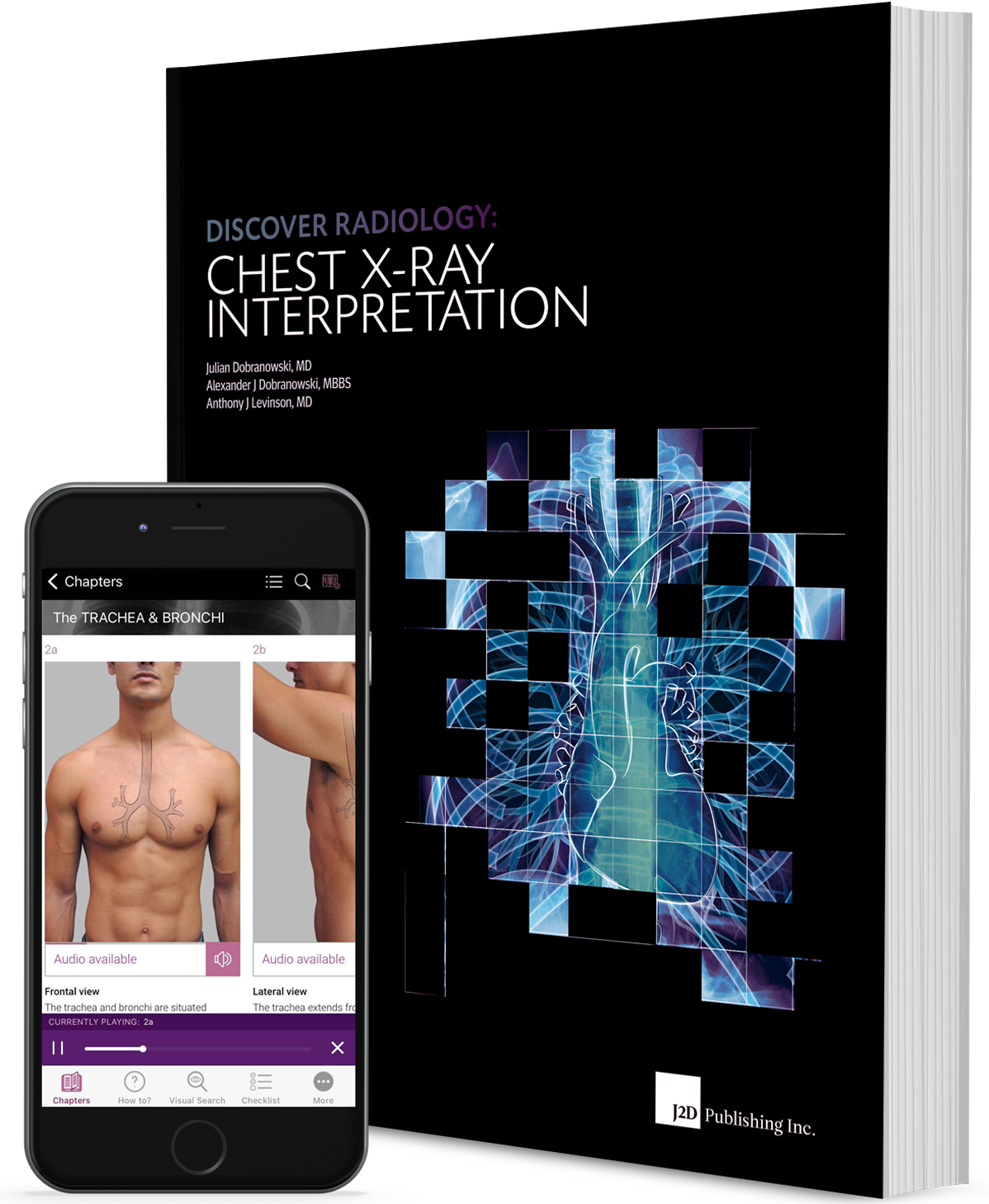
A young female patient presented at the emergency department with complaints of shortness of breath and worsening of a productive cough (Fig. 1).
