DefinitionTop
Bone and joint dysplasias (osteochondrodysplasias) are caused by abnormal osteogenesis, chondrogenesis, and other disorders of growth and development of the shafts (diaphyses), metaphyses, epiphyses, and epiphyseal (growth) plates of premature long bones and vertebral bodies. They frequently lead to peripheral joint and spinal dysfunction.
EpidemiologyTop
The prevalence of a vast majority of bone and joint dysplasias is very low (1/10,000-50,000 births). The most common forms in adults are developmental dysplasia of the hip (DDH) and Scheuermann disease.
Etiology and PathogenesisTop
Most dysplasias are caused by genetic mutations or deficiencies of proteins participating in bone formation.
Clinical FeaturesTop
Several types of dysplasia are distinguished depending on location of the predominant growth abnormalities: epiphyseal, metaphyseal, diaphyseal, and chondrodysplasia (epiphyseal growth plate dysplasia) (Figure 18.5-1).
Epiphyseal DysplasiasTop
1. DDH: A developmental disorder affecting the femoral head and acetabulum. Undiagnosed or mistreated DDH manifests in adults with early degenerative and proliferative changes that cause pain, limb shortening, decreased joint range of motion, and reduced mobility. Typical radiographic findings include a shallow and steep acetabulum and flattened femoral head (Figure 18.5-2). The treatment of choice in adults is hip arthroplasty.
2. Spondyloepiphyseal dysplasias: Besides the changes in long bone shafts, this group of dysplasias is characterized by platyspondyly (flattened vertebral bodies with a reduced anterior-posterior dimension), which results in a short neck and trunk.
3. Scheuermann disease (vertebral osteochondritis): The disease affects the thoracic or lumbar spine. The underlying cause is abnormal ossification of the (cartilaginous and bony) vertebral endplate. The contents of the nucleus pulposus protrude through the weak endplate into the spongy bone of vertebral bodies, which is visible on radiographic imaging as Schmorl nodules. A wedge-shaped deformity of vertebral bodies is also present, leading to thoracic kyphosis (Figure 18.5-3). The disease typically manifests at puberty. In 60% of cases back pain occurs. Treatment is conservative (physical rehabilitation, analgesics), and surgery is rarely needed. In adults the pathologies predispose to early degeneration of disks (degenerative disk disease) and vertebral bodies (Figure 18.5-4).
1. Hypophosphatasia (HPP): Next to radiographic findings, the disorder is characterized by very low serum alkaline phosphatase (ALP) activity (diagnostic criterion) as well as increased serum concentration and urinary excretion of phosphoethanolamine. In adult patients with radiographic bone abnormalities and accompanying bone and joint pain, differential diagnosis should include osteomalacia.
2. Craniometaphyseal dysplasia: The bone pathologies lead to scoliosis, valgus knees, pathologic fractures, arthralgia, and muscular weakness. Cranial sclerosis, ocular hypertelorism, and flat nasal bridge are observed.
1. Brittle bone disease (osteogenesis imperfecta): A group of diseases characterized by bone frangibility and blue sclerae that are mostly inherited in an autosomal dominant manner. Over 90% of patients have a mutation of one of type I collagen genes. In 50% of individuals the disease follows a mild course. In the remaining cases multiple fractures are common, particularly in lower extremities, resulting in short stature. Ligamentous laxity leads to hypermobility of joints and spinal deformities.
2. Nonhereditary idiopathic diaphyseal hyperplasia: Arthralgia manifests in late childhood or early adulthood and is accompanied by limited joint mobility, contractures, growth disturbance, and foot deformities.
1. Achondroplasia: A developmental anomaly of the epiphyseal cartilage inherited in an autosomal dominant manner. Typical features include greater proximal than distal limb shortening with a normal trunk length (short-limbed dwarfism). Other distinctive features include a large head, bulging forehead, midfacial hypoplasia, and lumbar hyperlordosis.
2. Enchondromatosis (Ollier disease): Acquired dysplasia of epiphyseal plates characterized by their proliferation, nonresorption, and ossification in the course of development of metaphyseal and diaphyseal long bones. The ossifying cartilage causes deformities, shortening, and pathologic fractures of bones. In 20% of cases malignancies develop, the most common being chondrosarcoma.
Natural HistoryTop
Most dysplastic syndromes are diagnosed incidentally, based on clinically insignificant radiographic findings. Characteristic phenotypic traits are found in some adults, with pain and motor dysfunction. Some of the dysplasias are associated with poor prognosis due to rapidly progressing abnormalities in joints and other organs or elevated risk of premature death.
DiagnosisTop
Diagnosis is made based on imaging: radiographic findings or, in some cases, ultrasonography, computed tomography (CT), or magnetic resonance imaging (MRI) of the musculoskeletal system. Bone biopsy or biochemical tests are rarely needed. Characteristic phenotypic traits may be present.
Other conditions and syndromes causing joint pain and dysfunction.
