Government of Canada Syphilis guide: Treatment and follow-up. Updated April 11, 2024. Accessed June 25, 2024. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/syphilis/treatment-follow-up.html
Workowski KA, Bachmann LH, Chan PA, et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187. doi: 10.15585/mmwr.rr7004a1. PMID: 34292926; PMCID: PMC8344968.
World Health Organization. Guidelines for the management of symptomatic sexually transmitted infections. Updated July 15, 2021. Accessed June 25, 2024. https://www.who.int/publications/i/item/9789240024168
Definition, Etiology, PathogenesisTop
1. Etiologic agent: Treponema pallidum from the order Spirochaetales, family Spirochaetaceae—a spiral gram-negative bacterium with limited metabolic capabilities that lacks lipopolysaccharide in its outer membrane. The organism divides every 30 to 33 hours and cannot survive outside the host’s body.
2. Pathogenesis: T pallidum can invade the host’s tissues using its motility and ability to adhere to multiple types of cells and extracellular matrix proteins. T pallidum also stimulates production of extracellular matrix metalloproteinases in the host’s cells, which facilitates tissue penetration. Cellular and humoral immune responses in syphilis are induced mainly by highly immunogenic proteins of the endoflagella, such as FlaA, FlaB1, FlaB2, and FlaB3.
Dendritic cells, CD4+ and CD8+ cells, and macrophages are primarily involved in the immune response to T pallidum infection. Macrophages participate in phagocytosis and elimination of the bacteria. However, the host’s immune response is insufficient to completely destroy the pathogens. No significant factors affecting the virulence of T pallidum have been identified so far. The majority of syphilitic lesions are likely due to inadequate, enhanced immune response (nonspecific and specific) induced by the bacteria.
3. Reservoir and transmission: The only reservoir is infected humans. The infection occurs as a result of T pallidum penetration through the abraded skin, mucous membranes, placenta (vertical transmission), or bloodstream. Sexual contact is the most frequent transmission route. Nonsexual transmission (eg, incidental rubbing in of infected secretions) is possible but rare, as the bacteria are highly sensitive to external factors. Blood-borne infection due to transfusion of infected blood may occur.
4. Risk factors: As for other sexually transmitted diseases; male sex, living in urban areas, multiple sexual contacts, psychoactive substance and/or alcohol use, chemsex.
5. Incubation and contagious period: Nine to 90 days; usually 21 days. Significant contagiousness is observed in early syphilis (chancres, sepsis due to T pallidum infection) and declines in subsequent stages.
Clinical Features and Natural HistoryTop
Acquired syphilis is classified as early (≤1 year from infection onset) and late (>1 year from infection onset). Irreversible organ damage and resulting symptoms may appear after years. The course of the disease is divided into stages based on manifestations, although manifestations characteristic for a particular stage may also appear at other stages.
1. Early syphilis:
1) Primary syphilis: Occurrence of a primary chancre (primary lesion). The primary lesion appears at the site of T pallidum inoculation. In men it is most frequently located on the coronal sulcus of the penis or on the inner foreskin layer (Figure 10.3-1), and in women, on the labia, posterior commissure, clitoris, or cervix. Chancres may also be found in the anal canal, mouth, or on fingers, depending on the type of sexual contact. Initially they present as infiltrates (primary indurated lesions), which subsequently disrupt and form ulcerations (primary chancre, hard chancre, Hunter chancre). Typically a solitary, painless, oval chancre develops, with smooth margins and a clean base with serous exudate; a base of gristly induration can be felt on palpation. Untypical primary manifestations include herpes simplex virus infection–like, multiple small, erosive, gangrenous, or slit-like lesions and syphilis-related infection of the glans or vulva. A primary chancre heals spontaneously, usually within 2 to 4 weeks, and sometimes causes skin hyperpigmentation or scarring. Symmetrical bilateral regional lymphadenopathy develops several days after primary lesion onset (lymph nodes become hard, painless, and mobile in the surrounding tissue and under the overlying skin; they do not disrupt or form conglomerates). Lesions located in the anal canal and vagina often remain unrecognized.
