Restablecimiento de la anticoagulación después de las intervenciones programadas
- Si antes de una intervención programada se suspendió el tratamiento antiagregante o anticoagulante, se recomienda restablecerlo hasta 2‑3 días después del procedimiento, en función del riesgo de sangrado y el riesgo trombótico esperado [F/M].
- Es necesario informar a todos los enfermos que reciben antiagregantes o anticoagulantes sobre el riesgo elevado, en comparación con los enfermos que no reciben estos fármacos, de sangrados posteriores a la intervención [F/B].
Existen pocos datos relativos al momento óptimo para restablecer el tratamiento anticoagulante que fue discontinuado antes de una intervención endoscópica programada. En todos los casos, la decisión debe ser individual y basarse en el análisis de riesgo de sangrado después de la intervención, y de riesgo trombótico en un paciente determinado. Se debe tomar en cuenta que el efecto anticoagulante de los ACOD se mantiene entre 10 y 20 h, mientras que el efecto de la warfarina persiste varios días. Los datos del estudio PAUSE indican que el restablecimiento de ACOD a los 2‑3 días de la intervención de alto riesgo de sangrado se asocia a un bajo riesgo de eventos tromboembólicos.19 En un estudio italiano que evaluó el riesgo de sangrado y de trombosis en función de la adherencia a las guías anteriores de la BSG y la ESGE en personas tras la polipectomía, se observó la tendencia a una mayor prevalencia de sangrados inmediatos, si los ACOD no fueron discontinuados según las recomendaciones.24 La prolongación de la pausa no disminuyó el riesgo de sangrado durante la intervención. El restablecimiento de ACOD directamente después de la polipectomía, y no a las 24‑48 h de la intervención (como lo sugieren las guías), en los enfermos del grupo de alto riesgo aumentó el riesgo de sangrado tardío en casi 2 veces y no disminuyó el riesgo de trombosis, aunque estas diferencias no fueron estadísticamente relevantes.
Durante los procedimientos con riesgo de sangrado muy alto, p. ej. DES, puede ser razonable posponer el restablecimiento de los anticoagulantes, fuera de los plazos recomendados en las guías. Se ha demostrado que el riesgo de sangrado después de la DES no aumentó significativamente si la terapia anticoagulante se restableció ≥1 semana después de la intervención, mientras que el restablecimiento de la misma directamente después del procedimiento o dentro de la primera semana se asoció a un aumento importante de la frecuencia de sangrados.27
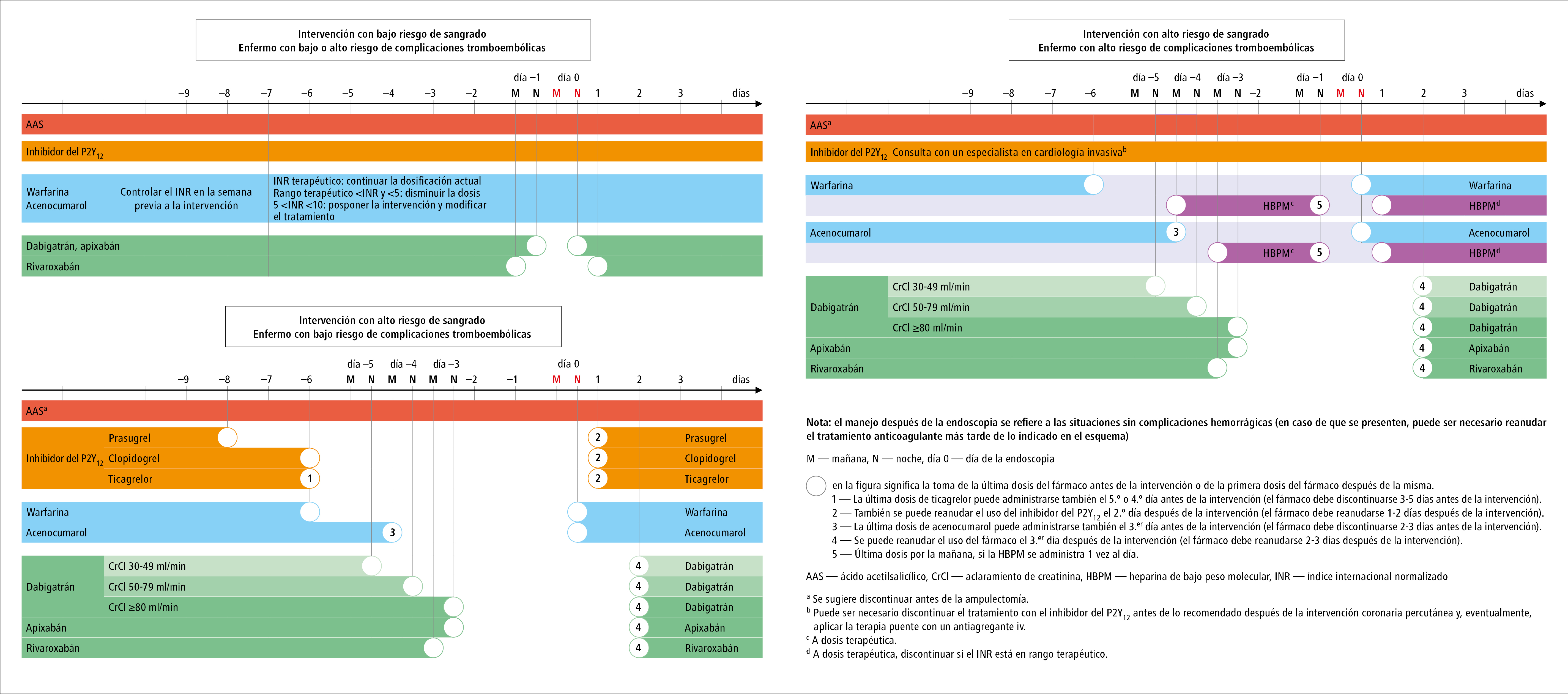
El algoritmo de manejo en el período perioperatorio en los pacientes anticoagulados, que toma en cuenta las guías de la ESG y la BSG, así como las guías de la ESC, se presenta en la figura 4.
Fig. 4. Modificaciones en el tratamiento anticoagulante en los pacientes sometidos a la endoscopia del tracto digestivo