TreatmentTop
No effective treatment exists for most bone dysplasias. Management is focused on analgesia as well as prevention of complications and disability through physical therapy and corrective surgery. As the majority of dysplasias are congenital, genetic counseling plays a major role.
ComplicationsTop
1. Musculoskeletal system:
1) Premature degenerative and proliferative changes.
2) Subluxations of joints.
3) Pathologic fractures.
4) False joints.
5) Slipped epiphysis.
6) Limb shortening.
7) Flexion contractures.
8) Muscular weakness.
9) Malignancies (osteosarcoma, chondrosarcoma).
2. Other systems and organs:
1) Malabsorption.
2) Anemia.
3) Nerve palsies.
4) Hearing impairment.
5) Aneurysms.
6) Internal bleeding.
7) Recurrent lung infections.
8) Pneumothorax.
9) Venous thromboembolism.
FiguresTop
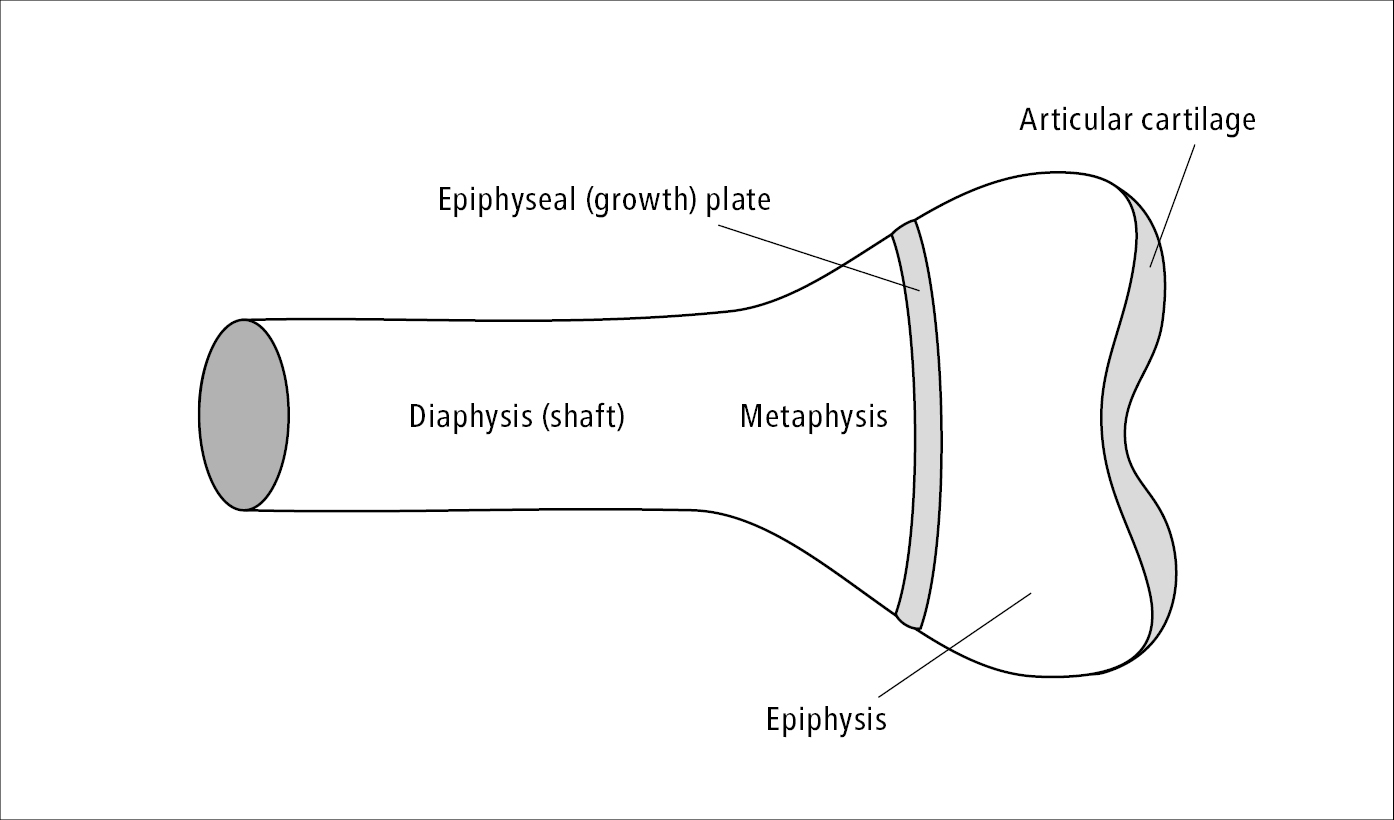
Figure 18.5-1. Schematic drawing of a long bone.
