Definition, Etiology, PathogenesisTop
Anisakiasis is a parasitic disease caused by nematode larvae of the genera Anisakis and Pseudoterranova. The term is broadly used to denote infections with any nematode species belonging to the family Anisakidae.
1. Etiologic agent: Nematodes of the genera Anisakis and Pseudoterranova, primarily A simplex (Figure 10.9-1) and P decipiens (Figure 10.9-2).
2. Pathogenesis: Ingested nematode larvae migrate to the gastric, small intestinal, or—less frequently—large intestinal wall. After 4 to 6 days of infection, the chemoattractants produced by the larvae activate the formation of eosinophilic granulomas in the muscular layer of the gastric or intestinal wall. Penetration of the gastric or intestinal wall might result in migration of the larvae and invasion of other organs. A severe IgE-dependent allergic reaction to the parasite antigens may develop in some patients.
3. Reservoir and transmission: The definitive hosts for Anisakis spp are piscivorous sea mammals, which release nematode eggs into the water. The larvae hatch in the water and are ingested by crustaceans. The nematode larvae found in crustaceans are invasive for the definitive hosts and may also infect fish and cephalopods that prey on crustaceans. Infection in humans is through accidental ingestion of larvae in fish and cephalopods.
4. Risk factors: Consumption of raw or undercooked wild-living fish and cephalopods, such as squids (eg, sushi, sashimi, ceviche, salted fish, cold-smoked fish, cold-pickled fish).
5. Incubation and contagious period: The onset of symptoms may occur 1 to 12 hours following larva ingestion. The patient is not contagious for contacts.
EpidemiologyTop
Anisakid nematodes are cosmopolitan parasites; infected sea animals have been reported in seas and oceans of all geographic regions (Figure 10.9-3). Approximately 200 fish and 25 cephalopod species that may contain Anisakis spp larvae have been identified to date. More than 300,000 cases of anisakiasis have been reported worldwide so far, with the biggest numbers found in Japan.
Clinical Features and Natural HistoryTop
The signs and symptoms depend on the nematode species and the geographic region where the infection occurs. Gastric anisakiasis is the most common type in Japan, while intestinal disease prevails in Europe. Gastric invasion is typically observed in P decipiens infections, which are usually milder than A simplex invasions.
The infection may be initially asymptomatic. In such cases diagnosis is made based on the presence of viable or dead larvae in vomits, usually ~48 hours following the consumption of infected fish.
1. Gastric anisakiasis: Sudden onset of symptoms 1 to 12 hours following ingestion of infested fish: Pronounced epigastric pain, nausea, vomiting, low-grade fever. Rash is rare. Sometimes esophageal invasion is observed—tingling sensation in the throat and cough. Acute symptoms typically resolve within days, but in some patients abdominal pain and nausea may persist for weeks to months.
2. Intestinal anisakiasis: Symptoms appear 5 to 7 days following infection and in most patients persist for a few days. Recurrent or persistent abdominal pain is typically observed; some patients also report nausea and vomiting. Ascites and signs of peritoneal involvement may develop. In rare cases symptoms related to intestinal wall inflammation due to the invasion persist longer.
3. Ectopic (extraintestinal) anisakiasis: Ectopic anisakiasis occurs rarely, if larvae penetrate through the gastric or intestinal wall. The peritoneum, pleura, mesentery, liver, pancreas, ovaries, or subcutaneous tissues may be involved.
4. Allergic reactions: Allergic reactions are most common in A simplex infections and include urticaria, angioedema, and anaphylaxis.
DiagnosisTop
1. Identification of the etiologic agent:
1) Direct identification of nematode larvae in vomits (or during endoscopic examination).
2) Detection of antibodies against the parasite antigens in serum (enzyme-linked immunosorbent assay [ELISA] or latex agglutination test).
3) Detection of IgE antibodies against A simplex in patients with allergic reactions and suspected anisakiasis; interpretation of the test results is difficult due to the cross-reactions with antigens of Ascaris spp and Toxocara canis.
2. Other tests: Eosinophilia and elevated serum IgE are frequent findings.
Anisakiasis can be suspected based on disease manifestations (acute abdominal pain) and information that the patient has recently eaten raw or undercooked fish or cephalopods. Diagnosis is made on the basis of identification of nematode larvae and positive serologic test results.
Gastroduodenal mucositis of other etiologies, peptic ulcer disease, peritonitis of other etiologies, appendicitis, intestinal obstruction.
TreatmentTop
Endoscopic removal of larvae from the gastrointestinal (GI) tract. In gastric and intestinal anisakiasis symptoms may resolve spontaneously. There are limited reports indicating the effectiveness of oral albendazole (400-800 mg once daily for 6-21 days). In rare cases, particularly in extraintestinal anisakiasis, surgical treatment is necessary.
ComplicationsTop
Intestinal obstruction, intussusception and/or perforation of the intestinal wall may rarely develop.
