed PMID: 11171742.
Definition, Etiology, PathogenesisTop
Pneumothorax is the presence of air in the pleural space. The air enters the pleural space as a result of damage to the visceral pleura or parietal pleura, causing positive intrapleural pressure and compressing the lung. This in turn leads to impairment of gas exchange. Classification:
1) Based on the cause:
a) Spontaneous pneumothorax is likely caused by rupture of an emphysematous bulla or subpleural alveoli. It may be primary (in previously healthy patients, ie, without any features of lung disease) or secondary (in the course of pulmonary diseases such as chronic obstructive pulmonary disease, cystic fibrosis, pulmonary Langerhans cell histiocytosis, or lymphangioleiomyomatosis).
b) Traumatic pneumothorax is caused by chest trauma, both penetrating and nonpenetrating (stab wounds with a sharp object, fall from height, crush wounds, traffic accidents).
c) Iatrogenic pneumothorax following thoracentesis, lung biopsy (percutaneous or transbronchial), catheterization of the large veins (a subclavian vein, less commonly an internal jugular vein), mechanical ventilation, or thoracic surgery.
2) Based on the mechanism:
a) Closed pneumothorax: A certain amount of air enters the pleural space and may be absorbed spontaneously after a few days (eg, as in the case of iatrogenic pneumothorax caused by thoracentesis).
b) Open pneumothorax: Air passes into the pleural space through a hole in the chest and leaves it unrestricted. This may cause shifting of the mediastinum to the contralateral side, which in turn may lead to tension pneumothorax and cardiac arrest.
c) Tension pneumothorax: A one-way valve is formed in a hole through which air flows into the pleural space. During each inspiration air enters the pleural space but cannot leave it during expiration. As a consequence, the intrapleural pressure exceeds the atmospheric pressure and is constantly increasing, thereby causing not only ipsilateral compression of the lung but also contralateral displacement of the mediastinum, compression of the contralateral lung, compression of the large veins, decrease in the venous return, and reduction in cardiac output. These changes lead to sudden hypotension, hypoxemia, and potentially cardiac arrest. Tension pneumothorax is a life-threatening condition that requires immediate intervention.
3) Based on the size (pneumothorax diameter, ie, the distance between the chest wall and visceral pleura [lung margin] at the level of the pulmonary hilum on anteroposterior [AP] chest radiographs):
a) Small pneumothorax (<2 cm).
b) Large pneumothorax (≥2 cm).
Clinical Features and Natural HistoryTop
The most common symptoms of pneumothorax are dyspnea, pleuritic chest pain, and cough, although some patients are asymptomatic. Signs (see Respiratory Sounds) may be minor and include silent lung sounds, hypertympany on percussion on the side of the pneumothorax, or tracheal displacement to the contralateral side. Tension pneumothorax is usually accompanied by rapidly progressive dyspnea, hypotension, signs of hypoxemia (cyanosis, tachypnea, tachycardia), and in the event of further worsening of the pneumothorax also cardiac arrest. Pneumothorax may be accompanied by subcutaneous emphysema and pneumomediastinum.
DiagnosisTop
Diagnosis is suggested by the patient’s history and physical examination and confirmed with imaging studies. The size of a pneumothorax cannot be accurately estimated on the basis of signs and symptoms.
1. Imaging studies:
1) Chest radiographs demonstrate displacement of the lung edge away from the chest wall (Figure 1).
2) Computed tomography (CT) of the chest is helpful in differentiating pneumothorax from an emphysematous bulla, especially in the setting of subcutaneous emphysema. Clinical data support the use of chest CT in the evaluation of incident pneumothorax to identify secondary causes (predisposing factors).Evidence 1Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to the observational nature of data. Phillips GD, Trotman-Dickenson B, Hodson ME, Geddes DM. Role of CT in the management of pneumothorax in patients with complex cystic lung disease. Chest. 1997 Jul;112(1):275-8. PubMed PMID: 9228391.