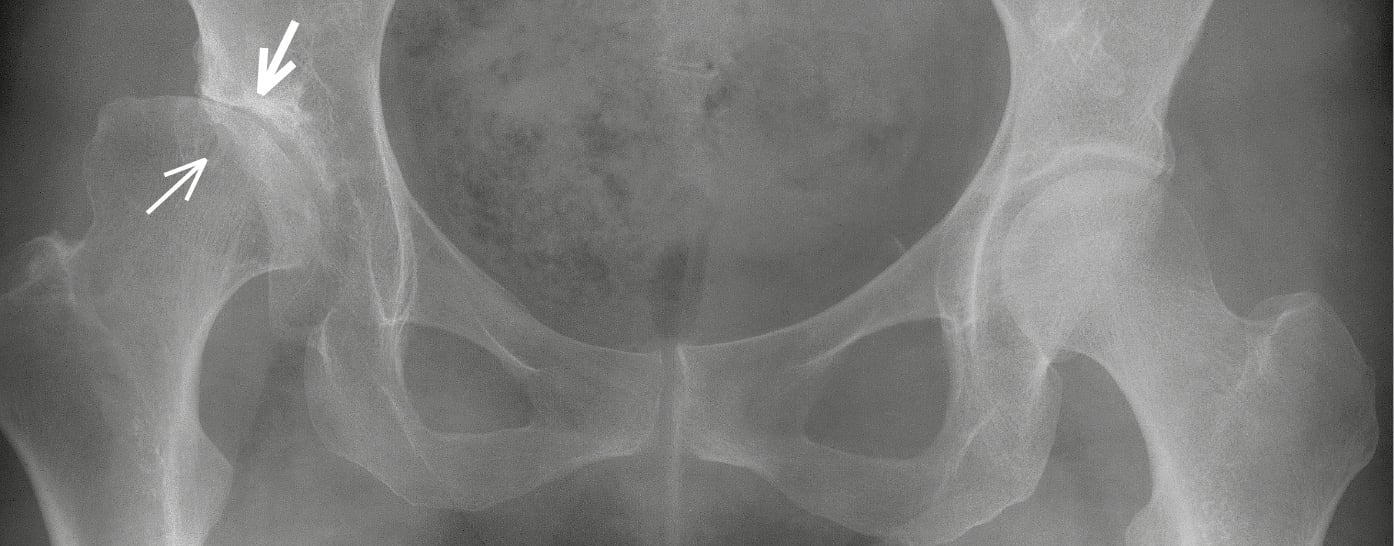
Figure 18.5-2. Right hip dysplasia: a shallow and steep acetabulum; flattened right femoral head, mostly outside of the socket, superolateral joint space narrowing, sclerosis in the subchondral bone at the site of the most pronounced joint space narrowing (thick arrow), a large degenerative cyst with sclerotic margins in the femoral head at the site of the greatest joint load (thin arrow), femoral head subluxation, left hip unremarkable.

Figure 18.5-3. Scheuermann disease. Thoracic spine. A wedge-shaped deformity of vertebral bodies visible in the mid-thoracic spine. Increased kyphosis. Irregular outline of vertebral endplates. Unequal intervertebral space height.
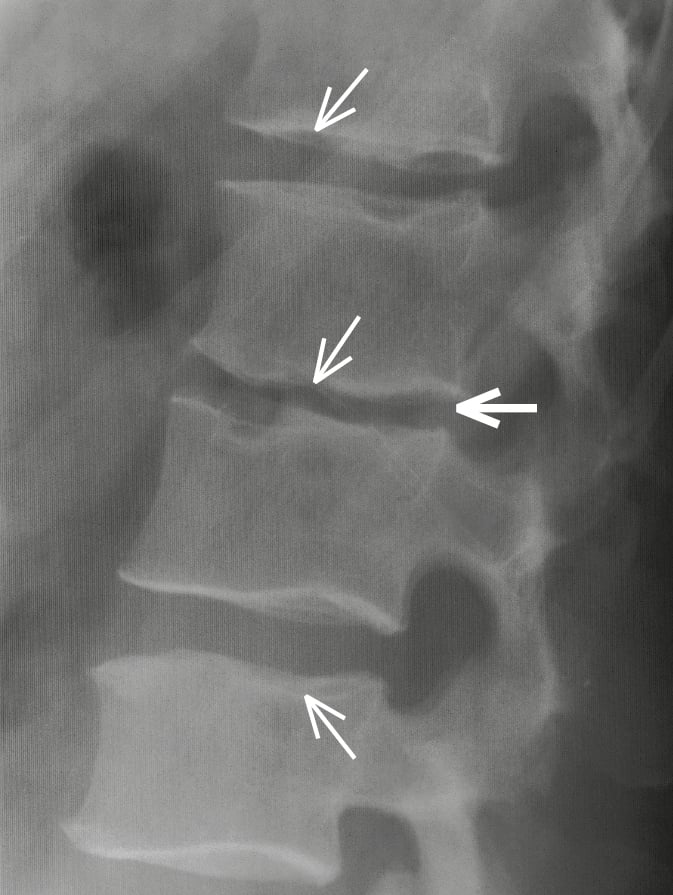
Figure 18.5-4. Secondary degenerative changes in the lumbar spine following Scheuermann disease: irregular endplate outline with Schmorl nodules (thin arrows), narrowed intervertebral space L2/L3 (thick arrow), degenerative hyperplasia seen on vertebral body margins.