Definition, Etiology, PathogenesisTop
Thromboangiitis obliterans (TAO), or Buerger disease, is an inflammatory occlusive disease of the small and medium-sized arteries and veins of the extremities and digits (although vascular beds in the entire body have been reported to be affected), which can cause significant tissue loss due to ischemia from progressive vessel occlusion and fibrosis. It is strongly associated with using tobacco and nicotine products, but there are also case reports of it being linked to cannabis use. TAO most commonly presents in men aged <45 years.
The pathogenesis is not clear but likely involves inflammatory, autoimmune, and endothelial factors. Three TAO phases have been described:
1) Acute phase: Inflammatory thrombi in the distal arteries and veins lead to microabscess formation, neutrophilic infiltration, and local inflammation.
2) Subacute phase: Progressive thrombi formation and organization in small to medium vessels with inflammation within the thrombi and progressive ischemia.
3) Chronic phase: Inflammation has resolved, but thrombus formation and fibrosis persist. Differentiation of TAO from atherosclerotic arterial disease is difficult at this stage.
Clinical Features and Natural HistoryTop
1. Symptoms: Disease activity usually begins in the distal arteries and veins and progresses proximally over time with ongoing exposure to tobacco. Typically >1 extremity is involved. Symptoms may be more likely in the winter. TAO tends to flare with intermittent exacerbations and may eventually lead to amputation if there is severe disease.
Secondary Raynaud phenomenon: Increased sympathetic nerve activity and sensitivity to cold lead to triphasic color changes due to progressive cyanosis, which can cause hypoxia if persistent and/or severe. Symptoms tend to be more severe than in primary Raynaud phenomenon and occur in 40% of patients with TAO.
Intermittent claudication: Claudication is not common, but it can occur and may affect smaller areas (fingers, hands) rather than the larger arteries, which are typically affected by atherosclerotic disease.
2. Signs: Physical examination does not distinguish TAO from other forms of peripheral artery disease (PAD).
Migratory superficial thrombophlebitis can occur in 40% of patients with early TAO, usually in the lower limbs. It usually manifests as tender nodules following a venous distribution that correlates with arterial disease activity. Superficial thrombophlebitis is often the distinguishing feature from other occlusive vascular diseases.
Ischemic ulceration (Figure 3.19-1): The poor perfusion of small arteries can cause focal ischemia that often manifests as ischemic ulcers of the lower limbs more often than arms, which are the areas of atrophy, erythema, and possibly dry gangrene from deperfused tissue.
Digit/limb ischemia: In the early stages of ischemia, patients develop paresthesia and neuropathic pain, as nerves are highly sensitive to hypoxia. This can progress to frank ischemia and subsequently to gangrene, which most often affects fingers and toes (as they have the most vulnerable blood supply).
The Allen test (Figure 3.19-2) may be used to test the patency of the arteries at the wrist level (the hand is squeezed tightly to limit blood supply, and then one artery [ulnar or radial] is released at a time to check if blood flow through that artery is sufficient to relieve pallor; see also Arterial Blood Gas Sampling).
DiagnosisTop
1. Laboratory tests may reveal increased erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level, as well as other acute phase reactants, especially in patients with an exacerbation or initial presentation of TAO. An immunologic panel may be considered to distinguish TAO from autoimmune vascular diseases; serologic tests results are negative in TAO. A hypercoagulability screen, antiphospholipid antibodies testing, and toxicology panel for stimulant drugs (cocaine, amphetamines) should also be performed.
2. Measurement of blood pressure in the extremities using a Doppler device (measurement of the ankle-brachial index [ABI] and toe-brachial index [TBI]): ABI can assess occlusion of the arteries of the limbs where pulses are weak or absent. In patients with early TAO, ABI may be normal and TBI should be considered.
3. Imaging studies:
1) Arteriography (Figure 3.19-3) is the imaging modality that is most suggestive of TAO. It can help differentiate TAO from atherosclerotic arterial disease by demonstrating multifocal occlusions and/or vasospasms, as well as collaterals of small peripheral arteries. Other findings consistent with TAO include absence of diffuse atherosclerosis, unexplained thromboembolism, and normal vasculature interrupted by occluded areas with collateralization. Findings of both TAO and atherosclerotic disease may be present, most often in older smokers.
2) Doppler ultrasonography (Figure 3.19-4) can help exclude occlusion of larger vessels that may be inconsistent with TAO and, to a lesser extent, evaluate for atherosclerosis and collateralization.
3) Histologic examination is rarely required, but it is the only definitive diagnostic test. Biopsy of subcutaneous nodules, superficial thrombophlebitis, or pathologic examination of ischemic limbs can demonstrate consistent changes.
There are no universally accepted specific diagnostic criteria for TAO, however, the following features should raise clinical suspicion:
1) Disease onset <50 years of age.
2) Current or recent history of tobacco smoking.