Volver al artículo principal: Guías: endoscopia del tracto digestivo en los pacientes que reciben anticoagulantes
Bibliografía:
- Veitch A.M., Radaelli F., Alikhan R. y cols., Endoscopy in patients on antiplatelet or anticoagulant therapy: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline update, Gut, 2021; 70: 1611‑1628
- Veitch A.M., Vanbiervliet G., Gershlick A.H. y cols., Endoscopy in patients on antiplatelet or anticoagulant therapy, including direct oral anticoagulants: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines, Gut, 2016; 65: 374‑389
- Abraham N.S., Barkun A.N., Sauer B.G. y cols., American College of Gastroenterology‑Canadian Association of Gastroenterology Clinical Practice Guideline: management of anticoagulants and antiplatelets during acute gastrointestinal bleeding and the periendoscopic period, Am. J. Gastroenterol., 2022; 117: 542‑558
- Douketis J.‑D., Spyropoulos A.C., Murad H. y cols., Perioperative management of antithrombotic therapy: An American College of Chest Physicians Clinical practice guideline, Chest, 2022; 162: e207‑e243
- Halvorsen S., Mehilli J., Cassese S. y cols., 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non‑cardiac surgery, Eur. Heart J., 2022; 43: 3826‑3924
- Acosta R.D., Abraham N.S., Chandrasekhara V. y cols., The management of antithrombotic agents for patients undergoing Gi endoscopy, Gastrointest. Endosc., 2016; 83: 3‑16
- Hindricks G., Potpara T., Dagres N. y cols., ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio‑Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC, Eur. Heart J., 2021; 42: 373‑498
- Oscarsson A., Gupta A., Fredrikson M. y cols., To continue or discontinue aspirin in the perioperative period: a randomized, controlled clinical trial, Br. J. Anaesth., 2010; 104: 305‑312
- Knuuti J., Wijns W., Sarante A. y cols., 2019 Guidelines for the diagnosis and managment of chronic coronary syndromes, Eur. Heart. J., 2020; 41: 407‑477
- Yasuda S., Kaikita K., Akao M. y cols., Antithrombotic therapy for atrial fibrillation with stable coronary disease, N. Engl. J. Med. Overseas Ed., 2019; 381: 1103‑1113
- Gori T., Polimeni A., Indolfi C. y cols., Predictors of stent thrombosis and their implications for clinical practice, Nat. Rev. Cardiol., 2019; 16: 243‑256
- Dasa O., Pepine C.J., Pearson T.A., Aspirin in primary prevention: what changed? A critical appraisal of current evidence, Am. J. Cardiol., 2021; 141: 38‑48
- Valgimigli M., Bueno H., Byrne R.A. y cols., 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the task force for dual antiplatelet therapy in coronary artery disease of the European Society of cardiology (ESC) and of the European association for Cardio‑Thoracic surgery (EACTS), Eur. Heart J., 2018; 39: 213‑260
- Witt D.M., Nieuwlaat R., Clark N.P. y cols., American Society of Hematology 2018 guidelines for management of venous thromboembolism: optimal management of anticoagulation therapy, Blood Adv., 2018; 2: 3257‑3291
