A NEJM editorial was added to references on May 29, 2020.
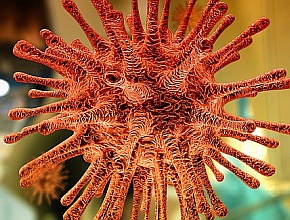
Intensive clinical investigations assessing myriad therapeutic modalities for the treatment of coronavirus disease 2019 (COVID-19), including anti-inflammatory, immune-modulating, and antiviral agents, are currently underway. Remdesivir is an antiviral agent that has been shown to have inhibitory activity against severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV). We have reviewed 2 recent papers discussing remdesivir treatment in patients with COVID-19: a randomized trial from China and a preliminary report from ACTT-1.
Remdesivir for severe COVID-19 respiratory illness: A Chinese RCT
In this multicenter trial done in Hubei, China, patients with COVID-19 and lower respiratory tract infection (LRTI) were enrolled if they presented with an oxygen saturation ≤94% on room air or a ratio of arterial oxygen partial pressure to fractional inspired oxygen (PaO2/FiO2) ≤300 mm Hg and with radiologically confirmed pneumonia. Patients were randomly allocated in a double-blind manner and 2:1 ratio to receive intravenous remdesivir—a 200 mg loading dose on day 1 followed by 100 mg daily on days 2 through 10 of hospitalization—or a matching placebo. The primary endpoint was time to clinical improvement up to day 28, which was defined as the time (in days) from randomization to the point of a 2-level reduction in clinical status on a 6-point ordinal scale (1, discharged; 6, death) or live discharge from the hospital, whichever came first.
There were 237 patients enrolled: 158 allocated to remdesivir and 79 to placebo. Treatment with remdesivir was not associated with a significant difference in time to clinical improvement (hazard ratio [HR], 1.23; 95% CI, 0.87-1.75). Patients who received remdesivir with ≤10 days of symptom duration had a statistically nonsignificant faster time to clinical improvement than those receiving placebo (HR, 1.52; 95% CI, 0.95-2.43). There was also no significant difference in adverse events in patients who received remdesivir or placebo (66% vs 64%) and no significant difference in mortality between patients who received remdesivir or placebo (14% vs 13%; rate difference, 1.1%; 95% CI, −8.1 to 10.3).
It is noteworthy that ∼30% of patients enrolled received coadministered lopinavir/ritonavir or interferon alpha-2b, two-thirds received corticosteroid therapy, and 1 in 6 patients required noninvasive or invasive mechanical ventilation. The original design was to recruit 453 patients (302 on remdesivir, 151 on placebo) but this goal was not met because of a decline in study-eligible patients during the trial. Moreover, ∼16% of patients required noninvasive or invasive mechanical ventilation. Finally, remdesivir is not widely available for clinical use in most countries.
This randomized trial does not support the use of remdesivir for the treatment of patients with COVID-19 and LRTI but should be interpreted with caution due to the smaller number of patients recruited than was planned.
Remdesivir for COVID-19 respiratory illness: A preliminary report from ACTT-1
Dolin R, Hirsch MS. Remdesivir - An Important First Step. N Engl J Med. 2020 May 27. doi: 10.1056/NEJMe2018715. Epub ahead of print. PMID: 32459913.
In the Adaptive COVID-19 Treatment Trial (ACTT-1) patients with COVID-19 and lower respiratory tract infection (LRTI) were randomly allocated in a double-blind manner to receive intravenous remdesivir—a 200 mg loading dose on day 1 followed by 100 mg daily on days 2 through 10 of hospitalization or until discharge—or a matching placebo. The primary outcome was time to recovery defined using an 8-category ordinal scale, whose criteria included the level of required hospital care, oxygen requirements, and level of activity. Mortality at 14 and 28 days after enrollment was a secondary outcome.
There were 1059 patients studied (538 allocated to remdesivir and 521 to placebo). A preliminary analysis showed that patients who received remdesivir had a statistically significant reduction in median recovery time compared with patients who received placebo: 11 days (95% CI, 9-12) versus 15 days (95% CI, 13-19). Patients who received remdesivir had a lower 14-day mortality than patients who received placebo but this difference was not statistically significant (7.1% vs 11.9%; hazard ratio [HR] for death, 0.70; 95% CI, 0.47-1.04). There was no significant difference in rates of serious adverse events between the remdesivir and placebo groups (21.1% vs 27.0%). The results for time to recovery did not appear to differ according to the severity of the presenting illness.
It is noteworthy that the ACTT-1 data and safety monitoring board recommended early unblinding of the study results on the basis of these findings; consequently, findings on 28-day mortality are not available for this analysis. Moreover, remdesivir is not widely available for clinical use in most countries.
ACTT-1 supports the use of remdesivir for the treatment of patients with COVID-19 and LRTI. Additional research is needed to assess long-term outcomes with this treatment, identify subgroups of patients who are most likely to benefit, and determine if the benefits of remdesivir are affected by coadministration of other therapeutic agents for COVID-19.
What are your thoughts about remdesivir treatment in COVID-19? Click here to submit your answer via MetaClinician and see what your peers would do.
 English
English
 Español
Español
 українська
українська