3) Ultrasonography (using a 5-10 MHz probe placed in the midclavicular and anterior axillary lines): The findings of pleural sliding with respiration and the comet tail sign (a longitudinal artifact observed at the border of normal adherence of the layers of pleura in B-mode ultrasonography) exclude pneumothorax. In M-mode ultrasonography the normal lung shows a “seashore sign,” which is a combination of a superficial layer of horizontal lines from the static chest wall and a deep layer of granular pattern caused by lung movement, while a pneumothorax shows a “barcode sign” or “stratosphere sign” (Figure 2).
2. Pulse oximetry and arterial blood gas measurements may reveal decreased oxygen saturation (SpO2) and hypoxemia (particularly in patients with a tension pneumothorax or large pneumothorax). In some cases hypercapnia and respiratory acidosis are seen (particularly in secondary pneumothorax).
TreatmentTop
Management of Life-Threatening Pneumothorax
Administer oxygen in all patients (see Oxygen Therapy).
1. Tension pneumothorax: Immediately insert a catheter 4 to 5 cm long, 2 mm (14 gauge) or 1.7 mm (16 gauge) in diameter (as for a peripheral IV line) through the second intercostal space in the midclavicular line, along the upper edge of the third rib, into the pleural space. Leave it in place until a definitive drain is placed using traditional chest tube insertion or pig-tail catheterization.
2. Bilateral pneumothorax: Perform pleural drainage as required, starting from the larger pneumothorax. Usually this necessitates a higher level of care and observation than unilateral pneumothorax.
3. Pneumothorax with hemothorax requires urgent drainage or surgery.
Management of Non–Life-Threatening Pneumothorax
1. Primary spontaneous pneumothorax: Management algorithm: Figure 3.
1) Observation: Observation is appropriate for patients with a small closed iatrogenic pneumothorax or primary spontaneous pneumothorax and with mild symptoms. You may consider outpatient treatment if a follow-up chest radiograph performed after 3 to 6 hours does not show an increase in the size of the pneumothorax; however, the patient should be asked to immediately report to the hospital in case of worsening symptoms and should be informed about the risk of recurrence. Other patients require hospitalization. If there are no contraindications (eg, due to chronic hypercarbic respiratory failure), administer oxygen at the rate of 10 L/min (see Oxygen Therapy); this promotes reabsorption of air from the pleural space. Perform follow-up chest radiographs and reassess the need for hospitalization.
2) Syringe aspiration through a catheter: This may be used in primary spontaneous and iatrogenic pneumothorax.Evidence 2Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to the risk of bias and imprecision. Carson-Chahhoud KV, Wakai A, van Agteren JE, et al. Simple aspiration versus intercostal tube drainage for primary spontaneous pneumothorax in adults. Cochrane Database Syst Rev. 2017 Sep 7;9:CD004479. doi: 10.1002/14651858.CD004479.pub3. Review. PubMed PMID: 28881006; PubMed Central PMCID: PMC6483783. After thoracentesis (as in pleural fluid collection) and inserting the catheter, remove up to 2.5 L of air from the pleural space using a syringe connected to the catheter via a 3-way stopcock. In case of ineffective aspiration (defined as removal of >2.5 L of air, persistent breathlessness, or large pneumothorax on follow-up chest radiographs), perform pleural drainage; aspiration may be repeated only in patients in whom no technical difficulties were encountered during the procedure. In the case of secondary spontaneous pneumothorax, this technique may be used only in patients with mild dyspnea and a small pneumothorax. Aspiration through a catheter is not recommended in patients with recurrent pneumothorax.
3) Pleural drainage through the intercostal space: Connect a drainage tube inserted into the pleural space to a 3-chamber drainage set and leave it until complete expansion of the lung or cessation of air leakage. If despite the drainage the lung does not expand, a high-volume low-pressure suction system may be applied to the drainage system.
