Valent P, Akin C, Hartmann K, et al. Updated Diagnostic Criteria and Classification of Mast Cell Disorders: A Consensus Proposal. Hemasphere. 2021 Oct 13;5(11):e646. doi: 10.1097/HS9.0000000000000646. PMID: 34901755; PMCID: PMC8659997.
Gotlib J, Gerds AT, Bose P, et al. Systemic Mastocytosis, Version 2.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2018 Dec;16(12):1500-1537. doi: 10.6004/jnccn.2018.0088. PMID: 30545997.
Mastocytosis Society Canada website. https://www.mastocytosis.ca/enDefinition, Etiology, PathogenesisTop
Mastocytosis is a group of disorders characterized by the proliferation and accumulation of mast cells in one or more organs. Types of mastocytosis include:
1) Cutaneous mastocytosis (CM), which may have the form of a maculopapular rash (urticaria pigmentosa), diffuse CM, or mastocytoma of skin.
2) Systemic mastocytosis (SM), which may be indolent SM, smoldering SM, SM with an associated hematologic neoplasm, aggressive SM, or mast cell leukemia.
3) Mast cell sarcoma.
Clinical Features and Natural HistoryTop
1. Cutaneous manifestations: Yellow-brown or red-brown macules and pruritic papules (Figure 9.4-1, Figure 9.4-2), Darier sign (urticaria appearing within minutes after stimulation of the skin affected by the lesions; Figure 9.4-3).
2. Symptoms caused by mast cell mediator release: Hypotension, tachycardia, syncope, headache, and shock (due to vasodilation); dyspnea (due to bronchoconstriction); flushing; bone pain, osteopenia and osteoporosis; fatigue, weight loss, cachexia; dyspepsia, diarrhea, and symptoms of peptic ulcer disease; depression, mood changes, lack of concentration, increased somnolence; bleeding.
Triggering factors: Drugs (eg, acetylsalicylic acid [ASA], morphine, nonsteroidal anti-inflammatory drugs [NSAIDs]), physical factors (heat, cold, pressure), physical activity, alcohol, insect venom, iodinated contrast agents, stress, invasive procedures.
3. Symptoms caused by tissue and organ infiltration: Hepatosplenomegaly, lymphadenopathy, diarrhea, and weight loss (due to malabsorption); features of anemia; bleeding; pathologic fractures; other organ-specific signs and symptoms.
DiagnosisTop
1. CM: Histologic examination of skin biopsy specimens.
2. SM: Bone marrow examination (Figure 9.4-4), biopsy of the skin or other affected organs, molecular studies (KIT D816V mutation), high serum tryptase levels.
3. Mast cell leukemia: Over 20% mast cells in bone marrow, >10% mast cells in peripheral blood, or organ infiltrates, frequently without cutaneous lesions.
Differential diagnosis should include nonclonal mast cell activation syndromes, idiopathic anaphylaxis, chronic spontaneous urticaria, hereditary or acquired angioedema, carcinoid syndrome, pheochromocytoma, and vasoactive intestinal peptide-secreting tumors.
TreatmentTop
1. General measures:
1) Due to the risk of anaphylactic shock, the patient should be advised of the factors that may trigger mast cell degranulation, learn the ways to avoid them, and carry at least 2 epinephrine autoinjectors.
2) Agents that may trigger mast cell degranulation (eg, opioids, ASA and NSAIDs, radiocontrast dye, some muscle relaxants) should be used with caution.
3) Beta-blockers can make anaphylaxis more severe and more difficult to manage and should be avoided where possible.
4) Before invasive medical or surgical procedures, administration of a prophylactic H1 antagonist, H2 antagonist, and glucocorticoid is suggested. A leukotriene antagonist can also be used.
5) If the patient has a coexisting insect venom allergy, they should be treated with venom immunotherapy.
2. CM, indolent and smoldering SM: Symptomatic treatment only, including H1 antihistamines, H2 antihistamines, leukotriene modifiers, omalizumab, proton pump inhibitors in the case of dyspepsia or peptic ulcer disease, topical glucocorticoids, psoralens with ultraviolet light in the A range (PUVA) photochemotherapy, mast cell stabilizers (cromolyn), calcium and vitamin D, and bisphosphonates. Interferon alpha-2b is used in the case of severe bone disease or progressive hepatosplenomegaly.
3. SM with an associated hematologic neoplasm: Treatment of the associated hematologic disorder.
4. Aggressive SM: The first-line agents are midostaurin, cladribine, and interferon alpha-2b. Imatinib mesylate may be considered in patients who are negative for KIT D816V mutation. Allogeneic hematopoietic stem cell transplant (HSCT) is used in selected patients.
5. Mast cell leukemia: Midostaurin, multidrug chemotherapy (as in acute myeloid leukemia), or cladribine, which may be combined with interferon alpha (chemotherapy is of limited efficacy); allogeneic HSCT.
PrognosisTop
In adults, spontaneous remissions are rare. Patients with CM, indolent SM, or smoldering SM in general respond well to symptomatic treatment and have normal life expectancy. The prognosis in patients with aggressive SM is variable, with a median survival of a few years. In patients with mast cell leukemia, the prognosis is poor.
FiguresTop