2) Secondary syphilis: Systemic illness with nonspecific general manifestations and skin lesions; may occur weeks to months after the appearance of a chancre:
a) General manifestations: Fever, headache, myalgia, sore throat, appetite loss.
b) Generalized, painless lymphadenopathy (in the neck, axilla, groin, and thigh).
c) Rash: Early secondary syphilis is characterized by a single type of rash—usually macular or papular, very extensive, and symmetrically distributed; the lesions do not tend to coalesce or group and heal without leaving a trace. Recurrent secondary syphilis presents with different types of rash (macules, papules, pustules), which is less extensive than in early secondary syphilis and nonsymmetrically distributed; the lesions tend to extend peripherally and form groups and may leave scars. Macular rash (Figure 10.3-2) appears at the time of primary chancre occurrence. The most severe lesions are observed on the lateral trunk and medial upper extremities. Lesions do not cause discomfort and often remain unrecognized by the patient. Papular rash (Figure 10.3-3) appears in recurrent secondary syphilis; the lesions are particularly frequently localized on the genitalia and anus (hypertrophied, verrucous, oozing lesions with a wide, infiltrated base, called condylomata lata), palms (Figure 10.3-4), soles, and face (involving the hairline). Pustular rash appears in recurrent secondary syphilis. Papules transform into hard, infiltrated, well-demarcated pustules, which may heal with scarring.
d) Syphilitic leukoderma usually develops in recurrent secondary syphilis in women. Multiple fine macules of >1 cm in diameter, forming a reticular pattern, poorly demarcated from the surrounding skin, appear in the area of the lateral neck and nape of the neck (the so-called necklace of Venus).
e) Syphilitic alopecia may be diffuse (progressive hair loss mainly along the top of the head) or focal (Figure 10.3-5); focal alopecia is typical of recurrent secondary syphilis and manifests as multiple, fine bald patches, mainly in temporal and occipital areas of the scalp, which produce a “moth-eaten” appearance.
f) Mucosal lesions develop in 30% of patients and involve the palatine arches, tonsils, uvula (syphilitic pharyngitis), inner surface of the cheeks, tongue, inner foreskin, and vagina. They present as macules (opalescent) and papules (often infiltrated and oozing, sometimes ulcerative). The lesions are painless and highly infectious. Lesions in late syphilis tend to disintegrate and cause perforation, deformation, and disfigurement.
g) Involvement of other organs is very rare and includes syphilitic interstitial hepatitis manifested by jaundice and increased activity of hepatic enzymes or syphilitic nephropathy with transient proteinuria.
3) Early latent syphilis occurs within the first year of infection and is characterized by serologically confirmed infection without symptoms.
2. Late syphilis:
1) Tertiary syphilis, encompassing cardiovascular syphilis and gummatous disease. Cardiovascular syphilis develops after ≥10 years from infection onset (usually after 15-30 years), more frequently in men than in women. Semilunar aortic valve leaflets and the thoracic aortic wall are commonly affected. Valve involvement usually results in insufficiency. Inflammation of vessels that feed the aorta leads to damage of all layers of the aortic wall and aneurysm formation (a serious complication of syphilis, which does not improve with antibiotics). Gummatous disease is characterized by the presence of (mainly cutaneous) indolent, indurated inflammatory nodules showing a tendency to central necrosis (gummas), with a sticky, jelly-like substance leaking from the central area of the lesion. The nodules spread peripherally (nodular creeping syphilis or nodular-ulcerative syphilis) and form ring-shaped groups, which heal spontaneously in the central part and leave mosaic scars. Gummas may also involve internal organs (mostly the liver and testicles) and bones (particularly at the sites where skin adheres to the bones, eg, on lower legs).
2) Late latent syphilis occurs >1 year after infection and is characterized by serologically confirmed infection without symptoms.
3. Neurosyphilis: Neurosyphilis can occur at any stage of T pallidum infection, that is, both in early and late syphilis. It is classified as early and late:
1) Early neurosyphilis: T pallidum enters the central nervous system (CNS) at the early infection stage, most frequently without any clinical manifestations. Infection may be asymptomatic or present with cerebrospinal meningitis that usually develops within 6 months of infection onset.
