DefinitionTop
Blastocystosis is a disease of the large intestine caused by the protozoal parasite Blastocystis hominis.
EpidemiologyTop
B hominis is a cosmopolitan parasite, but invasions are most common in low-income countries with low sanitary standards. It is estimated that in some populations 20% to 40% of individuals are colonized or infected; in Canada this figure is <10%. The parasite is often identified in individuals with HIV infection, patients in psychiatric wards, children attending preschool facilities, and returned travelers.
Etiology and PathogenesisTop
1. Etiologic agent: B hominis, a unicellular eukaryotic organism with undetermined taxonomy and not fully known life cycle. Individual development stages of B hominis are highly diversified, with various morphologic forms including vacuolar, granular, multivacuolar, avacuolar, ameboid, and cyst forms. The predominant form found in stool specimens is the round or oval-shaped vacuolar form (Figure 10.9-1) sized 6 to 40 microm in diameter, with a large central vacuole surrounded by cell nuclei and other peripherally located organelles. The thick-wall cyst is postulated to be the invasive form for humans.
The pathogenesis of blastocystosis remains unclear and the pathogenicity of B hominis is debatable. Cases with intestinal mucosal edema and inflammation and cases with colonic ulcerations have been reported; however, some data suggest that B hominis may be normal flora in those with healthy diets and is in fact associated with better cardiometabolic outcomes.Evidence 1Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to observational nature of data and indirectness. Piperni E, Nguyen LH, Manghi P, et al. Intestinal Blastocystis is linked to healthier diets and more favorable cardiometabolic outcomes in 56,989 individuals from 32 countries. Cell. 2024;187(17):4554-4570.e18.
2. Reservoir and transmission: The primary reservoir of B hominis is humans. Transmission occurs through the fecal-oral route, typically through ingestion of water or foods contaminated with human feces.
Clinical FeaturesTop
The infection is frequently asymptomatic (carriers).
Types of symptomatic disease:
1) Mild blastocystosis: The most common type; manifests with diarrhea (without blood in stool), abdominal pain, nausea, weight loss, and sometimes fine macular rash.
2) Acute blastocystosis: Very rare; typically manifests with watery diarrhea, spastic abdominal pain, and occasionally fever; may lead to gastrointestinal (GI) bleeding.
Irritable bowel syndrome (IBS) has been associated with blastocystosis in some studies, although a causal relationship has not been proven.Evidence 2Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to imprecision the risk of bias and indirectness. Nourrisson C, Scanzi J, Pereira B, et al. Blastocystis is associated with decrease of fecal microbiota protective bacteria: comparative analysis between patients with irritable bowel syndrome and control subjects. PLoS One. 2014 Nov 3;9(11):e111868. doi: 10.1371/journal.pone.0111868. PMID: 25365580; PMCID: PMC4218853.
DiagnosisTop
Diagnosis is made based on microscopic identification of any morphologic forms of B hominis in stool. Repeat stool sampling is usually recommended, several days apart, as the parasite is excreted in shifted temporal patterns and in varying amounts.
Because of the morphologic diversity of the different forms of B hominis, standard direct stool examination should be accompanied by the analysis of permanent trichrome-stained smears.
Polymerase chain reaction (PCR) assays are now available and have high sensitivity and specificity. However, as B hominis is frequently found in asymptomatic individuals and its pathogenicity is not fully known, the significance of a positive PCR test result is debatable. A large observational study of individuals who had PCR testing of stool without reporting results to providers showed that those with Blastocystis species in stool had similar rates of symptoms and referrals to health care as those with negative PCR test results.Evidence 3Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to observational nature of data and indirectness. Shasha D, Grupel D, Treigerman O, et al. The clinical significance of Dientamoeba fragilis and Blastocystis in human stool-retrospective cohort study. Clin Microbiol Infect. 2024 Jan;30(1):130-136. doi: 10.1016/j.cmi.2023.09.003. Epub 2023 Sep 7. PMID: 37689266.
1. Other GI parasitic diseases.
2. Infectious diarrhea.
3. Functional bowel disorders, including IBS.
TreatmentTop
1. Symptomatic treatment: As in infectious diarrhea.
2. Antiprotozoal treatment: B hominis is a saprophytic protozoan largely considered nonpathogenic, and the infection usually does not require specific treatment.Evidence 4Weak recommendation (downsides likely outweigh benefits, but the balance is close or uncertain; an alternative course of action may be better for some patients). Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to imprecision. Cobuccio LG, Laurent M, Gardiol C, et al. Should we treat Blastocystis sp.? A double-blind placebo-controlled randomized pilot trial. J Travel Med. 2023 Feb 18;30(1):taac143. doi: 10.1093/jtm/taac143. PMID: 36440639. Specific treatment is indicated in patients with comorbid conditions such as ulcerative colitis or Crohn disease, in immunosuppressed individuals, and in massive infections.
