DEFINITION, ETIOLOGY, PATHOGENESISTop
1. Epidemiology: Chikungunya fever is present in tropical Asia; Africa; North, Middle, and South America; and on islands of the Pacific and Indian Ocean (Figure 10.11-1). It often causes large epidemic outbreaks, with 30% to 70% of the local population infected with the chikungunya virus (CHIKV). In recent years local CHIKV transmission has also been observed in the south of Europe (France, Italy). In 2019 there were 421 cases of the disease reported in the European Union Member States/European Economic Area, imported by travelers. In late 2013 the first local transmission of chikungunya was identified in the Americas.
2. Etiologic agent: CHIKV, member of the Alphavirus genus, Togaviridae family.
3. Pathogenesis: The virus initially replicates at entry sites, in human skin fibroblasts. This is followed by viremia and dissemination of infection, with accompanying clinical manifestations. The pathogenesis of chronic articular symptoms is not fully known; a role of immune-mediated mechanisms is suggested.
4. Reservoir and transmission: Reservoirs of the pathogen are monkeys and humans. The virus is transmitted by Aedes spp mosquitoes (primarily A aegypti and A albopictus). Bloodborne or vertical human-to-human transmission is possible. CHIKV has never been identified in human breast milk. Transmission by aerosol inhalation during laboratory work involving contact with biologic material that contains CHIKV has been reported.
5. Risk factors: Staying within areas with active CHIKV transmission, particularly during outbreaks and in the wet season.
6. Incubation and contagious period: One to 12 days after a bite of an infected mosquito (3-7 days on average). Patients in the viremic phase (the first 2-6 days after the onset of symptoms) may transmit the virus to mosquitoes.
CLINICAL FEATURES AND NATURAL HISTORYTop
CHIKV infection is asymptomatic in 3% to 28% of patients, depending on the population studied. The most common manifestations include sudden-onset fever (>39 degrees Celsius) and severe pain in multiple joints, most frequently bilateral and symmetrical. Usually hands and feet are affected, but larger joints such as shoulders, hips, and elbows may also be involved. Some patients also report headache, muscle pain, nausea, and vomiting. Physical findings include conjunctivitis and maculopapular rash. Acute manifestations typically resolve within 7 to 10 days. Chronic manifestations of joint involvement—pain persisting for months or years, polyarthritis, tenosynovitis—develop in 5% to 80% of patients (the discrepancy in study results is due to differences in diagnostic criteria and methodology, among other things).
DIAGNOSISTop
1. Identification of the etiologic agent
1) Molecular assays in the viremic phase (blood): Reverse transcriptase–polymerase chain reaction (RT-PCR), reverse transcription loop-mediated isothermal amplification (RT-LAMP).
2) Virus isolation from blood in the viremic phase.
3) Serologic studies: Testing for IgM antibodies, IgG antibodies, or neutralizing antibodies; no earlier than towards the end of week 1 of disease.
2. Other possible nonspecific findings: Thrombocytopenia, leukopenia, elevated blood creatinine concentration, elevated alanine aminotransferase (ALT) and aspartate aminotransferase (AST) activity.
Confirmed diagnosis is possible based on molecular or serologic findings.
Case definitions recommended by the World Health Organization (WHO) during epidemics: www.who.int.
Dengue, Zika virus, malaria, leptospirosis, other Alphavirus infections (Mayaro, Ross River, Barmah Forest, O’nyong-nyong, Sindbis), parvovirus infections, enterovirus infections, rubella, measles, group A streptococcus infections, postinfectious arthritis, other rheumatic diseases.
No antiviral treatment is available. Use antipyretics and analgesics (nonsteroidal anti-inflammatory drugs [NSAIDs]). In dengue endemic areas, acetaminophen (INN paracetamol) is the drug of choice for symptomatic treatment of fever and arthralgia until dengue virus infection is excluded. In patients with chronic joint pain, use NSAIDs, glucocorticoids, and physiotherapy.
COMPLICATIONSTop
Rarely myocarditis, iritis and retinitis, hepatitis, acute kidney injury, bullous skin lesions, meningoencephalitis, Guillain-Barré syndrome, myelitis, cranial nerve palsies.
PROGNOSISTop
The prognosis is good in the majority of patients. Risk factors for a severe course and complications of CHIKV infection are infection during labor, age >65 years, concomitant chronic conditions.
PreventionTop
Vaccination: None available.
