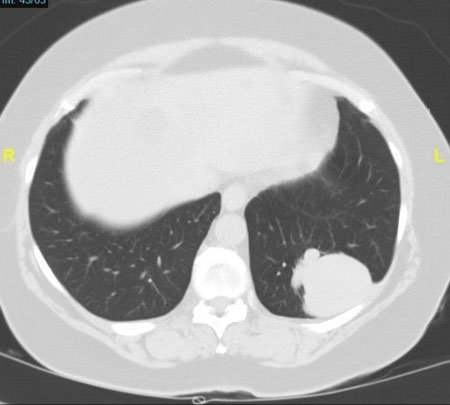
A 45-year-old male with history of HIV and skin lesions presented with chronic pulmonary findings not responding to antibiotic therapy. The patient’s CD4 count was less than 200 cells/µL and he had elevated HHV–8 antibody titer. Posteroanterior (PA) chest radiographs were requested (Fig. 1).
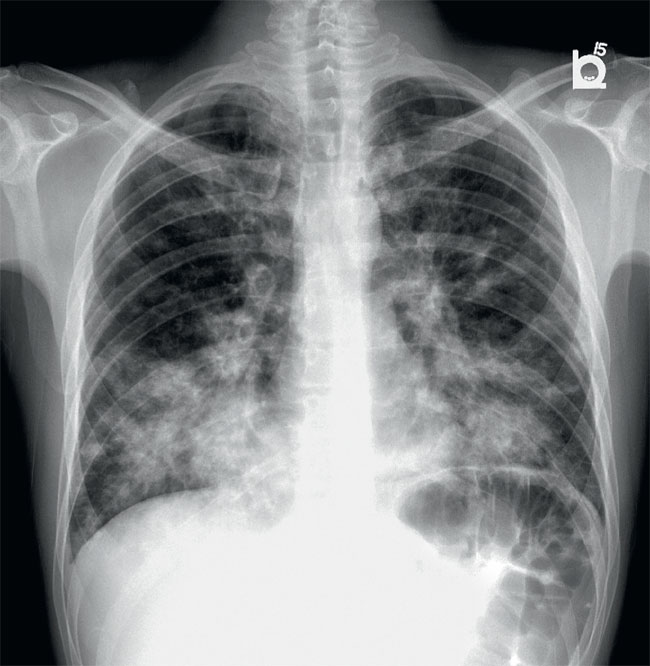
Figure 1. PA chest x-ray
Part 1: Chest Radiographs
Question
- Do you see any abnormalities on the PA radiograph?
- How do you describe the principle abnormality?
- Where is the precise location of the abnormality?
Answers and explanation
The most apparent finding on the PA image (Fig. 2) is the presence of bilateral heterogeneous irregular mass-like opacities and consolidations with central distribution and perihilar predominance. There is relative sparing of the upper lobes, pleural spaces are clear, and cardiac silhouette is not widened. These consolidations show an air-bronchogram pattern.
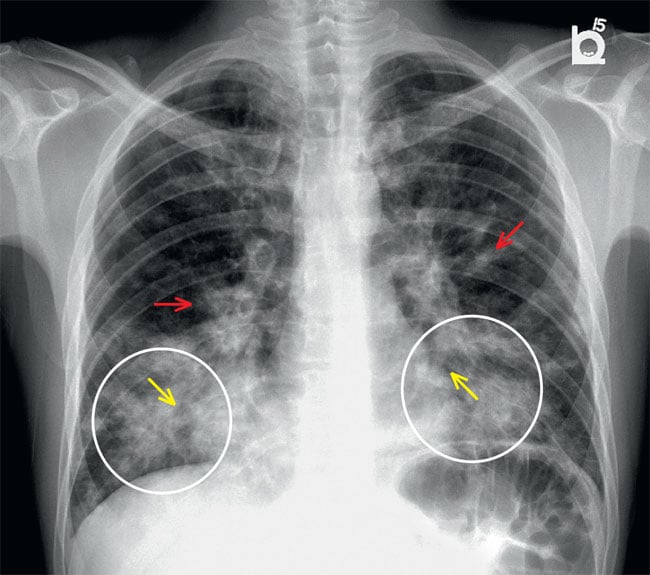
Figure 2.
