Definition, Causes, PathogenesisTop
Otalgia (earache) is a symptom of external ear or middle ear disorders (primary otalgia) or of diseases located outside the ear (secondary otalgia, referred pain).
1. Pathogenesis:
1) External ear inflammation or trauma (these processes are painful due to the dense sensory innervation of the periosteum and skin of the external auditory meatus).
2) Middle ear disorders: Increased pressure (eg, as a result of exudate accumulation caused by acute otitis media [AOM]) or markedly decreased pressure (eg, in Eustachian tube dysfunction) in the tympanic cavity.
3) Referred pain: A result of shared innervation of the ear and other structures of the head and neck by sensory fibers of the same cranial nerves (V, VII, IX, X) or cervical nerves (C2 and C3).
Inner ear disorders do not generally cause pain.
2. Causes:
1) External ear:
a) Diffuse otitis externa, which may be bacterial (most frequently; so-called swimmer’s ear) or fungal; perichondritis.
b) Furuncle of the external auditory meatus.
c) Erysipelas of the auricle.
d) Herpes zoster oticus (Ramsay Hunt syndrome).
e) Allergic dermatitis, contact dermatitis.
f) Mechanical or thermal injury (frostbite, burn).
g) Foreign body or cerumen impaction.
h) Tumors, eosinophilic granuloma, granulomatosis with polyangiitis (Wegener granulomatosis).
2) Middle ear:
a) Inflammation: AOM, exacerbation of chronic otitis media, myringitis bullosa.
b) Mastoiditis.
c) Tumors located in the tympanic cavity or compressing or infiltrating the auditory tube.
d) Eustachian tube dysfunction: Inflammation, tumor, granulomatosis with polyangiitis.
e) Trauma (damage and perforation of the tympanic membrane): Direct mechanical trauma to the tympanic membrane, head trauma, barotrauma (eg, caused by flying, diving, explosions), and acoustic trauma (eg, loud live music).
3) Referred pain (secondary otalgia):
a) Dental problems (the most frequent cause of referred otalgia): Pulpitis, periodontitis, trauma, unerupted third molars.
b) Temporomandibular arthritis or trauma.
c) Inflammatory or degenerative processes in the cervical spine.
d) Neuralgia: Trigeminal neuralgia, cervical neuralgia.
e) Inflammatory processes affecting the structures adjacent to the ear (parotid glands, nose, pharynx, paranasal sinuses, temporal artery).
f) Inflammatory processes in distant structures (pharynx, tonsils, cervical lymph nodes, thyroid gland, peritonsillar abscess or infiltrate).
g) Malignant tumors of the floor of the mouth, laryngopharynx, tonsil, larynx.
h) Aphthous ulcers of the mouth, acute stomatitis, glossitis.
i) Disorders of the esophagus: Esophagitis, gastroesophageal reflux disease (GERD), hiatal hernia, foreign body.
j) Disorders of the larynx: Acute laryngitis, trauma, cricoarytenoid arthritis, laryngeal cancer.
k) Cardiovascular diseases: Myocardial infarction, aneurysm.
l) Other: Torticollis, head and neck tumors and trauma, facial neuritis (Bell palsy).
DiagnosisTop
Otalgia is rarely an isolated symptom. History and physical examination (a thorough examination of the head and neck) facilitate diagnosis:
1) Onset:
a) Sudden onset: Acute illnesses, most frequently AOM or trauma, foreign body.
b) Gradual onset: Disorders of lower dynamics (eg, otitis externa, cerumen impaction, Eustachian tube dysfunction, laryngopharyngeal or laryngeal cancer).
2) Severity and quality:
a) A strong constant or increasing pain, sometimes throbbing: Most frequently AOM, trauma, furuncle of the external auditory canal.
b) Less severe dull pain: Diffuse otitis externa, cerumen impaction, foreign body, chronic otitis media (during exacerbations), Eustachian tube dysfunction, sometimes otitis media with effusion (OME).
c) Short, sharp or stabbing, shooting, or episodic pain: Neuralgia.
d) Pruritus or irritation: Diffuse otitis externa, eczema of the external ear, cerumen impaction, foreign body.
e) Intermittent periodic pain: Referred pain.