1. Mosquito bite protection: Avoiding mosquito bites and eradication of mosquito breeding grounds in tropics.
2. Patient isolation: Not required. Prevention against mosquito bites is to be used in patients in the viremic phase (eg, hospitalization in sealed, air-conditioned rooms equipped with mosquito net canopies) to prevent further transmission.
3. Personal protective equipment (PPE) for health-care professionals: Standard.
FiguresTop
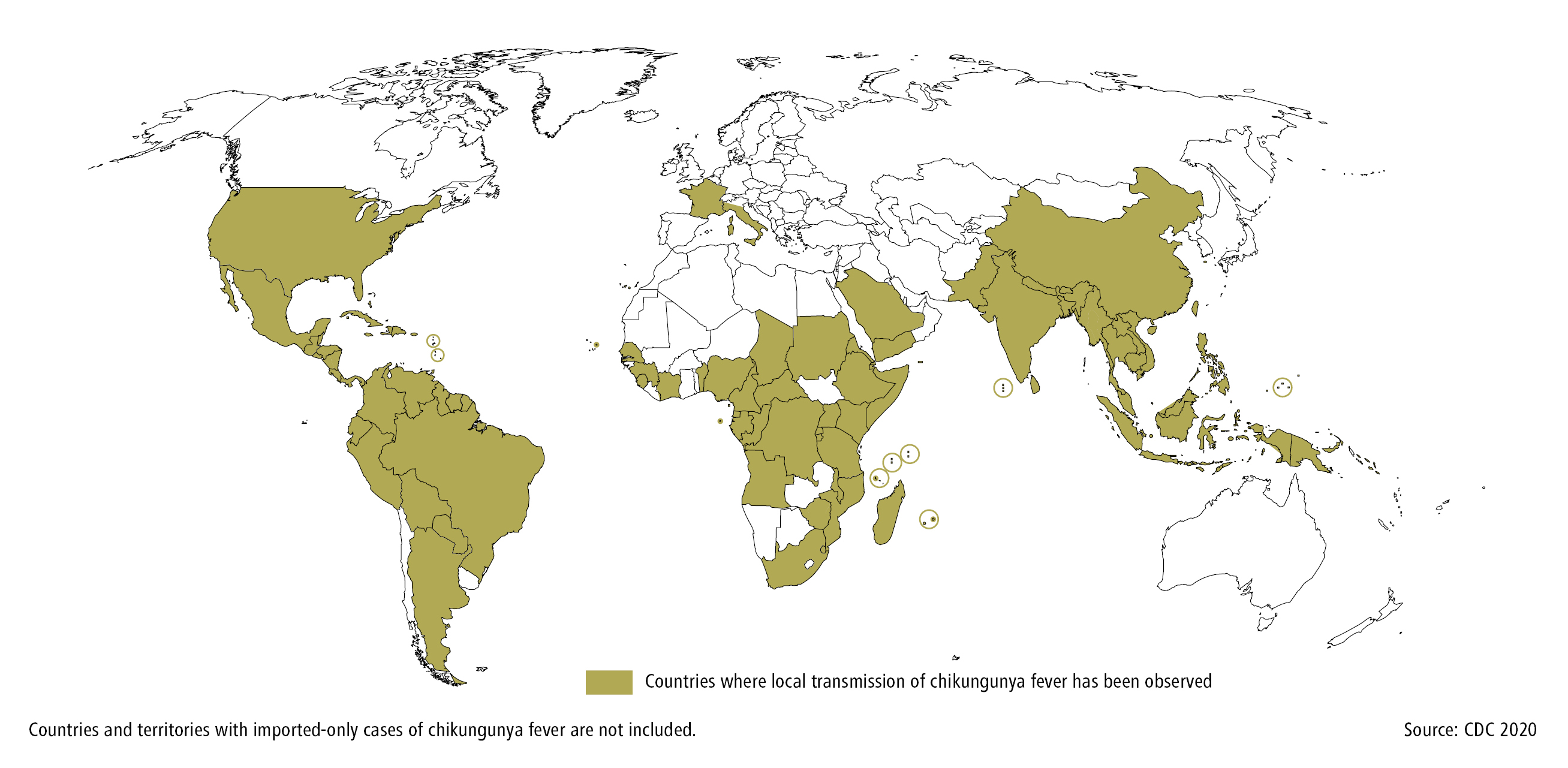
Figure 10.11-1.
Countries with current or previous local transmission of chikungunya fever. Based on CDC 2020.