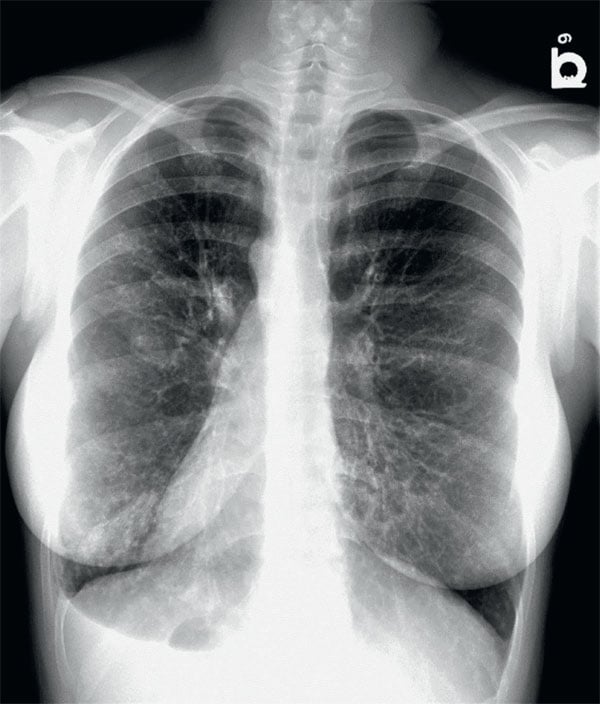
Figure 1. PA chest x-ray
Part 1: Chest Radiographs
Questions
- What is the abnormality on the chest radiographs?
- What are the differential considerations for the findings?
Answers and explanation
Chest radiograph shows dextrocardia, right sided aortic arch, gastric fundus air on the right, and bronchiectasis in the left lower lung zones, greater than that in the right ones (Fig. 2). Differential considerations include post infective bronchiectasis, cystic fibrosis and Kartagener syndrome.
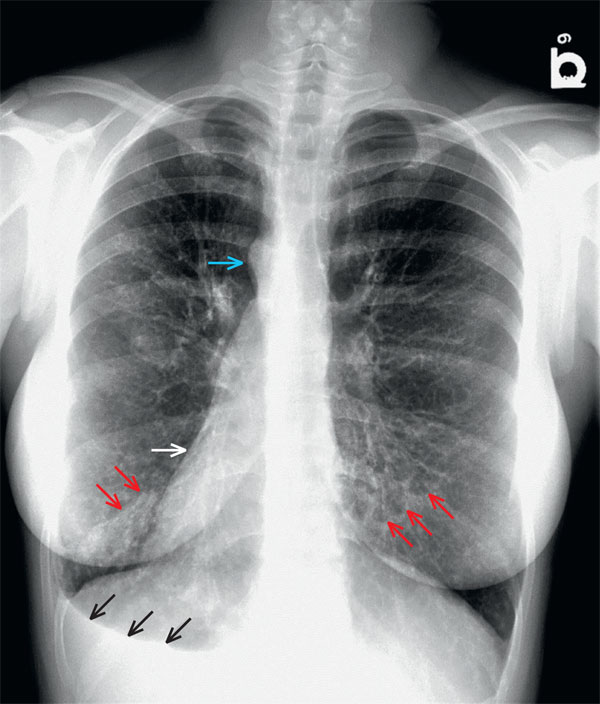
Figure 2. Frontal chest radiograph shows a right sided aortic arch (blue arrow), dextrocardia (white arrow), bronchiectasis in the lower lung zones bilaterally (red arrows) and gastric fundus on the right (black arrows).
Part 2: CT scan
The patient subsequently underwent a chest CT (Fig. 3).