3) Duration:
a) Acute pain (up to several days): Acute otitis or trauma. In cases of barotrauma, acoustic trauma, or mechanical trauma to the tympanic membrane, a sharp pain occurs directly after the trauma and spontaneously resolves within 1 to 2 hours. In progressing and untreated AOM, the pain increases in severity until the tympanic membrane is perforated or a drainage procedure is performed.
b) Chronic pain: Chronic otitis externa, foreign body or cerumen impaction, ear tumors, certain types of referred pain.
4) Location:
a) Superficial: Auricle, external auditory canal.
b) Deep: Middle ear.
5) Specific activities and body positions affecting pain severity:
a) Pain is worse in the supine position and when swallowing: AOM.
b) Pain is increased by traction on the auricle, particularly by pressure or traction on the tragus: Otitis externa, furuncle of external auditory canal, erysipelas, perichondritis.
c) Pain is increased during mastication: Otitis externa, furuncle of the external auditory canal, abnormalities of the temporomandibular joint.
6) Characteristic findings of history and physical examination:
a) Fever: Suggestive of infection.
b) Manifestations of upper respiratory tract infection, rhinitis: Suggestive of AOM.
c) Vomiting: AOM or chronic otitis media and its complications.
d) Blocked ear sensation: AOM, OME, cerumen impaction or foreign body in the external auditory canal; Eustachian tube dysfunction (partially improving or completely resolving after the Valsalva maneuver).
e) Hearing loss: Middle ear diseases (AOM, OME, chronic otitis media, trauma), cerumen impaction or foreign body in the external auditory canal.
f) Cough or sneezing: AOM, foreign body in the external auditory canal (cough reflex).
g) Purulent discharge from the external auditory canal: Otitis media (if discharge is associated with a marked improvement or complete resolution of pain, it is suggestive of AOM with tympanic membrane perforation or rupture and evacuation of a furuncle; if the pain persists or intensifies after the appearance of discharge, it is suggestive of diffuse otitis externa; a persistent or recurring foul-smelling discharge that is usually painless is suggestive of chronic otitis media [pain reflects exacerbation of the inflammatory process]).
h) Bleeding from the external auditory canal: Trauma (ruptured tympanic membrane or fractured skull base).
i) Skin lesions in the auricle or adjacent area: Erythema: otitis externa, erysipelas, perichondritis or chondritis, mastoiditis, burn, or mechanical injury. Edema: otitis externa, erysipelas, perichondritis or chondritis, mastoiditis or subperiosteal abscess of the mastoid process, burn or mechanical injury, parotitis, lymphadenitis. Erythematous nodule with an indurated base: furuncle. Vesicular rash: herpes zoster, herpes simplex. Wounds, ecchymoses, and bruising: mechanical injury. Asymmetric protrusion of the auricle: mastoiditis.
Otoscopy should be performed in every patient with ear pain; this study is essential for the identification of the cause of primary otalgia (Figure 1.31-1). If the cause cannot be established, it is necessary to consider diseases that may lead to serious complications (this is usually possible based on history and physical examination): necrotizing (malignant) otitis externa (particularly in patients with diabetes mellitus, immunodeficiency, or in the elderly), cholesteatoma (an abnormal skin growth in the middle ear), temporal arteritis, or even myocardial infarction.
ManagementTop
Management of patients with unexplained otalgia (with no abnormal findings on otoscopy):
1) Patients aged ≤40 years: Consider initial symptomatic treatment. If symptoms persist, perform further diagnostic workup.
2) Patients aged >40 years: Consider temporal arteritis (see Giant Cell Arteritis).
3) Patients aged >50 years or with symptoms or risk factors for cancer (smoking, excessive alcohol consumption, dysphagia, weight loss, chronic hoarseness, exposure to ionizing radiation): Refer to an ear, nose, and throat (ENT) specialist for assessment, possibly including nasal and laryngeal endoscopy.