PrognosisTop
The prognosis is good in the majority of patients.
PreventionTop
None.
Avoiding consumption of raw, undercooked, pickled, or salted fish and cephalopods. Proper thermal processing of foods to prevent invasion of the GI tract (this does not prevent allergic reactions to dead A simplex larvae):
1) Boiling fish until a temperature >60 degrees Celsius is maintained for ≥1 minute.
2) Freezing fish at a temperature of at least –20 degrees Celsius for 7 days.
3) Freezing fish at a temperature of at least –35 degrees Celsius for ≥15 hours; or at least –20 degrees Celsius for 24 hours before consumption.
FiguresTop

Figure 10.9-1. Anisakis simplex larva with visible ventriculus.
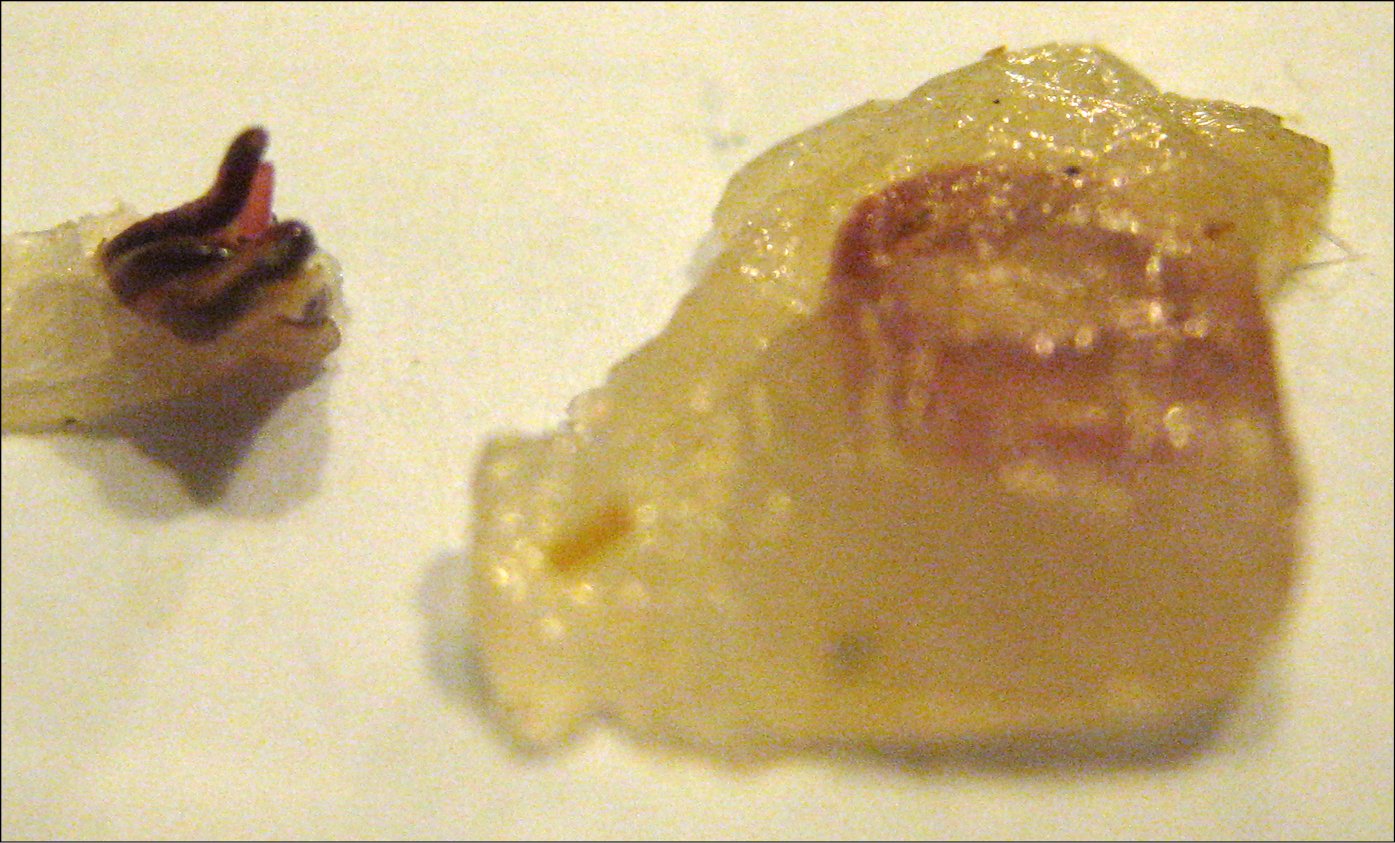
Figure 10.9-2. Pseudoterranova decipiens larvae.

Figure 10.9-3. Larvae of Pseudoterranova decipiens in cod (Gadus morhua callarias) muscles.