A 64-year-old male patient with central chronic worsening chest pain which was investigated with posteroanterior (PA) and lateral chest x‑rays (Fig. 1a and b).
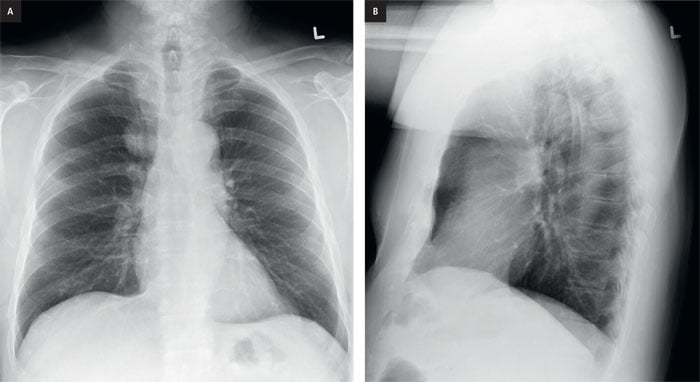
Figure 1. a, PA chest x-ray, b, lateral chest x-ray.
Do you see an abnormality on the PA view?
If you do not see an abnormality on the PA x‑ray, take the systematic approach to its interpretation. A full review of the systematic approach is found in "Discover Radiology: Chest x‑ray interpretation" book, Chapter 5 or in application.
You should check
Are the trachea and the airways normal?
Are the lungs normal?
Is the mediastinum normal?
Are the hila normal?
Is the chest wall normal?
Is the pleura normal?
There are several areas on the PA chest x‑ray where we can easily miss an abnormality. Figure 2a and b present the most common areas where pathologies are missed on PA and lateral chest x-rays.
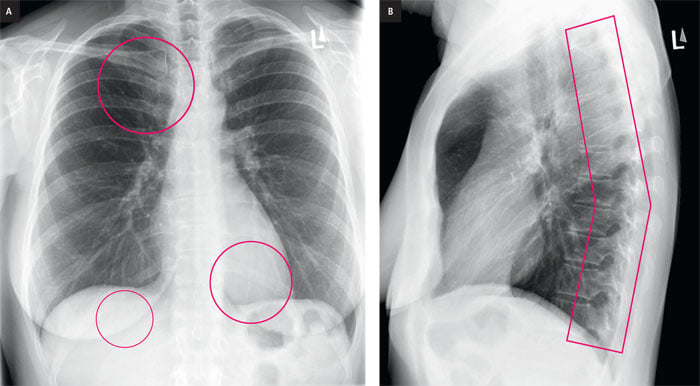
Figure 2. Normal PA and lateral chest x-ray. The areas where pathologies are commonly missed are
highlighted with white circles on PA chest x‑ray (a) and with white shape on lateral view (b).
Now take a look at our case again. If we look at the lungs you will see that the right side is superiorly whiter
than the corresponding region on the left (Fig. 3a). The white area is homogeneous and has smooth, sharp upper,
lower and lateral borders. The medial border is not seen.
Before we can discuss what this is, we need to localize the abnormality on the x‑ray. What are the possibilities?
Anterior chest wall, anterior pleura, lung, mediastinum, posterior pleura or posterior chest wall.
To narrow down the possibility you need to look at the lateral x‑ray. Do you see an abnormality on the lateral view
(Fig. 1b)?
On the lateral x‑ray, there is an abnormal opacity that lies superiorly and posteriorly (Fig 3b).
So, we can eliminate anterior chest wall, anterior pleura, posterior pleura and posterior chest wall. The remaining possibilities are lung and mediastinum.
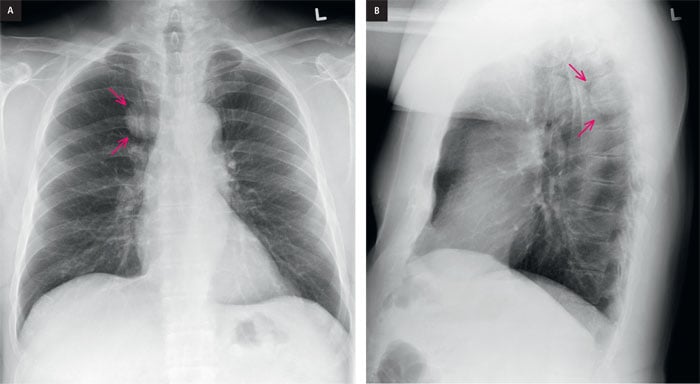
Figure 3. a, PA chest x‑ray. Round, homogeneous right upper para-mediastinal
lesion (arrows) with smooth upper, lower and lateral borders. The medial border is obscured. b, Lateral chest x‑-ray
shows a round, well defined posterior mediastinal lesion (arrows) that has smooth upper, lower and anterior borders.