4) Surgical treatment:
a) Indications: Second episode of spontaneous ipsilateral pneumothorax; recurrence of pneumothorax on the contralateral side of the chest; bilateral spontaneous pneumothorax; persistent air leakage or incomplete expansion of the lung after >5 days of pleural drainage; hemothorax; occupations associated with an increased risk of pneumothorax (divers, pilots, professional drivers, train engineers, sailors, deep sea fishermen, glass factory workers, wind instrument players); cystic fibrosis (consider surgery after the first episode of pneumothorax).
b) Types of procedures: Pleurodesis (usually with the use of talc, which leads to obliteration of the pleural space), optimally in combination with videothoracoscopy; pulmonary wedge resection and pleurectomy (complete resection of the parietal pleura that leads to permanent obliteration of the pleural space and almost completely prevents recurrence of pneumothorax).
5) Recommendations for patients with a history of pneumothorax: Airlines recommend a 6-week interval between complete resolution of pneumothorax and air travel. A history of spontaneous pneumothorax is a permanent contraindication to diving (except for patients undergoing pleurectomy). Cessation of smoking reduces the risk of recurrent pneumothorax.
2. Management algorithm in secondary spontaneous pneumothorax:
1) Hospitalization and supplemental oxygen: All patients with secondary spontaneous pneumothorax should be considered for close observation with supplemental oxygen (see above). Asymptomatic patients with a pneumothorax <1 cm on AP chest radiographs may not require further active interventions.
2) Drainage: Needle aspiration may be tried in patients with mild symptoms and a small pneumothorax (<2 cm on AP chest radiographs) to avoid chest drain insertion. Otherwise, placement of a small-bore chest drain is recommended.
3) Specialist consultation: All patients with secondary spontaneous pneumothorax require early referral for evaluation and consideration of specialized definitive management. Patients with persistent air leak after 48 hours of chest drain insertion should be referred to a thoracic surgeon.
FiguresTop
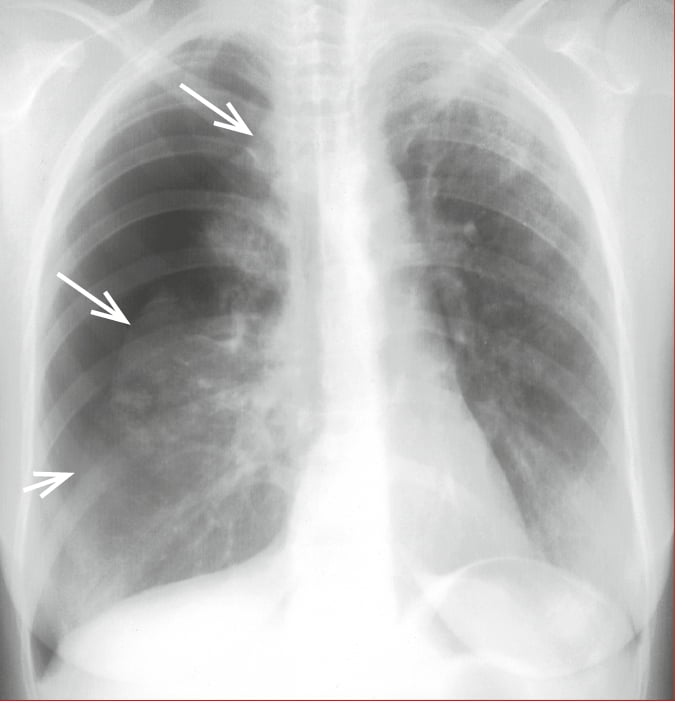
Figure 17.16-7. Large (≥2 cm) pneumothorax (arrows indicate the lung margin).
