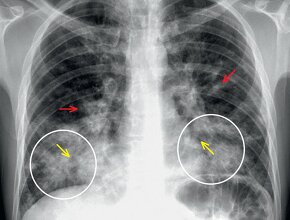
A 57-year-old male patient with chest pain. You order a chest x-ray examination (Fig. 1a,b).
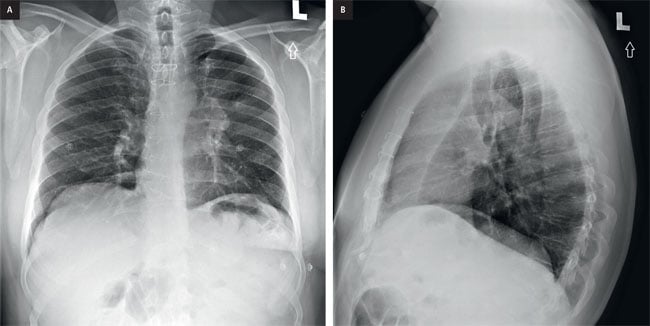
Figure 1. a, PA chest x-ray, b, lateral chest x-ray.

Figure 2. Normal PA chest x-ray for comparison.
Can you identify an abnormality on the PA and on the lateral views?
PA chest x-ray (Fig. 3) demonstrates several abnormalities. First, there is a veil-like opacity overlying the left hemithorax. This is associated with generalized volume loss (small left hemithorax, elevated left hemidiaphragm).
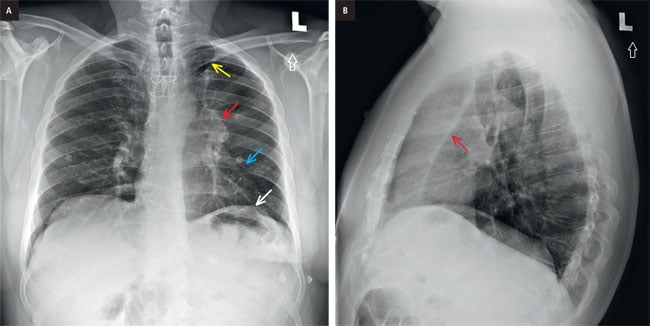
Figure 3. a, PA chest x-ray: Note the left hilum is higher than the level of the right hilum (red arrow). These signs are diagnostic for lobar collapse. The next step is deciding, which lobe is collapsed. In the above case, the left cardiac border is silhouetted (blue arrow) whereas the left hemidiaphragm is not (white arrow). This tells us that the left upper lobe and lingula are collapsed. Small volume pneumatized lung at the left apex is likely secondary to pneumatized superior segment of the left upper lobe, termed Luftsichel sign (yellow arrow). b, lateral chest x-ray: Notice a band like opacity over the retrosternal space associated with a straight sharp posterior border (arrow), confirming a left upper lobe collapse. The straight border is secondary to the left major fissure.
If you identified these findings, then well done. To complete the interpretation of the chest x-ray we need to go over all of the other structures to make sure we did not miss anything.
Are the trachea and the airways normal? YES
Is the heart normal? YES
Is the chest wall normal? NO
Is the pleura normal? YES
No additional findings are present. In a non-hospitalized patient, sudden lobar collapse is always suspicious for a central bronchial or perihilar mass. Therefore, you must proceed with additional testing.
If there are no contraindications (anaphylactic reaction to iodine contrast agent or acute severe kidney injury), the best second line is contrast enhanced computed tomography (CT) of the chest. This can be done immediately at the time of the radiograph or on a semi-urgent basis if the patient is being seen in the outpatient setting.
The CT images confirm complete collapse of the left upper lobe and lingula (Fig. 4, arrows).
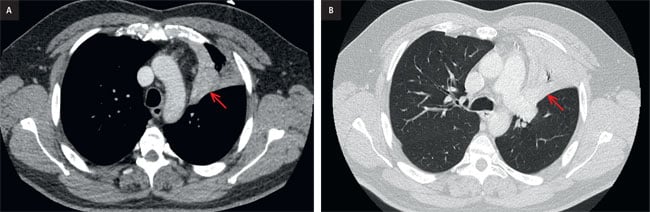
Figure 4. CT scan. a, axial image, soft tissue window, b, axial image, lung window.
The collapsed lung is homogenous and a dominant measurable mass was not identified on this exam. However, the sudden lobar collapse in an otherwise healthy patient is once again concerning for a central obstructive mass. Therefore, either bronchoscopy or positron-emission tomography CT (PET-CT) should be performed. In this case, both procedures were performed for the patient for work-up completion.
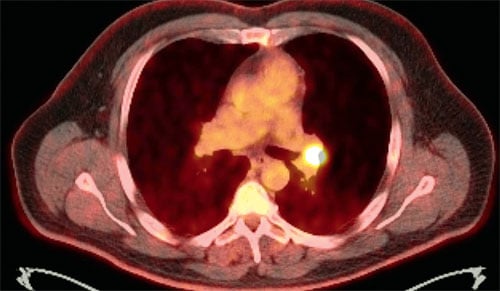
Figure 5. PET-CT scan. The PET-CT confirms that the lesion of concern has high metabolic activity and is therefore likely malignant. Infectious masses can also show hypermetabolic activity which is why sampling is critical.
This confirms the presence of an endobronchial heterogenous soft tissue mass occupying most of the bronchial lumen. The mass is mildly hemorrhagic but the appearance is non-specific. This mass was sampled endobronchial and the LUL collapse was partially relieved during the procedure.
As noted above, this mass is not discretely identified on CT but the presence of an acute lobar collapse in the outpatient setting is a strong secondary indicator of an obstructive bronchial mass.
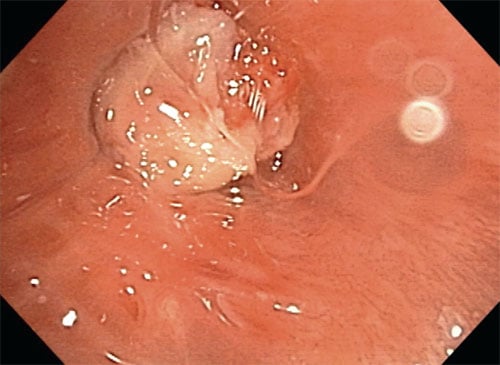
Ryc. 6. Bronchoscopy: image obtained during bronchoscopy and endo-bronchial biopsy of the LUL bronchus.
Summary
This is a 57-year-old male patient with sudden LUL collapse. In an otherwise well patient, the diagnosis of exclusion is an obstructive central or endobronchial mass. If the mass is not seen on contrast-enahnced CT, further work-up is required to diligently look for the obstructive lesion which can sometimes be quite small. In this case, a lesion was demonstrated on both bronchoscopy and PET-CT.
In general, the differential considerations for a central mass are:
- Bronchogenic carcinoma
- arcinoid tumor
- Aspirated foreign body or food particles
You can find more interesting cases in the app "Discover Radiology: Chest x-ray interpretation".
Price – only $6.99>
References
1. Raasch B.N., Heitzman E.R., Carsky E.W. i wsp.: A computed tomographic study of bronchopulmonary collapse. Radiographics, 1984; 4: 195–2322. Blankenbaker D.G.: The luftsichel sign. Radiology, 1998; 208: 319–320
3. Singh S., Singh N., Tikkiwal S.: Luftsichel sign. Lung India. 2012; 29: 83–84