Adler Y, Charron P, Imazio M, et al; European Society of Cardiology (ESC). 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC). Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015 Nov 7;36(42):2921-64. doi: 10.1093/eurheartj/ehv318. Epub 2015 Aug 29. PubMed PMID: 26320112.
Sagristà-Sauleda J, Angel J, Sambola A, Permanyer-Miralda G. Hemodynamic effects of volume expansion in patients with cardiac tamponade. Circulation. 2008 Mar 25;117(12):1545-9. doi: 10.1161/CIRCULATIONAHA.107.737841. Epub 2008 Mar 10. PubMed PMID: 18332261.
Roy CL, Minor MA, Brookhart MA, Choudhry NK. Does this patient with a pericardial effusion have cardiac tamponade? JAMA. 2007 Apr 25;297(16):1810-8. Review. PubMed PMID: 17456823.
Little WC, Freeman GL. Pericardial disease. Circulation. 2006 Mar 28;113(12):1622-32. Review. Erratum in: Circulation. 2007 Apr 17;115(15):e406. Dosage error in article text. PubMed PMID: 16567581.
Definition, Etiology, PathogenesisTop
Cardiac tamponade represents the most severe and urgent clinical presentation of pericardial effusion. It occurs when pericardial fluid accumulation exceeds the elastic limit of the pericardium, resulting in significantly elevated intrapericardial pressures. Cardiac tamponade is a life-threatening condition resulting from a slow or more rapid compression of cardiac chambers due to the accumulation of content in the pericardium (inflammatory/malignant exudates, pus, blood, clots, or gas).
Causes:
1) Pericarditis (eg, idiopathic; viral; other infectious, including tuberculous pericarditis in resource-limited countries where tuberculosis is endemic).
2) Iatrogenic (eg, related to invasive procedures, as in the case of complications related to percutaneous coronary intervention [PCI], atrial fibrillation ablation, pacemaker lead insertion; postpericardiotomy syndrome after cardiac surgery).
3) Neoplasm/malignancy (eg, metastatic breast or lung cancer, lymphoma, melanoma).
4) Trauma.
5) Systemic autoimmune disease (eg, systemic lupus erythematosus, rheumatoid arthritis, scleroderma).
6) Myocardial infarction.
7) Radiation therapy.
8) Uremia.
9) Myxedema/hypothyroidism.
10) Aortic dissection.
Clinical Features and Natural HistoryTop
1. Symptoms: Dyspnea; reduced exercise tolerance; sometimes cough, dysphagia, syncope or presyncope.
2. Signs: Most common signs include tachycardia (may be absent in patients with hypothyroidism or uremia), pulsus paradoxus with a systolic arterial pressure drop >10 mm Hg with inspiration, an enlarged cardiac silhouette on chest radiography (before pericardiocentesis: Figure 3.5-1; after pericardiocentesis: Figure 3.5-2), and jugular venous distention. Other signs include diminished or muffled heart sounds, hypotension, and tachypnea.
3. Natural history: Slowly accumulating effusions cause gradual distension of the pericardium, which allows the accumulation of large pericardial effusions (often ≥1 L). In the case of rapidly accumulating effusions or reduced pericardial elasticity, the intrapericardial pressures increase promptly and lead to cardiac tamponade with as little as a few hundred mL of fluid. Cardiac tamponade can lead to obstructive shock and cardiac arrest.
DiagnosisTop
1. Electrocardiography (ECG) may occasionally be normal but usually reveals sinus tachycardia. Other potential findings include low QRS voltage (<5 mm in limb leads and <10 mm in precordial leads), electrical alternans of the QRS complex (Figure 3.5-3), or both. The end-stages of tamponade are associated with bradycardia, and death is due to pulseless electrical activity (PEA).
2. Chest radiography may demonstrate enlargement of the cardiac silhouette without features of pulmonary congestion. In patients with acute cardiac tamponade the cardiac silhouette may be normal.
3. Echocardiography (Figure 3.5-4) is the key diagnostic study for evaluating cardiac tamponade, as recognizing tamponade ultimately remains a clinical diagnosis. In patients with suspected cardiac tamponade an echocardiogram should be performed without delay. Transthoracic echocardiography (TTE) can evaluate for the presence of pericardial fluid, and if present, it can also evaluate the size (>20 mm is considered large [Figure 3.5-5]) and hemodynamic consequences. In large effusions the heart can be seen “swinging” within the pericardial space.
Key echocardiographic signs of cardiac tamponade physiology include:
1) Chamber collapse:
a) Right atrial collapse in late atrial diastole or early atrial systole (more than one-third of the cardiac cycle) is a highly specific and sensitive finding. Left atrial collapse can also be seen and is specific for tamponade.
b) Right ventricular free wall collapse in early ventricular diastole may be absent in patients with marked right ventricular hypertrophy or elevated right ventricular diastolic pressures. Left ventricular collapse is a rare finding, because the muscular left ventricle produces a higher end-diastolic pressure.