3) Exclusion of autoimmune disease, thrombophilia, diabetes, and embolic diseases.
4) Distal extremity ischemia.
5) Arteriographic findings suggestive of TAO.
6) Involvement of both upper and lower limbs.
7) Superficial thrombophlebitis preceding features of ischemia.
1. PAD: TAO is more distal than PAD and involves upper and lower extremities, while PAD favors the lower limbs.
2. Thromboembolic disease: Patients with thromboembolic disease may have a history of thromboembolic events or other features of thrombophilia, an alternative cause for embolism (eg, atherosclerotic disease, infectious endocarditis). Acute limb ischemia typically does not have a prodrome of Raynaud phenomenon or superficial phlebitis, which is often seen in TAO.
3. Autoimmune disease: Digital ischemia is a feature of certain autoimmune diseases, particularly scleroderma, Raynaud phenomenon, and Takayasu arteritis. However, autoimmune markers should be negative in TAO and symptoms suggestive of other diseases should be absent.
4. Trauma: Some patients with an occupational history that causes repetitive trauma may have small vessel damage. The mechanism of injury should correlate with the location of the vascular injury. There may be associated secondary Raynaud phenomenon, but no other symptoms.
TreatmentTop
An acute episode of TAO requires multifaceted, multidisciplinary therapy. Significant vasospasm may be treated with vasodilators, although the evidence is mostly indirect and of low quality: calcium channel blockers (amlodipine, nifedipine), topical or oral phosphodiesterase-5 inhibitors (eg, sildenafil) or oral phosphodiesterase-3 inhibitors (cilostazol), and/or, if the episode poses a risk of tissue loss, IV prostaglandins or prostacyclins. There may be regional differences in the approved therapies. If microthrombi are thought to significantly contribute to the presentation, anticoagulation with IV heparin may be used. Vascular surgery may be able to provide endovascular repair or bypass, although vessels are often too small to perform such interventions. If ischemia has occurred, supportive care with antibiotics, surgery (often amputation), and/or wound care may exhaust the available options. Immunosuppression is not typically used and is often avoided due to the risk of infection associated with ischemia. Episodes are often painful and require significant analgesia.
The most important step in chronic disease management is avoidance of all tobacco and nicotine products and treatment of nicotine use disorder. Even minimal nicotine exposure can perpetuate disease activity, and cessation of nicotine use can avert the need for any further therapies. Nicotine replacement products should not be used in the management of dependency. Management of the associated Raynaud phenomenon is the same as in other circumstances, with cold avoidance and the use of calcium channel blockers, phosphodiesterase-5 inhibitors, and further therapy as needed. Persistent thrombotic manifestations may be treated with antiplatelets (such as acetylsalicylic acid [ASA]), anticoagulation, or both.
FiguresTop

Figure 3.19-1. Cutaneous manifestations in thromboangiitis obliterans: A, characteristic skin color and trophic toenail lesions; B, hand ulcerations.
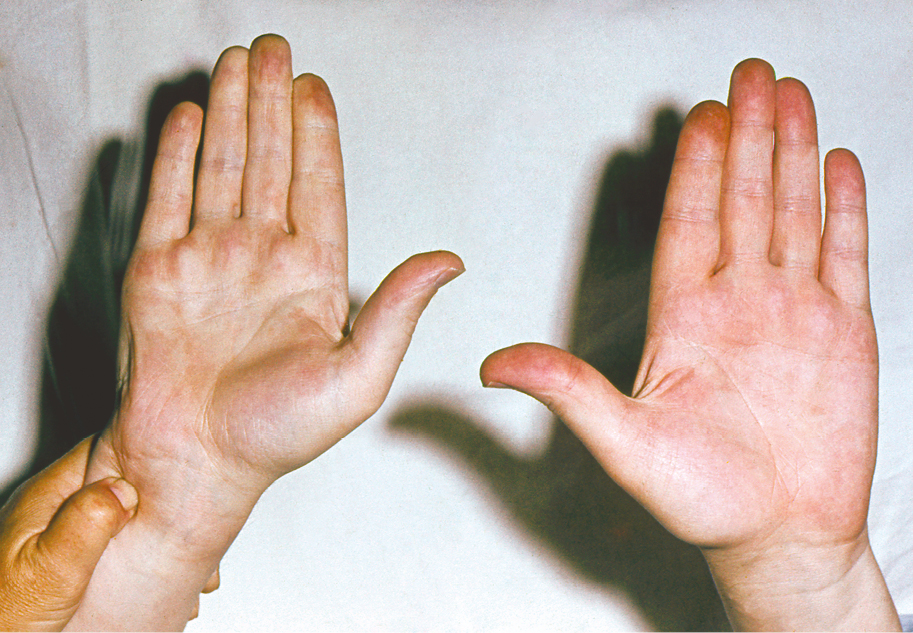
Figure 3.19-2. Testing for the involvement of hand arteries (Allen test).