- Otto C.M., Nishimura R.A., Bonow R.O. y cols., 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines, Circulation, 2021; 143: e72‑e227
- Douketis J.D., Spyropoulos A.C., Kaatz S. y cols., Perioperative bridging anticoagulation in patients with atrial fibrillation, N. Engl. J. Med. Overseas Ed., 2015; 373: 823‑833
- Keeling D., Tait R.C., Watson H., et al y cols., Perioperative management of anticoagulation and antiplatelet therapy, Br. J. Haematol., 2016; 175: 602‑613.
- Chan F.K.L., Goh K.‑L., Reddy N. y cols., Management of patients on antithrombotic agents undergoing emergency and elective endoscopy: joint Asian Pacific association of gastroenterology (APAGE) and Asian Pacific Society for digestive endoscopy (APSDE) practice guidelines, Gut, 2018; 67: 405‑417
- Douketis J.D., Spyropoulos A.C., Duncan J. y cols., Perioperative management of patients with atrial fibrillation receiving a direct oral anticoagulant, JAMA Intern. Med., 2019; 179: 1469‑1478
- Beyer‑Westendorf J., Gelbricht V., Förster K. y cols., Peri‑interventional management of novel oral anticoagulants in daily care: results from the prospective Dresden NOAC registry, Eur. Heart J., 2014; 35: 1888‑1896
- Douketis J.D., Healey J.S., Brueckmann M. y cols., Perioperative bridging anticoagulation during dabigatran or warfarin interruption among patients who had an elective surgery or procedure. substudy of the RE‑LY trial, Thromb. Haemost., 2015; 113: 625‑632
- Steffel J., Collins R., Antz M. y cols., 2021 European Heart Rhythm Association. Practical guide on the use of non‑vitamin K antagonist oral anticoagulants in patients with atrial fibrillation, Europace, 2021; 23: 1612‑1676
- Yuki T., Ishihara S., Yashima K. y cols., Bleeding risk related to upper gastrointestinal endoscopic biopsy in patients receiving antithrombotic therapy: a multicenter prospective observational study, Curr. Ther. Res. Clin. Exp., 2017; 84: 32‑36
- Radaelli F., Fuccio L., Paggi S. y cols., Periendoscopic management of direct oral anticoagulants: a prospective cohort study, Gut, 2019; 68: 969‑976
- Takeuchi Y., Mabe K., Shimodate Y. y cols., Continuous anticoagulation and cold SNARE polypectomy versus heparin bridging and hot SNARE polypectomy in patients on anticoagulants with Subcentimeter polyps, Ann. Intern. Med., 2019; 171: 229‑237
- Li D.‑F., Chang X., Fang X. y cols., Colonoscopic post‑polypectomy bleeding in patients on uninterrupted clopidogrel therapy: a systematic review and meta‑analysis, Exp. Ther. Med., 2020; 19: 3211‑3218
- Dong J., Wei K., Deng J. y cols., Effects of antithrombotic therapy on bleeding after endoscopic submucosal dissection, Gastrointest. Endosc., 2017; 86: 807‑816
- Jaruvongvanich V., Sempokuya T., Wijarnpreecha K. y cols., Continued versus interrupted aspirin use and bleeding risk after endoscopic submucosal dissection of gastric neoplasms: a meta‑analysis, Ann. Gastroenterol., 2018; 31: 344‑349