FiguresTop
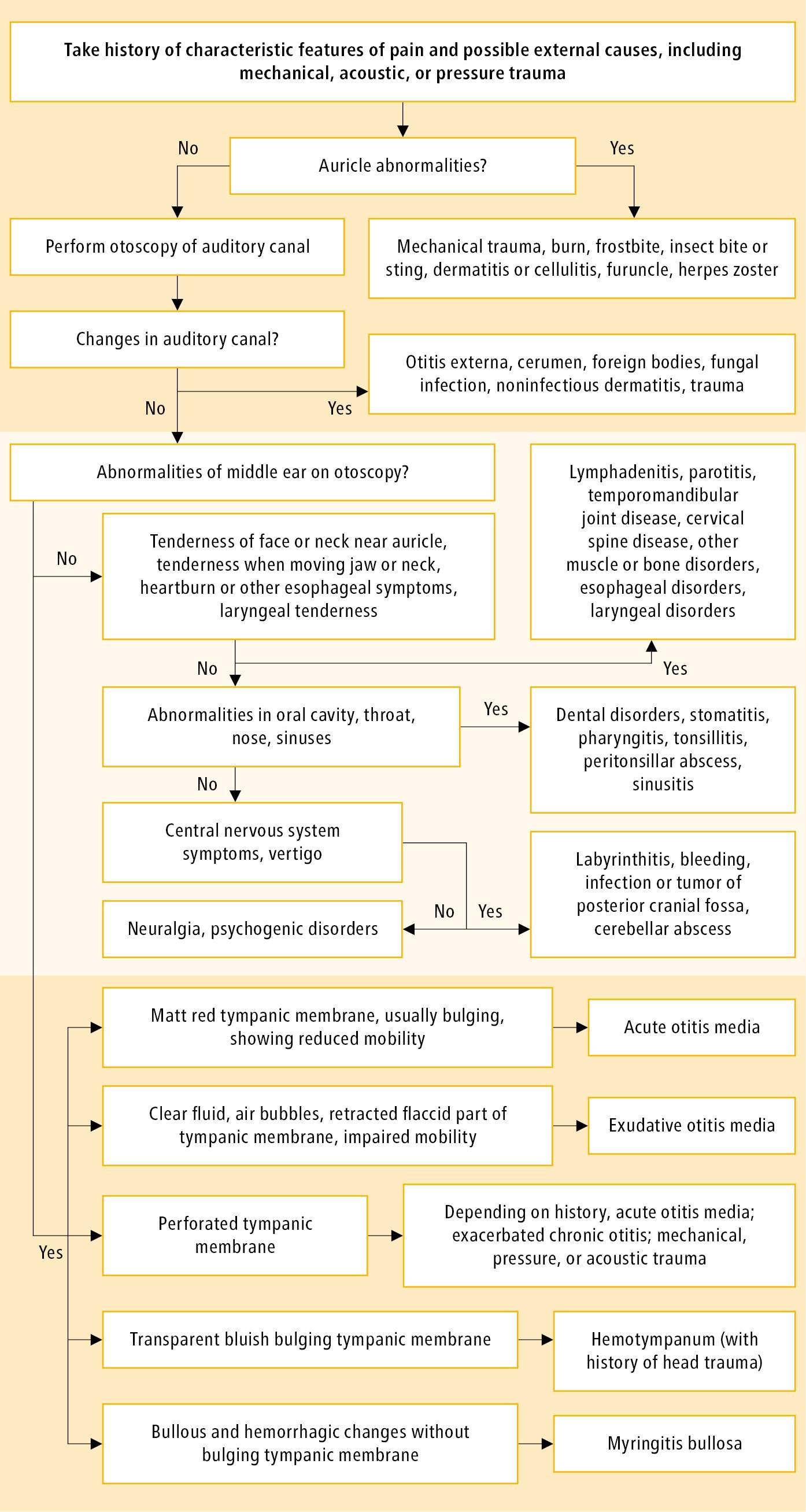
Figure 1.31-1. Diagnostic algorithm for otalgia in adolescents and adults.