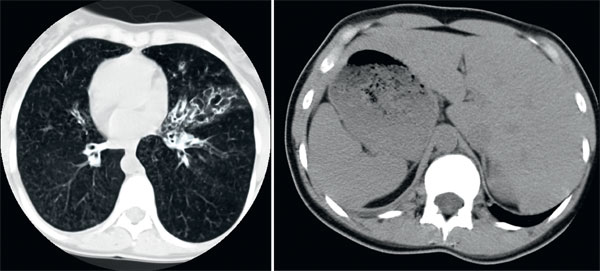
Figure 3. CT scan
Questions
- What is the abnormality?
- Is there a need for additional imaging?
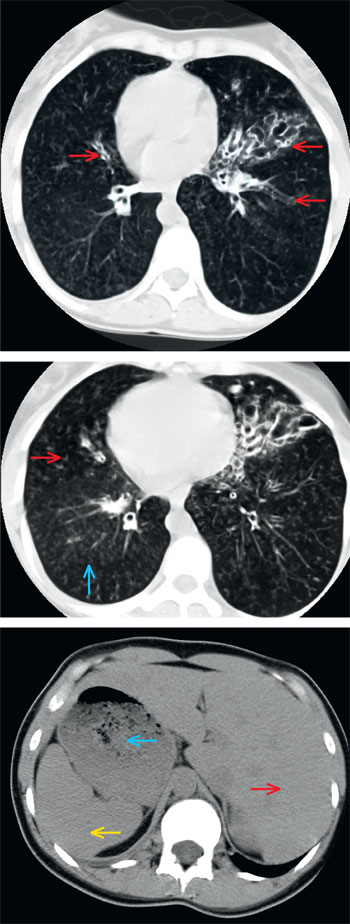
Figure 4. CT scanA – CT chest lung window demonstrates cystic and tubular bronchiectasis in the lingular segment of left upper lobe and tubular bronchiectasis in the right middle lobe (arrows). B – centrilobular nodules (blue arrow) and tree in bed opacities (red arrow) suggest endobronchial spread. C – CT upper abdomen shows stomach (blue arrow) and spleen (yellow arrow) on the right and liver (red arrow) on the left.
Answers and explanation
CT showed situs inversus with dextrocardia, as well as cystic bronchiectasis predominantly affecting the lingular segment of the left upper lobe and right middle lobe. Furthermore, the centrilobular ground-glass opacities and the tree-in-bud sign were visible in both lungs, suggesting endobronchial infection. Finally, centrilobular nodules and emphysema were noted throughout the lungs, bilaterally. Additional imaging of the paranasal sinuses should be carried out to rule out a paranasal sinus disease e.g. chronic sinusitis and/or nasal polyposis. A diagnosis of KS was made based on clinical presentation and imaging features.
Summary
Kartagener syndrome (KS) is an inherited autosomal recessive disorder that causes defects in the action of ciliary movements and is a subset of a larger group of ciliary motility disorders called primary ciliary dyskinesias (PCD). It was first recognized in 1933 by Manes Kartagener as a clinical triad of sinusitis, situs inversus and bronchiectasis1. The reported incidence is 1 in 30,000 live births2. Normal ciliary function is important for respiratory host defence and motility of sperm and ensures proper visceral orientation during embryogenesis.
In KS, there are mutations in genes DNAL1 and DNAH5, leading to impaired ciliary motility that predisposes to recurrent sinus and pulmonary infections, infertility and errors with left-right body orientation. Diagnosis is made by various ciliary function tests, genetic testing and biopsy. Imaging plays an important role in the diagnosis. Early diagnosis and treatment change patient’s prognosis.
Kartagener syndrome is the first reported primary ciliary dyskinesia characterized by a triad of situs inversus, bronchiectasis and chronic sinusitis. The most common signs and symptoms include bronchiectasis, situs inversus, male infertility due to impaired sperm motility, and female ectopic pregnancy or infertility because of ciliary dysfunction in the fallopian tubes3.