2) Late neurosyphilis:
a) Meningovascular syphilis involving the brain and spinal cord: A wide spectrum of signs and symptoms associated with vessel injury in the meninges, brain, and spinal cord, which leads to microstrokes.
b) Parenchymatous syphilis: Progressive paresis usually develops 15 to 20 years after infection onset and causes a psychiatric/neurologic syndrome with typical megalomania, behavioral disorders, hyperactive tendon reflexes; Argyll Robertson pupils may be observed (pupils do not constrict when exposed to light, but the accommodation-convergence reflex is preserved). Syphilitic myelitis (tabes dorsalis) usually develops after 25 years of infection onset and is manifested by sudden attacks of shooting pain in different parts of the body (eg, lower extremities), pain crises—severe visceral pain (eg, in the stomach), superficial sensation disorders, cranial nerve palsy. The lesions are irreversible and do not resolve despite treatment.
c) Gummas of the CNS: Manifestations depend on the location and size of lesions.
d) Ocular syphilis may present with iritis, choroiditis, retinitis, and optic neuritis.
DiagnosisTop
1. Identification of the etiologic agent: T pallidum cannot be detected by culture; therefore, the etiologic agent can be determined only in serologic studies or through direct identification of the organism.
1) Serologic tests are the basic diagnostic method; antibodies are detected in serum and cerebrospinal fluid (CSF):
a) Nontreponemal antibody tests detecting nonspecific IgG and IgM antibodies against a cardiolipin-lecithin-cholesterol complex, which appear 5 to 6 weeks after infection onset: Rapid plasma reagin (RPR), venereal diseases research laboratory (VDRL), and unheated serum reagin (USR) tests.
b) Specific treponemal antibody tests detecting IgG and IgM antibodies against T pallidum antigens: Agglutination tests (T pallidum hemagglutination assay [TPHA] and T pallidum passive particle agglutination assay [TPPA]), enzyme immunoassay (EIA), chemiluminescence immunoassay (CIA), immunoblot assay, fluorescent treponemal antibody absorption (FTA-ABS) test.
c) Rapid point-of-care tests (POCTs): The majority of POCTs detect specific treponemal antibodies; only few of them detect both nontreponemal and treponemal antibodies. With POCTs a single medical consultation is sufficient to establish the diagnosis and initiate treatment. POCTs are crucial for the elimination of cases of congenital syphilis and vertical transmission of T pallidum infection between the mother and child in countries with low-income economies. Due to low sensitivity and specificity, POCTs are not recommended for routine use in countries with access to diagnostic services, where treponemal antibody tests can be performed.
2) Darkfield microscopy of a swab specimen from cutaneous and mucosal lesions that may contain a large number of bacteria; the examination is technically demanding and time consuming and requires highly experienced personnel, specific conditions, and specialized equipment.
3) Molecular testing (polymerase chain reaction [PCR]) is not routinely performed due to suboptimal standardization; it may be of use if there is a suspicion that a primary chancre is localized in the mouth or sites often cohabited by saprophytic treponemes.
4) Detection of treponemes in tissues (immunohistochemistry, in situ hybridization, silver staining): Unavailable in routine clinical practice.
2. Other:
1) CSF examination: Pleocytosis >5 cells/microL, moderately increased protein concentration (<200 mg/dL), decreased glucose levels (<2.2 mmol/L [40 mg/dL]).
2) All patients with syphilis should undergo screening for HIV, hepatitis C virus (HCV), and hepatitis B virus (HBV) infections.
Diagnosis is established on the basis of clinical features and results of serologic tests. To confirm the diagnosis, ≥1 positive nonspecific (nontreponemal) and 1 specific (treponemal) antibody test results are required (Figure 10.3-6). Positive nontreponemal antibody test results indicate active disease, and a decreasing titer reflects an adequate response to treatment. Treponemal antibody titers are not used to monitor response to treatment. Both nontreponemal (often) and treponemal (rarely) antibody tests may give false-positive results (Table 10.3-1). Many laboratories now begin initial testing with a treponemal antibody test followed by a nontreponemal test for confirmation.