PA chest x-ray. Irregularly shaped opacities (circles) can be observed overlying lower lung fields with a central distribution (yellow arrows).
Irregular opacities with air bronchogram pattern (red arrows) can be observed centrally with a perihilar predominance and relative sparing of the upper lobes.
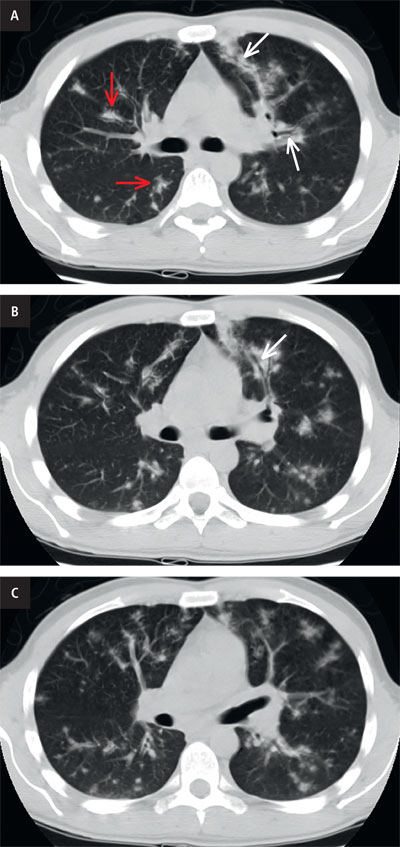
Figure 3. CT scan. a. coronal reformatted image shows bilateral irregular flame-shaped nodular opacities (red arrows) along with peribronchovascular distribution (white arrows), relative sparing of the periphery; b. axial in lung window. The tendency of KS to grow in the axial interstitium (arrow). No significant mediastinal lymphadenopathy is seen. No pleural effusions are seen. c. axial in lung window. Poorly defined lung nodules. Central airways are patent. No ground-glass opacities.
Approach the differentials with a chest radiograph and demystify chronic air space diseases?
Infections remain the predominant cause of respiratory disease in HIV. However, non-resolving consolidation could be secondary to an atypical infection like mycobaterim, lymphoma and Kaposi Sarcoma. The presence of skin lesions might suggest Kaposi sarcoma.
Chest radiographic findings are nonspecific, and Kaposi sarcoma frequently coexists with opportunistic infections in people with AIDS.
There are two distinct patterns visible: diffuse linear and reticular interstitial opacities (including Kerley B lines), and diffuse nodular opacities. Both patterns have a perihilar dispersion, indicating a bronchovascular distribution. Bronchovascular nodules can take on the appearance of flames. Pleural effusions are frequently seen. Although hilar and mediastinal lymphadenopathy is widespread, they are not bulky.
In our case, the fungal disease, bacterial bronchopneumonia, mycobacterial infection, and lymphoma were top differentials of nodular disease, which is already diagnosed with AIDS.
Part 2: CT scan
This case was subsequently investigated with a CT scan of the chest. Please review the CT scan (Fig. 3). It shows that there are bilateral perihilar consolidations with air bronchograms. Irregular nodules or masses with a peribronchovascular distribution, often called "flame-shaped" lesions, are very characteristic.
| Top Differential Diagnosis | |
|---|---|
| sarcoidosis | thickening of bronchovascular bundle, perilymphatic distribution of lung nodules, & septal thickening (often nodular) mimic KS Lymphadenopathy – does not typically enhance |
| pulmonary edema | difficult to differentiate clinical history of AIDS/transplant & presence of skin lesions may provide a clue |
| Lymphoma | peribronchovascular bundle thickening larger nodules without atypical flame shape air bronchograms are more common in lymphoma |
| Lymphangitic carcinomatosis | peribronchovascular bundle & nodular septal thickening unilateral distribution favors lymphangitic carcinomatosis |
| infectious bronchiolitis | mycobacterial & bacterial infections centrilobular nodules than peribronchovascular with tree-in-bud appearance |
Diagnosis
Pulmonary Kaposi SarcomaSummary
Clinical Vignette
- Kaposi sarcoma was the first AIDS-defining malignancy – low-grade mesenchymal neoplasm of blood & lymphatic vessels, primarily affecting the skin.