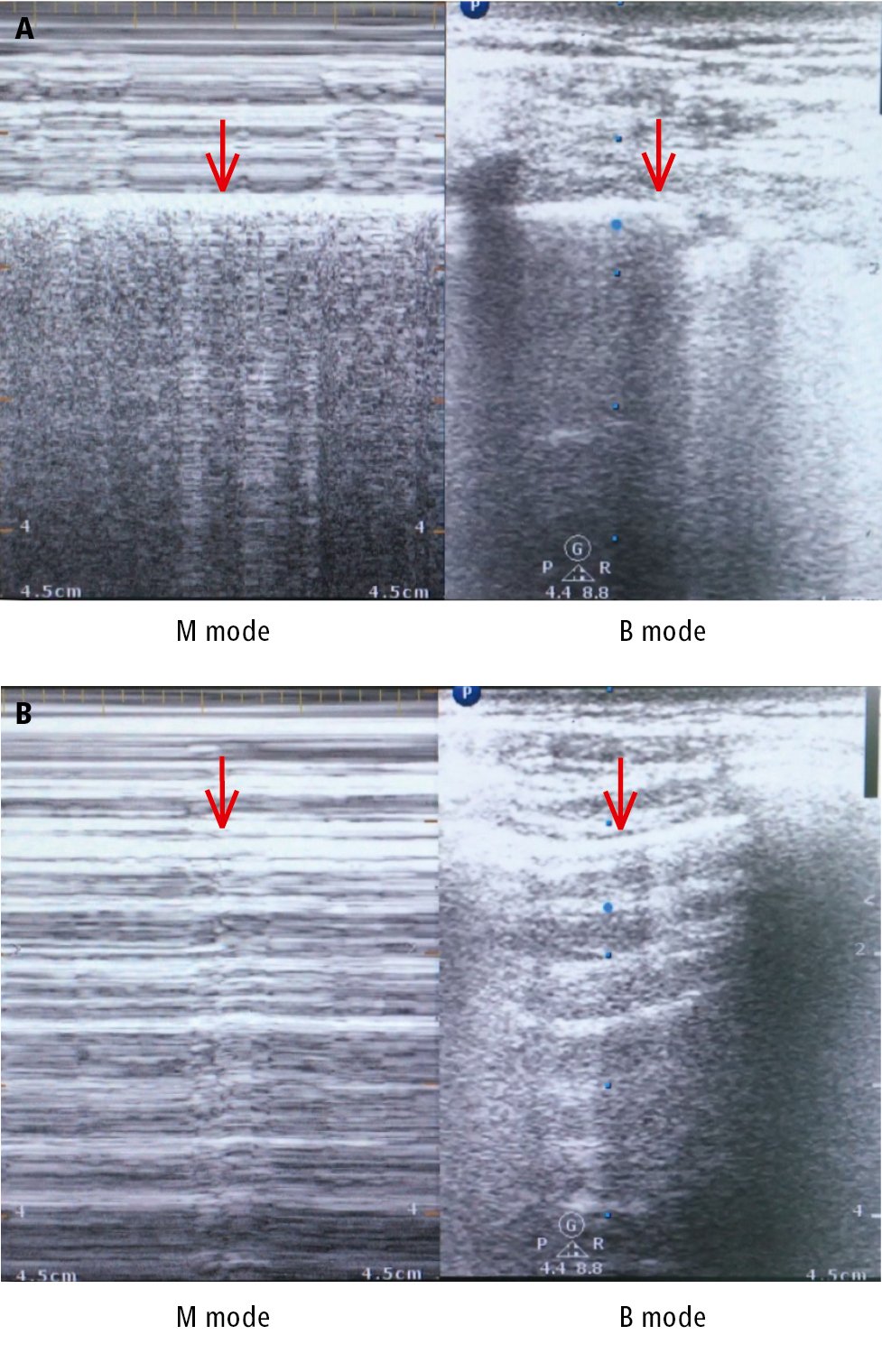
Figure 17.16-8. Pleural ultrasonography demonstrates the “seashore sign” in a healthy person (A) and the “barcode sign” in pneumothorax (B). Pleural lines are identified by arrows.