The posterior border is not visible.
When you see a lesion that looks like it lies in the lungs but one of the borders is obscured (like in this case), consider that the lesion originates outside of the lungs but forms an interface with the lung. This is known as incomplete border sign which is a useful sign to confirm the extra-pulmonary location of a mass.
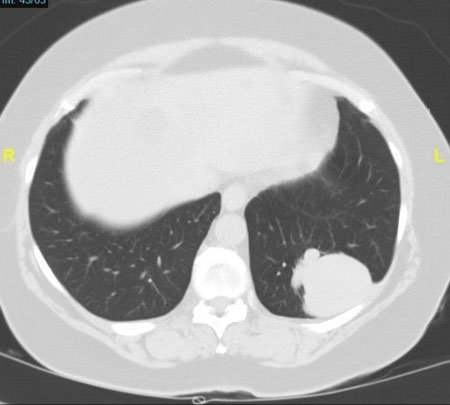
To further accurately localize the abnormality a chest CT scan was performed (Fig. 4).
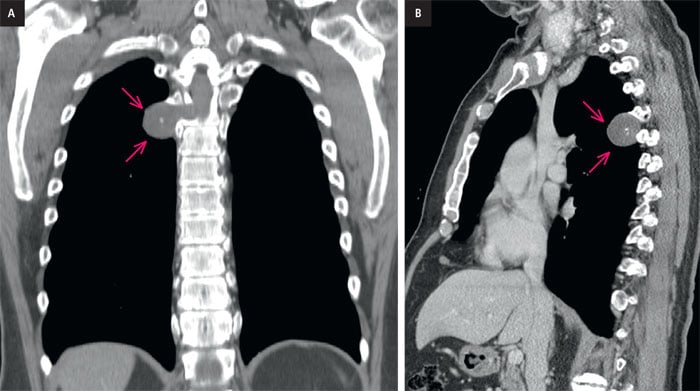
Figure 4. a, coronal CT scan. There is a soft tissue density (arrows) lesion within the right posterior
mediastinum, in a paravertebral location and forming a smooth interface with the lung parenchyma. Note the presence
of central calcification. This corresponds with the PA chest x‑ray finding. There is associated boney remodeling but
no osseous destruction.
b, sagittal CT scan. Soft tissue lesion (arrows) originating from the posterior spine region
and forming a smooth interface with the lung. Note the presence of central calcification. This corresponds with the
lateral chest x‑ray finding.
The CT examination (Fig. 4a,b) shows the lesion is clearly originating from the right T4-T5 neuro foramina of the thoracic spine. This was also confirmed on an MRI examination (Fig. 5)
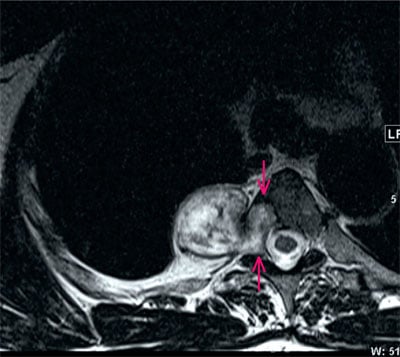
Figure 5. Axial MRI. T2 weighted soft tissue (white arrows) shows the lesion originating from and
expanding the right T4‑T5 neuro foramen. The lesion demonstrates heterogeneous T2 high signal with small
areas of low signal due to calcification. It has a classic dumbbell or hourglass appearances of spinal peripheral nerve
sheath tumors.
Summary
The chest x‑ray shows an opacity on the right on the PA x-ray. The lateral x‑ray shows the lesion posteriorly. Pathology in this region can be easily missed because of an overlap of the ribs and the clavicle. The area is too busy. This area on lateral x‑ray is called Raider’s triangle (Retrotracheal triangle) (Ref. 1). A CT scan is needed to further localize and characterize the lesion. In this case the CT scan showed that the opacity originated from paravertebral soft tissues and the neuro foramen. The full extent of spinal involvement was assessed with MRI.
Diagnosis
Spinal Schwannoma (Ref.2)
It is a benign nerve sheath tumor that typically arises from spinal nerve roots.You can find more interesting cases in the app "Discover Radiology: Chest x‑ray interpretation".
Price – only $6.99
References
1. Raider L., Landry B.A., Brogdon B.G.: The retrotracheal triangle. Radiographics, 1990; 10: 1055–10792. Bicakcioglu P., Demirag F., Yazicioglu A. i wsp.: Intrathoracic neurogenic tumors. Thorac. Cardiovasc. Surg., 2014; 62: 147–152