- Seo M., Song E.M., Cho J.W. y cols., A risk‑scoring model for the prediction of delayed bleeding after colorectal endoscopic submucosal dissection, Gastrointest. Endosc., 2019; 89: 990‑998
- Tomida H., Yoshio T., Igarashi K. y cols., Influence of anticoagulants on the risk of delayed bleeding after gastric endoscopic submucosal dissection: a multicenter retrospective study, Gastric Cancer, 2021; 24: 179‑189
- Nagata N., Yasunaga H., Matsui H. y cols., Therapeutic endoscopy‑related Gi bleeding and thromboembolic events in patients using warfarin or direct oral anticoagulants: results from a large nationwide database analysis, Gut, 2018; 67: 1805‑1812
- Andriulli A., Loperfido S., Napolitano G. y cols., Incidence rates of post‑ERCP complications: a systematic survey of prospective studies, Am. J. Gastroenterol., 2007; 102: 1781‑1788
- Dumonceau J.‑M., Kapral C., Aabakken L. y cols., ERCP‑related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) guideline, Endoscopy, 2020; 52: 127‑149
- Lee M.G., Kim J., Lee S.H. y cols., Effect of sustained use of platelet aggregation inhibitors on post‑endoscopic sphincterotomy bleeding, Dig. Endosc., 2014; 26: 737‑744
- Spadaccini M., Fugazza A., Frazzoni L. y cols., Endoscopic papillectomy for neoplastic ampullary lesions: a systematic review with pooled analysis, United European Gastroenterol. J., 2020; 8: 44‑51
- Chung K.H., Lee S.H., Choi J.H. y cols., Effect of submucosal injection in endoscopic papillectomy of ampullary tumor: propensity‑score matching analysis, United European Gastroenterol. J., 2018; 6: 576‑585
- Polkowski M., Jenssen Ch., Kaye Ph. y cols., Technical aspects of endoscopic‑ultrasound (EUS)‑guided sampling. European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline – 2017, Endoscopy, 2017; 49: 989‑1006
- Li D.‑F., Wang J.‑Y., Yang M.‑F. y cols., Factors associated with diagnostic accuracy, technical success and adverse events of endoscopic ultrasound‑guided fine‑needle biopsy: a systematic review and meta‑analysis, J. Gastroenterol. Hepatol., 2020; 35: 1264‑1276
- Ogura T., Nishioka N., Ueno S. y cols., Antiplatelet and/or anticoagulant treatment does not increase hemorrhagic adverse events during EUS‑guided biliary drainage, Gastrointest. Endosc., 2020; 92: 659‑666
- Atukorale Y.N., Church J.L., Hoggan B.L. y cols., Self‑expanding metallic stents for the management of emergency malignant large bowel obstruction: a systematic review, J. Gastrointest. Surg., 2016; 20: 455‑462
- Anderloni A., Di Leo M., Barzaghi F. y cols., Complications and early mortality in percutaneous endoscopic gastrostomy placement in lombardy: a multicentre prospective cohort study, Dige. Liver Dis., 2019; 51: 1380‑1387
- Noujaim M.G., Parish A., Raines D. y cols., Use, yield, and risk of device‑assisted enteroscopy in the United States: results from a large retrospective multicentre cohort, J. Clin. Gastroenterol., 2021; 55: 792‑797