1) First-line treatment: Metronidazole 500 to 750 mg tid for 10 days or 1.5 g once daily for 7 days; or cotrimoxazole 320/1600 mg once daily or bid in divided doses for 7 days. Some specialists recommend higher doses of cotrimoxazole, 320/1600 mg bid.
2) Alternative treatment: Iodoquinol 650 mg tid for 10 to 20 days, nitazoxanide 500 mg bid for 3 days, paromomycin 500 mg tid for 7 days or 25 mg/kg tid for 10 days, tinidazole 2 g once daily for 5 days.
COMPLICATIONSTop
Invasive colonic disease and GI bleeding may occur in the very rare cases of acute infection. B hominis may cause exacerbations of ulcerative colitis.
PROGNOSISTop
In general the prognosis is good.
PreventionTop
1. Avoiding consumption of contaminated water or food (particularly in tropical areas).
2. Maintaining good personal hygiene.
FiguresTop
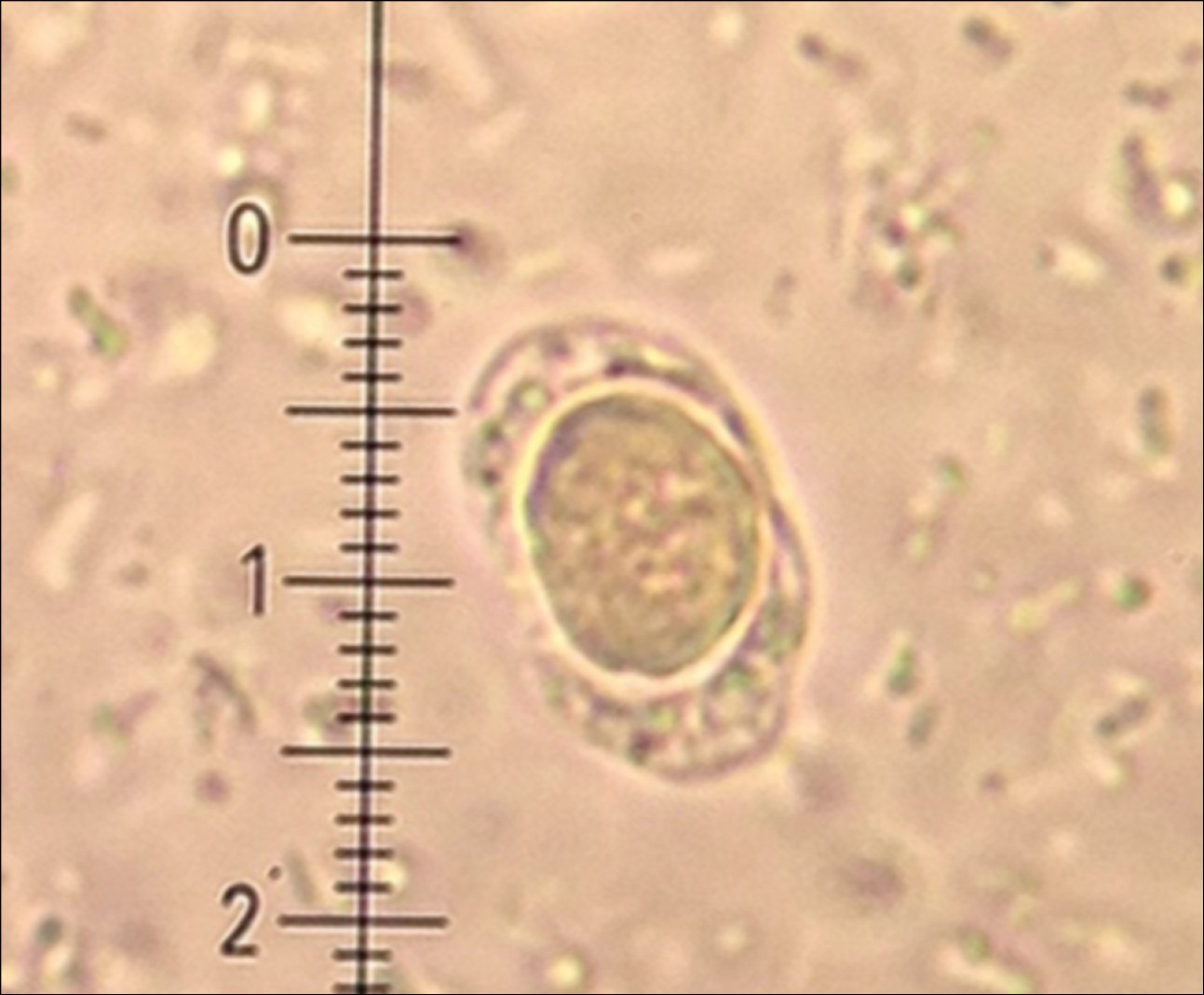
Figure 10.9-1. Vacuolar form of Blastocystis hominis.