Baumgartner H, De Backer J, Babu-Narayan SV, et al; ESC Scientific Document Group. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur Heart J. 2021 Feb 11;42(6):563-645. doi: 10.1093/eurheartj/ehaa554. PMID: 32860028.
Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Apr 2;139(14):e637-e697. doi:10.1161/CIR.0000000000000602. PMID: 30586768.
Definition, Etiology, PathogenesisTop
In fetal circulation the foramen ovale provides the necessary anatomic and functional communication between the right and left atria. The foramen ovale closes after birth in ~75% to 80% of people due to increased left atrial pressures. In others it remains patent and is considered a normal anatomic variant.
A patent foramen ovale (PFO) can cause interatrial mainly right-to-left shunting, which can predispose to paradoxical embolization, orthodeoxia-platypnea syndrome (dyspnea and arterial desaturation in the upright position with improvement in the supine position) in susceptible patients, and decompression sickness in divers. The role of PFOs in the pathophysiology of migraines is not well established, however its association has been implicated in a number of retrospective studies.
Clinical Features and DiagnosisTop
The presenting feature may be stroke of undetermined source or a transient ischemic attack, usually in young persons. There is occasional imaging evidence of cerebral embolization without the presence of symptoms. PFOs can be diagnosed using transthoracic echocardiography (TTE) (with Doppler imaging); the sensitivity of detection can be increased using agitated bubble contrast injection with imaging at rest and with the release phase of the Valsalva maneuver. However, the gold standard for PFO detection remains transesophageal echocardiography (TEE) (Figure 3.7-1) with bubble contrast injection at rest and with the release phase of the Valsalva maneuver (leading to transient increase in right atrial pressures and increased right-to-left shunt across the PFO, if present). Transcranial Doppler (TCD) ultrasonography can also be used as a noninvasive alternative for diagnosis. However, TCD can only detect the presence of right-to-left shunting and not the location of this shunt, which can be extracardiac (eg, intrapulmonary).
TreatmentTop
1. In the event of recurrent central nervous system embolism in younger individuals (≤60 years of age) and in the absence of other etiologies after a comprehensive evaluation that should include thrombophilia assessment, the patient can be referred for percutaneous PFO closure, particularly in the case of a coexisting atrial septal aneurysm or large right-to-left shunting observed on TEE.Evidence 1Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to indirectness and imprecision. Saver JL, Carroll JD, Thaler DE, et al; RESPECT Investigators. Long-Term Outcomes of Patent Foramen Ovale Closure or Medical Therapy after Stroke. N Engl J Med. 2017 Sep 14;377(11):1022-1032. doi: 10.1056/NEJMoa1610057. PMID: 28902590. Mas JL, Derumeaux G, Guillon B, et al. Patent Foramen Ovale Closure or Anticoagulation vs. Antiplatelets after Stroke. N Engl J Med 2017; 377:1011. PubMed ID: 28902593Mas JL, Derumeaux G, Guillon B, et al; CLOSE Investigators. Patent Foramen Ovale Closure or Anticoagulation vs. Antiplatelets after Stroke. N Engl J Med. 2017 Sep 14;377(11):1011-1021. doi: 10.1056/NEJMoa1705915. PMID: 28902593. Kuijpers T, Spencer FA, Siemieniuk RAC, et al. Patent foramen ovale closure, antiplatelet therapy or anticoagulation therapy alone for management of cryptogenic stroke? A clinical practice guideline. BMJ. 2018 Jul 25;362:k2515. doi: 10.1136/bmj.k2515. PMID: 30045912; PMCID: PMC6058599.
2. Antiplatelet treatment and prevention of infective endocarditis is necessary for up to 6 months after device closure of the PFO.
FiguresTop
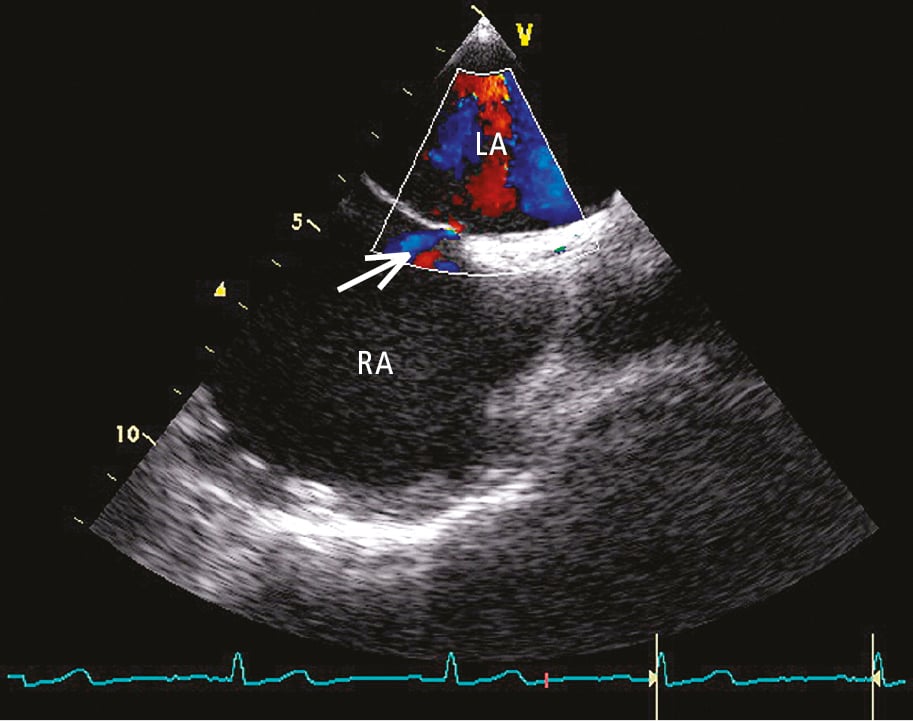
Figure 3.7-1. Transesophageal echocardiography (TEE) with color Doppler, longitudinal view: shunt across a patent foramen ovale (PFO) (arrow). LA, left atrium; RA, right atrium.