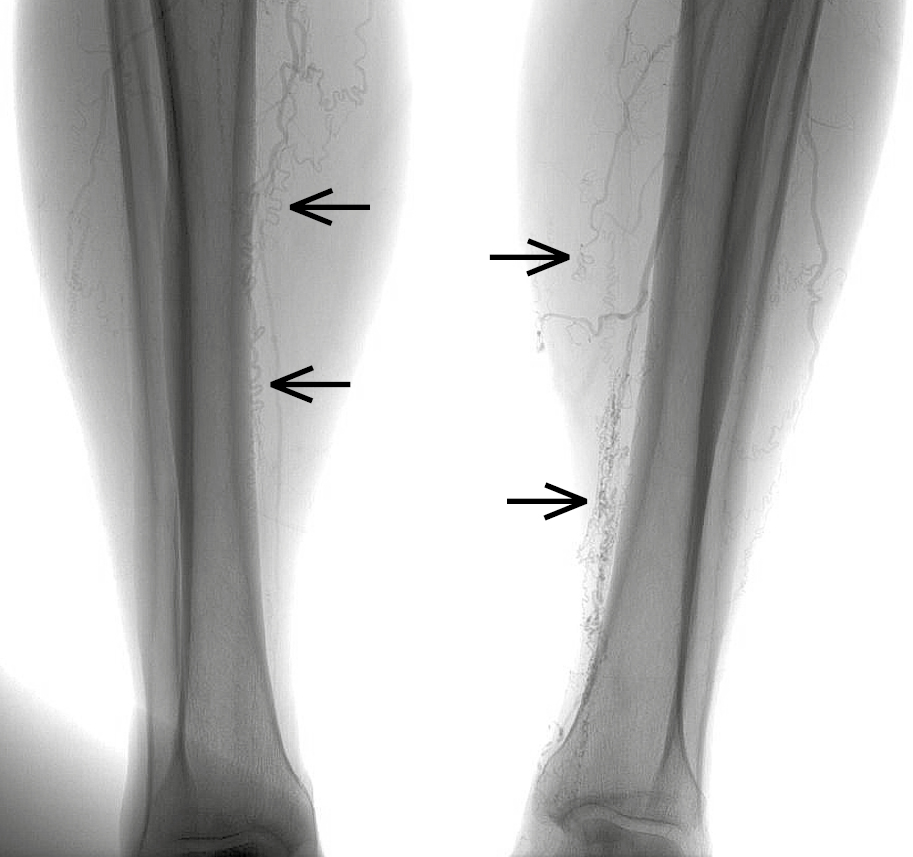
Figure 3.19-3. Thromboangiitis obliterans. Arteriography reveals occluded arteries of the lower leg and typical corkscrew-shaped collateral arteries (arrows).
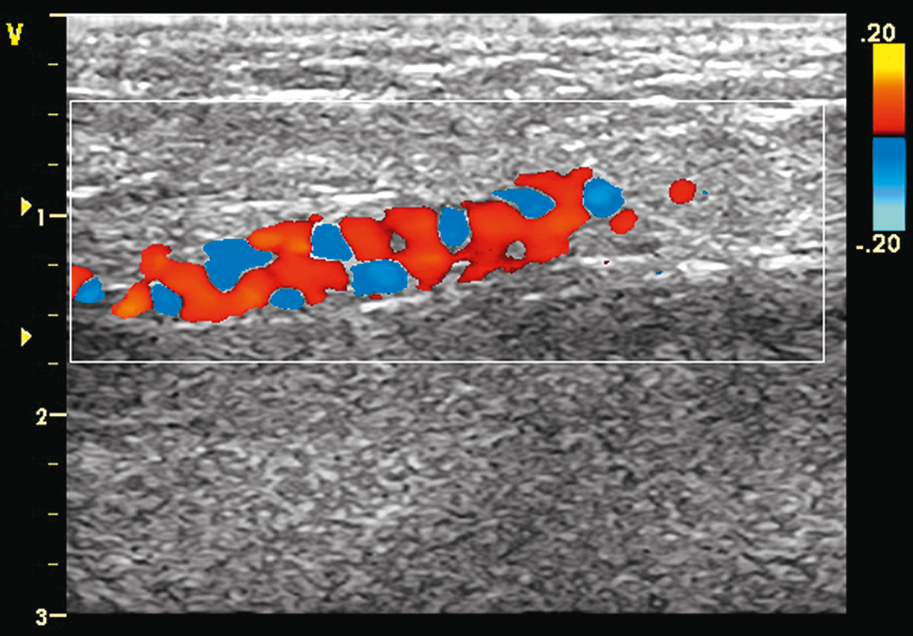
Figure 3.19-4. Color Doppler imaging in a patient with thromboangiitis obliterans: collateral spiral vessels visible at the level of the posterior tibial artery.