CSF examination is the basic method in the diagnostic workup of neurosyphilis. No single test has been considered sufficient to establish the diagnosis. A reactive VDRL test performed on CSF is considered highly specific for the diagnosis of neurosyphilis, but its sensitivity is low. A negative (nonreactive) test result is seen in 70% of patients with neurosyphilis; in such cases the disease is diagnosed based on the presence of inflammatory indicators (pleocytosis ≥5 cells/microL) and reactive treponemal antibodies in CSF.
1. Primary chancre: Chancroid, genital herpes, squamous cell carcinoma, nonspecific genital ulcerations (eg, dermatitis artefacta [factitious dermatitis]).
2. Rash in secondary syphilis: Psoriasis, drug-induced lesions, contact eczema, tinea versicolor.
3. Mucosal lesions: Herpes, leukoplakia, Stevens-Johnson syndrome, streptococcal pharyngitis.
4. Syphilitic leukoderma: Vitiligo, tinea versicolor.
5. Syphilitic alopecia: Alopecia in the course of infectious diseases, scarring alopecia, alopecia areata, toxic alopecia.
6. Late benign syphilis: Lupus erythematosus, sarcoidosis, lupus vulgaris, scarring basal cell carcinoma.
7. Cardiovascular syphilis: Aneurysms of other etiology, atherosclerosis, rheumatic disease, myocarditis.
8. Neurosyphilis: Cerebrospinal meningitis of other etiology, brain tumor, multiple sclerosis, schizophrenia.
TreatmentTop
1. Early syphilis (primary, secondary, or early latent syphilis):
1) First-line treatment: Benzathine penicillin G 2.4 million IU IM as a single dose or as a 1.2 million-IU IM injection into each buttock. IM procaine penicillin G 600,000 IU can be given every 24 hours for 14 days if benzathine penicillin G is unavailable.
2) Alternative treatment (in patients with allergy to penicillin or those who refuse parenteral treatment): Oral doxycycline 100 mg every 12 hours for 14 days or ceftriaxone 1 g IV or IM every 24 hours for 10 days (when close follow-up is assured).
2. Late syphilis (tertiary, late latent syphilis):
1) First-line treatment: Benzathine penicillin G 2.4 million IU IM weekly for 3 weeks.
2) Alternative treatment (in patients with allergy to penicillin or those who refuse parenteral treatment): Oral doxycycline 100 mg every 12 hours for 21 to 28 days. Ceftriaxone 2 g IM or IV every 24 hours for 10 to 14 days.
3. Neurosyphilis (including ocular syphilis and otosyphilis):
1) First-line treatment: IV crystalline penicillin G at a dose of 3 to 4 million IU every 4 hours for 10 to 14 days.
2) Alternative treatment (only if IV administration of crystalline penicillin G is not possible): IM procaine penicillin G 2.4 million IU every 24 hours in combination with oral probenecid 500 mg every 6 hours for 10 to 14 days. In the presence of a penicillin allergy, there are limited data that IV or IM ceftriaxone 1 to 2 g every 24 hours for 14 days can be used as an alternative. Patients with allergy to penicillin should be desensitized. All patients with neurosyphilis should be tested for HIV at the time of diagnosis.
4. Syphilis in pregnancy: Benzathine penicillin G is the only treatment of choice in pregnant patients; dosage should be the same as in other patients, depending on the stage and clinical features of the disease. Pregnant patients with allergy to penicillin should be desensitized. Do not use macrolides (they do not cross the placenta and are therefore ineffective in the treatment of infection in the fetus; they may also induce drug resistance).
Follow-UpTop
Treatment effectiveness or reinfection should be assessed on clinical and serologic follow-up.
In patients with symptomatic syphilis, resolution of clinical manifestations must be confirmed. Clinical and serologic follow-up (nontreponemal antibody testing) after treatment of early syphilis (primary, secondary, early latent) should be performed after 3, 6, and 12 months. Resolution of clinical manifestations and ≥4-fold decline (eg, from 1:32 to 1:8) in nontreponemal antibody titer after 6 months of therapy completion compared with baseline are considered an adequate response to treatment. A negative nontreponemal antibody test result is the best marker of infection resolution. Inadequate response to treatment may indicate CNS involvement or serum resistance.