- Biondi‑Zoccai G.G.L., Lotrionte M., Agostoni P. y cols., A systematic review and meta‑analysis on the hazards of discontinuing or not adhering to aspirin among 50 279 patients at risk for coronary artery disease, Eur. Heart J., 2006; 27: 2667‑2674
- Sung J.J.Y., Lau J.Y.W., Ching J.Y.L. y cols., Continuation of low‑dose aspirin therapy in peptic ulcer bleeding: a randomized trial, Ann. Intern. Med., 2010; 152: 1‑9
- Siau K., Hannah J.L., Hodson J. y cols., Stopping antithrombotic therapy after acute upper gastrointestinal bleeding is associated with reduced survival, Postgrad. Med. J., 2018; 94: 137‑142
- Oakland K., Kothiwale S., Forehand T. y cols., External validation of the Oakland score to assess safe hospital discharge among adult patients with acute lower gastrointestinal bleeding in the US, JAMA Netw. Open, 2020; 3: e209 630
- Strate L.L., Orav E.J., Syngal S., Early predictors of severity in acute lower intestinal tract bleeding, Arch. Intern. Med., 2003; 163: 838‑843
- Radaelli F., Dentali F., Repici A. y cols., Management of anticoagulation in patients with acute gastrointestinal bleeding, Dig. Liver Dis., 2015; 47: 621‑627
- Nagata N., Sakurai T., Moriyasu S y cols., Impact of INR monitoring, reversal agent use, heparin bridging, and anticoagulant interruption on rebleeding and thromboembolism in acute gastrointestinal bleeding, PLoS One, 2017; 12: e0 183 423
- Cuker A., Burnett A., Triller D. y cols., Reversal of direct oral anticoagulants: guidance from the anticoagulation forum, Am. J. Hematol., 2019; 94: 697‑709
- Tomaselli G.F., Mahaffey K.W., Cuker A. y cols., 2020 ACC expert consensus decision pathway on management of bleeding in patients on oral anticoagulants: a report of the American College of Cardiology solution set oversight Committee, J. Am. Coll. Cardiol., 2020; 76: 594‑622
- Connolly S.J., Crowther M., Eikelboom J.W. y cols., Full study report of Andexanet alfa for bleeding associated with factor Xa inhibitors, N. Engl. J. Med., 2019; 380: 1326‑1335
- Choudari C.P., Rajgopal C., Palmer K.R., Acute gastrointestinal haemorrhage in anticoagulated patients: diagnoses and response to endoscopic treatment, Gut, 1994; 35: 464‑466
- Little D., Chai‑Adisaksopha C., Hillis C. y cols., Resumption of anticoagulant therapy after anticoagulant‑related gastrointestinal bleeding: a systematic review and meta‑analysis, Thromb. Res., 2019; 175: 102‑109
- Tapaskar N., Pang A., Werner D.A. y cols., Resuming anticoagulation following hospitalization for gastrointestinal bleeding is associated with reduced thromboembolic events and improved mortality: results from a systematic review and meta‑analysis, Dig. Dis. Sci., 2021; 66: 554‑566
- Qureshi W., Mittal C., Patsias I. y cols., Restarting anticoagulation and outcomes after major gastrointestinal bleeding in atrial fibrillation, Am. J. Cardiol., 2014; 113: 662‑668
 Español
Español
 English
English
 українська
українська