Figure 9.4-1. Mastocytosis: macules on the back.

Figure 9.4-2. Cutaneous manifestations of mastocytosis.

Figure 9.4-3. Positive Darier sign. Figure courtesy of Dr Magdalena Lange.
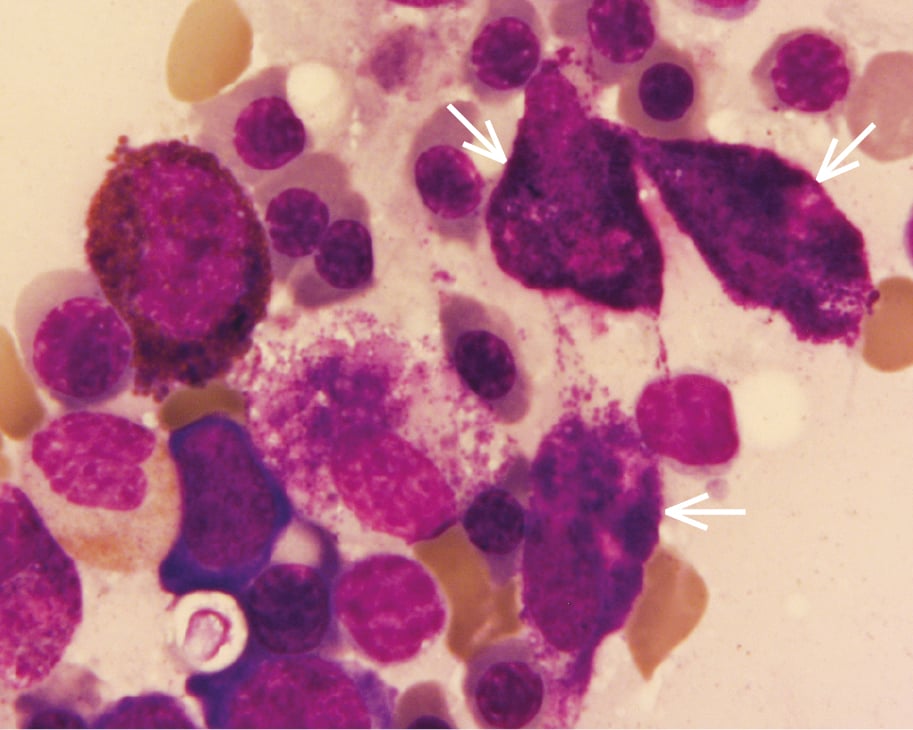
Figure 9.4-4. Mastocytosis: bone marrow smear, visible pathologic mastocytes (arrows; Pappenheim stain).