Imaging studies have an important supporting role in the diagnosis of KS. Patients with respiratory symptoms readily undergo a plain chest radiograph. In KS, the findings of a chest radiograph include bronchiectasis with mid to lower lobe predilection4. The findings depend on the severity of underlying bronchiectasis. Additional findings include situs inversus, a term used to describe the inverted position of chest and abdominal organs. The condition is called situs inversus totalis, where there is a total transposition of abdominal and thoracic viscera (mirror image of internal organs normal positioning). Much more rare is transposition of the abdominal organs with a 'normal' left-sided heart, known variously as situs inversus incompletus, situs inversus partialis, or simply situs inversus with laevocardia.
High-resolution CT is an important tool in the detection and management of bronchiectasis. High-resolution CT shows that pulmonary disease related to PCD predominantly involves the middle and lower lobes of the lungs. In a study by Kennedy. et al, the right middle lobe was the most common lobe to manifest bronchiectasis in both adult (93%) and pediatric patients(38%).The distribution of bronchiectasis was central (42%) or diffuse (53%). No patient was found to have peripheral bronchiectasis alone5. In adults, high-resolution CT findings negative for bronchiectasis may have a role in excluding the diagnosis of PCD. Correlation of severity of disease on high-resolution CT with patient phenotype gives further insight into the diversity and natural history of PCD5. Peribronchial consolidation, mucous plugging, atelectasis, and nonspecific infiltrates have been associated with bronchiectasis and could be seen in KS6.
Tree-in-bud pattern or centrilobular nodules may be encountered with mucus impaction and endobronchial spread of an infection. Eventual scarring may result from recurrent infection, requiring pulmonary resection surgery. Abnormal ciliary motility also leads to chronic recurrent sinus infections; therefore, it is not uncommon to see paranasal sinus disease on CT. An important differential diagnosis includes Cystic fibrosis (a genetic disorder also leading to defective airway mucociliary clearance with common clinical and radio-graphic features)7. In Cystic fibrosis, disease pre-dominates in the upper lobes or is diffuse throughout both lungs. Imaging may help in the early diagnosis and help to prevent complications7.
Diagnosis
Kartagener syndrome
In conclusion, situs abnormality in association with lower lobe bronchiectasis should prompt the diagnosis of Kartagener syndrome. A high index of suspicion is needed to make an early diagnosis, so that timely treatment options may be offered to prevent associated problems.
You can find more interesting cases in the app "Discover Radiology: Chest x-ray interpretation".
Price – only $6.99
References
1. Crespo P., Salto M.F., Aguilar R.C. i wsp.: Kartagener syndrome: neonatal diagnosis. A case report. Arch. Argent. Pediatr., 2019; 117: e292-e2962. Ibrahim R., Daood, H.: Kartagener syndrome: a case report. Can. J. Respir. Ther., 2021; 57: 44-48
3. Chen W., Shao C., Song Y., Bai C.: Primary ciliary dyskinesia complicated with diffuse panbronchiolitis: a case report and literature review. Clin. Respir. J., 2014; 8: 425-430
4. Tadesse A., Alemu H., Silamsaw M., Gebrewold Y.: Kartagener's syndrome: a case report. J. Med. Case Reports, 2018; 12: 5
5. Kennedy M.P., Noone P.G., Leigh M.W. i wsp.: High-resolution CT of patients with primary ciliary dyskinesia. AJR Am. J. Roentgenol., 2007; 188: 1232-1238
6. Lucas J.S., Paff T., Goggin P., Haarman E.: Diagnostic methods in primary ciliary dyskinesia. Paediatr. Respir. Rev., 2016; 18: 8-17
7. Gupta S., Handa K.K., Kasliwal R.R., Bajpai P.: A case of Kartagener's syndrome: importance of early diagnosis and treatment. Indian J. Hum. Genet., 2013; 19: 266-269