Baumgartner H, De Backer J, Babu-Narayan SV, et al; ESC Scientific Document Group. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur Heart J. 2021 Feb 11;42(6):563-645. doi: 10.1093/eurheartj/ehaa554. PMID: 32860028.
Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Apr 2;139(14):e637-e697. doi:10.1161/CIR.0000000000000602. PMID: 30586768.
Definition Top
In fetal circulation the ductus arteriosus connects the proximal left pulmonary artery to the aortic arch immediately distal to the origin of the left subclavian artery, allowing nutrient-rich blood from the mother to bypass the developing lungs. If it fails to close after birth, the patent ductus arteriosus (PDA) causes a left-to-right shunt at the level of pulmonary artery. In adults, this is usually an isolated defect.
Clinical Features and Diagnosis Top
The clinical significance of PDA depends on its size and hence volume of the left-to-right shunt:
1) Small shunt: Usually discovered incidentally by echocardiography, it is asymptomatic and associated with normal pulmonary pressures and normal left atrial and ventricular volumes.
2) Moderate shunt: Exertional dyspnea, reduced exercise tolerance, and palpitations; a continuous murmur in the second left intercostal space, enlargement of the left atrium and left ventricle; pulmonary hypertension may develop, but this is usually reversible after percutaneous intervention or surgery.
3) Large shunt: Rare in adults; adult patients with large shunts usually present at the stage of Eisenmenger syndrome (such patients have a loud second heart sound and no continuous murmur, but they develop differential cyanosis and clubbing, affecting the lower parts of the body and occasionally the left arm depending on whether the PDA joins the aorta before or after the left subclavian artery).
Diagnosis is based on the physical findings and results of echocardiographic evaluation (Figure 1; with magnetic resonance imaging [MRI] and computed tomography [CT] in equivocal cases). However, PDAs can be missed on echocardiography if the pulmonary arteries are not well visualized.
Treatment Top
1. PDA with a continuous murmur: These defects should be closed, preferably using the percutaneous approach. Percutaneous closure is the method of choice and can be performed safely in the vast majority of adults. After invasive treatment, patients without residual hemodynamic disturbances do not need a specialized follow-up. Endocarditis prophylaxis is required in the first 6 months after device closure and in patients in whom there may be residual shunting adjacent to the device, thus not allowing for complete endothelialization.
2. Patients with Eisenmenger syndrome: Medical treatment geared towards complications of Eisenmenger syndrome. Selective pulmonary vasodilators can be used.
FiguresTop
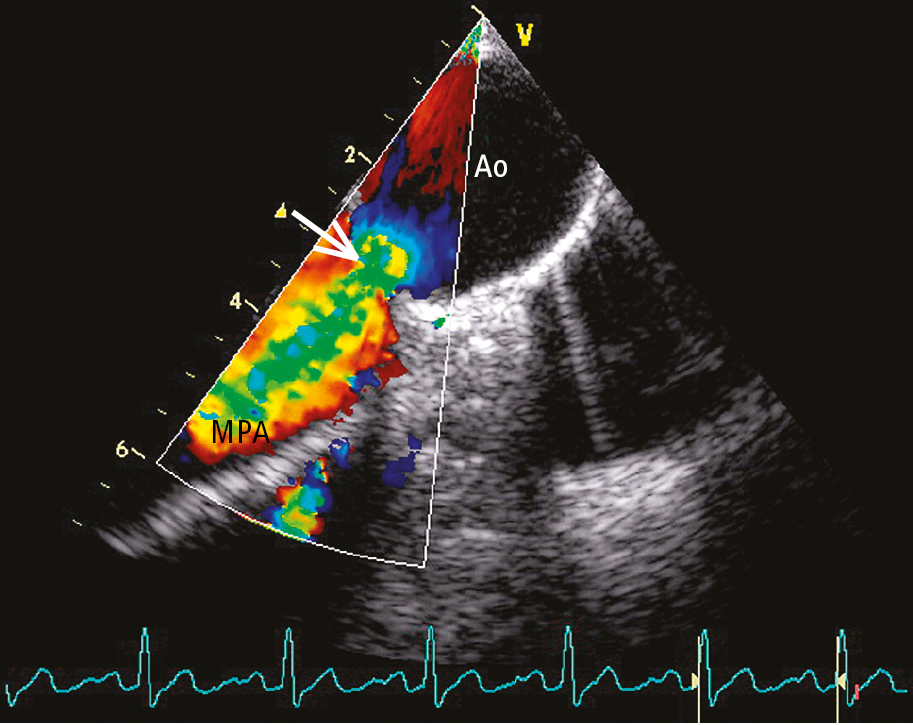
Figure 3.7-1. Transesophageal echocardiography (TEE) with color Doppler in a patient with patent ductus arteriosus (PDA): a left-to-right shunt (arrow). Ao, aorta; MPA, main pulmonary artery.