A serologic response after treatment of late syphilis (tertiary syphilis and late latent syphilis) follow-up testing should be done at 6, 12, and 24 months. Patients with stable (ie, maintained for ≥1 year) low nontreponemal titers after treatment of late latent syphilis do not need further clinical or serologic follow-up.
A ≥4-fold rise in nontreponemal antibody titers indicates reinfection, even if no clinical manifestations are observed. Try to evaluate the infection stage and initiate treatment in those patients.
A follow-up CSF examination should be performed 6 weeks to 6 months after completion of neurosyphilis treatment. Normalization of leukocyte count to <5 cells/microL is considered an adequate response. Repeat examination is recommended every 6 months until the CSF white blood cell count is normal and the nontreponemal test nonreactive.
More frequent follow-up is needed for patients with HIV: 3, 6, 12, 24 months regardless of stage.
In pregnant patients, testing for primary, secondary, and early latent syphilis should be performed monthly until delivery if they are at high risk of reinfection. Testing for late latent syphilis should be performed at the time of delivery and at 12 and 24 months.
ComplicationsTop
1. Adverse effects of treatment:
1) Anaphylactic shock (due to allergy to penicillin).
2) Jarisch-Herxheimer reaction in response to destruction of bacteria after antibiotic therapy and release of pyrogenic cytokines. Clinical features depend on the infection stage:
a) Early syphilis: Fever of up to 41 degrees Celsius, headache, myalgia, arthralgia, exacerbated inflammation in skin lesions.
b) Cardiovascular syphilis: As in early syphilis; myocardial infarction is possible.
c) Neurosyphilis: As in early syphilis; worsening of neurologic manifestations and ischemic stroke are possible.
d) Syphilis in pregnancy: As in early syphilis; premature birth may also occur.
Initiate symptomatic treatment with fluid therapy, antipyretics, and analgesics.
3) Hoigné syndrome may occur after the administration of procaine penicillin G as a result of reflex vasoconstriction following accidental spread of procaine to CNS vasculature. Manifestations include auditory and visual hallucinations, anxiety, and increased arterial blood pressure and resolve spontaneously within 5 to 15 minutes; an IM anxiolytic agent may be used.
2. Primary chancre: Phimosis, paraphimosis, and indurated edema (genital lymphedema due to embolic events evoked by T pallidum).
3. Cardiovascular syphilis: Myocardial infarction, aneurysm rupture, aortic valve insufficiency.
PrognosisTop
Prognosis is good in patients who receive appropriate antibiotic treatment at early stages of infection. Approximately 15% of patients do not develop adequate serologic response to treatment. In 10% of those cases it is due to CNS involvement. The remaining patients are diagnosed with serum resistance; its mechanism and clinical significance have not been elucidated yet.
PreventionTop
1. Vaccination: None available.
2. Pharmacoprophylaxis: Sexual partners of a person diagnosed with early syphilis (symptomatic or latent) should undergo examination. In individuals who had the last sexual contact with an infected person within <90 days, follow a treatment regimen for early syphilis, even if serologic test results are negative. Individuals with negative treponemal antibody test results who had the last sexual contact with an infected person >90 days before do not need treatment.
1. Avoiding high-risk sexual behaviors, limiting the number of sexual partners, using condoms, sexual education.
2. Patient isolation: Not required.
3. Personal protective measures: Standard; it is recommended to follow contact isolation precautions in the case of exposure to primary chancres (highly infectious lesions).
Screening should be performed in blood donors and pregnant women (in the first trimester, between week 28 and 32, and before delivery; both the pregnant woman and her partner should undergo examination).
Tables and FiguresTop

Figure 10.3-1. Primary chancre.

Figure 10.3-2. Macular rash in early secondary syphilis.

Figure 10.3-3. Recurrent maculopapular rash.

Figure 10.3-4. Maculopapular lesions in secondary syphilis. Peripheral desquamation (the so-called Biett collarette) can be observed.

Figure 10.3-5. Focal alopecia in recurrent secondary syphilis.