- Cause: Kaposi sarcoma-associated human herpesvirus 8 [HHV–8], notorious for having infections that last a long time and cause diseases that weaken the immune system. Classic–KS: 50–80 years.
- The most common sites of involvement are skin, lymph nodes, lungs, and gastrointestinal tract.
- Cutaneous lesions on the skin are pink, purple, or brown, and they can be of different sizes and shapes. There are different mucosal lesions in the mouth, larynx, and pharynx. There are patches, raised plaques, and nodular lesions.
- Gastrointestinal involvement can be found in about half the cases of oral Kaposi sarcoma. Patients may show up with these symptoms because ulcerated mucosal lesions can cause pain, haemorrhaging, diarrhoea, or weight loss. Endoscopy can look at these ulcerated lesions.
- Pulmonary Kaposi sarcoma: Patients may have a cough, fever, shortness of breath, hemoptysis, and chest pain because the disease spreads to the parenchyma, airway, lymphatic, pleural, and chest wall. The appearance on the radiograph can range from reticular interstitial opacities with perihilar predominance to parenchymal nodular lesions. Pleural effusions and lymphadenopathy are often seen.
CT shows multiple bilateral symmetric “flame-shaped” or ill-defined nodular lesions peribronchovascular distribution. Ground-glass opacities and thickening of the interlobar septal walls may be seen.
Teaching point
- Patients with mildly abnormal radiographs had coarsening of the bronchovascular bundles, with "tram–track" opacities and peribronchial cuffing generally observed in the central perihilar lung, consistent with axial interstitial illness.
- The majority may present the peribronchial cuffing and thickening of the bronchial wall (usually bilateral and most apparent in the central lower lung zones).
- KS has a proclivity for growth in the peribronchial axial interstitial spaces, frequently as continuous tumor sheets.
- Consolidation of coalescent material with or without an air bronchogram. Confluent tumor with central perihilar consolidation and formation of nodules when tumor proliferates, invading the parenchyma.
- When this peribronchovascular distribution is not visible on normal radiographs, it can be seen clearly on computed tomography, which can aid in establishing the differential diagnosis.
- On CT scans, the small nodules frequently have a similar distribution. When coupled with nodules, linear axial or peripheral interstitium anomalies are highly indicative of KS in the appropriate clinical situation.
Because of these ubiquitous manifestations of Kaposi sarcoma, it is essential to be aware of its various imaging faces.
You can find more interesting cases in the app "Discover Radiology: Chest x-ray interpretation".
Price – only $6.99
References
1. Javadi S., Menias C.O., Karbasian N. i wsp.: HIV-related malignancies and mimics: imaging findings and management. Radiographics, 2018; 38: 2051–20682. Rosado-de-Christenson M.L., Martínez-Jiménez S.: Diagnostic imaging: chest. Elsevier, 2021
3. Restrepo C.S., Martínez S., Lemos J.A. i wsp.: Imaging manifestations of Kaposi sarcoma. Radiographics, 2006; 26: 1169–1185
4. Garay S.M., Belenko M., Fazzini E., Schinella R.: Pulmonary manifestations of Kaposi's sarcoma. Chest, 1987; 91: 39–43
5. Cheung M.C., Pantanowitz L., Dezube B.J. AIDS-related malignancies: emerging challenges in the era of highly active antiretroviral therapy. Oncologist, 2005; 10: 412–426
6. Gruden J.F., Huang L., Webb W.R. i wsp.: AIDS-related Kaposi sarcoma of the lung: radiographic findings and staging system with bronchoscopic correlation. Radiology, 1995; 195: 545–552