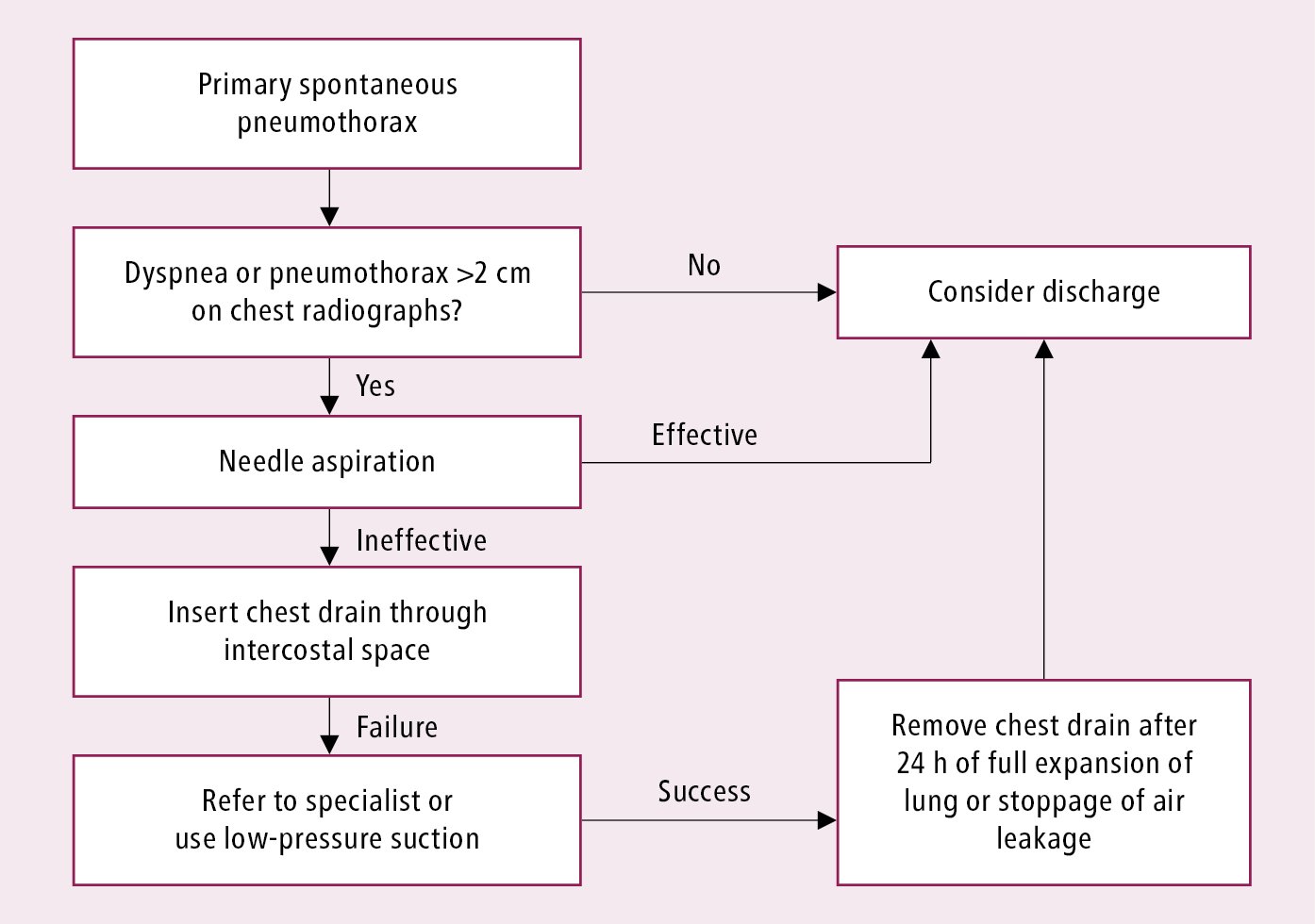
Figure 17.16-9. Treatment algorithm of primary spontaneous pneumothorax. Adapted from Thorax. 2010;65 Suppl 2:ii18-31.