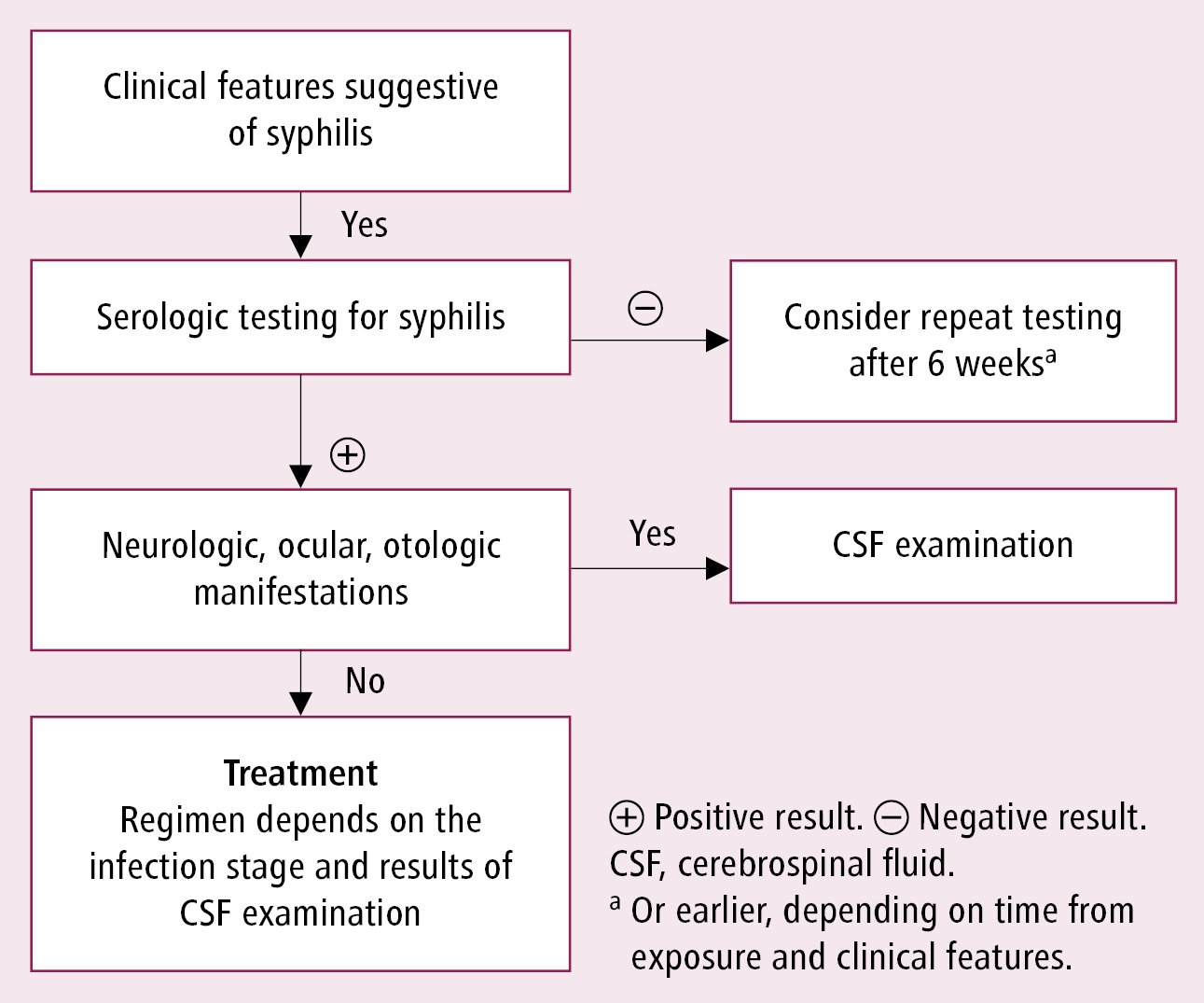
Figure 10.3-6. Diagnostic algorithm for syphilis.
|
Nontreponemal antibody tests |
Treponemal antibody tests | |
|
Positive result persisting for <6 months |
Positive result persisting for ≥6 months |
– Connective tissue diseases – Lyme disease |
|
– After vaccination – After myocardial infarction – Pregnancy – Malaria – Viral hepatitis – Varicella – Measles – Other infectious diseases |
– IV illicit drug use – Autoimmune diseases – Leprosy – Neoplasms – Chronic liver disease – Advanced age | |
|
IV, intravenous. | ||