2) Plethoric inferior vena cava (IVC): Dilated IVC (>20 mm) with <50% collapse on inspiration.
3) Respiratory variation:
a) Inflow velocity variation across the mitral (>30%) and tricuspid (>60%) valves.
b) Hepatic flow reversal on expiration during diastole.
4. Computed tomography (CT) (Figure 3.5-6) reveals pericardial effusion. In patients with chylopericardium it may help locate a connection between the thoracic duct and the pericardium (especially when combined with lymphography).
5. Analysis of pericardial fluid (see Pericardial Fluid Analysis) is used in case of equivocal etiology.
Cardiac tamponade is diagnosed based on clinical features (hypotension, tachycardia) and imaging studies, mainly echocardiography.
Clinical signs of cardiac tamponade should be differentiated from acute right ventricular myocardial infarction and other causes of right ventricular dysfunction.
TreatmentTop
1. IV fluid bolus may be attempted to temporize (this is not a substitute for definitive treatment). However, only ~50% of patients will have a favorable stroke volume/hemodynamic response to fluid loading.
2. Pericardiocentesis is a life-saving procedure in those with clinical/echocardiographic pericardial tamponade. Note that a large pericardial effusion does not always cause tamponade and therefore clinical and hemodynamic assessment is required. Needle pericardiocentesis with or without pericardial tube insertion using echocardiographic guidance is the preferred method of pericardial fluid drainage if technically feasible.
3. Surgical approaches can be considered if effusion is not amenable to percutaneous needle drainage as well as in the case of purulent effusions, recurrent effusions from malignancy requiring pericardial window creation, or hemopericardium with clotted blood.
4. Treatment of chylopericardium depends on the etiology and volume of lymph in the pericardium. In patients with chylopericardium that develops as a postoperative complication, use pericardiocentesis and a diet containing medium-chain triglycerides. If lymph continues to accumulate, use surgical treatment.
FiguresTop
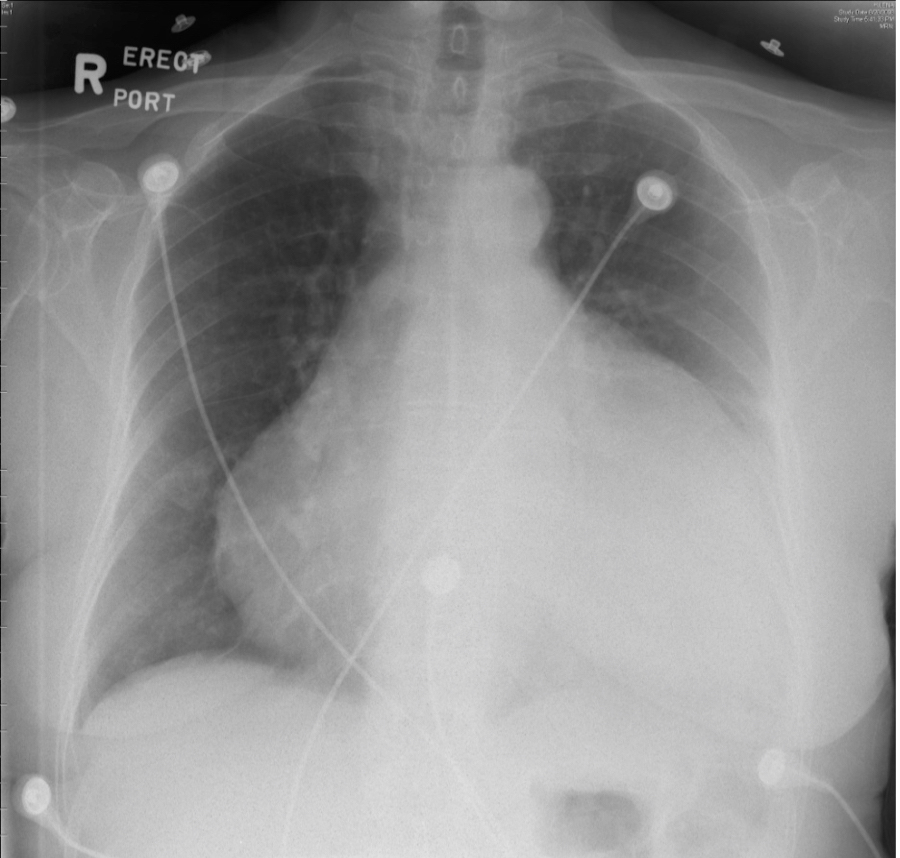
Figure 3.5-1. Chest radiography of a patient with cardiac tamponade before pericardiocentesis. Figure courtesy of Dr Craig Ainsworth.
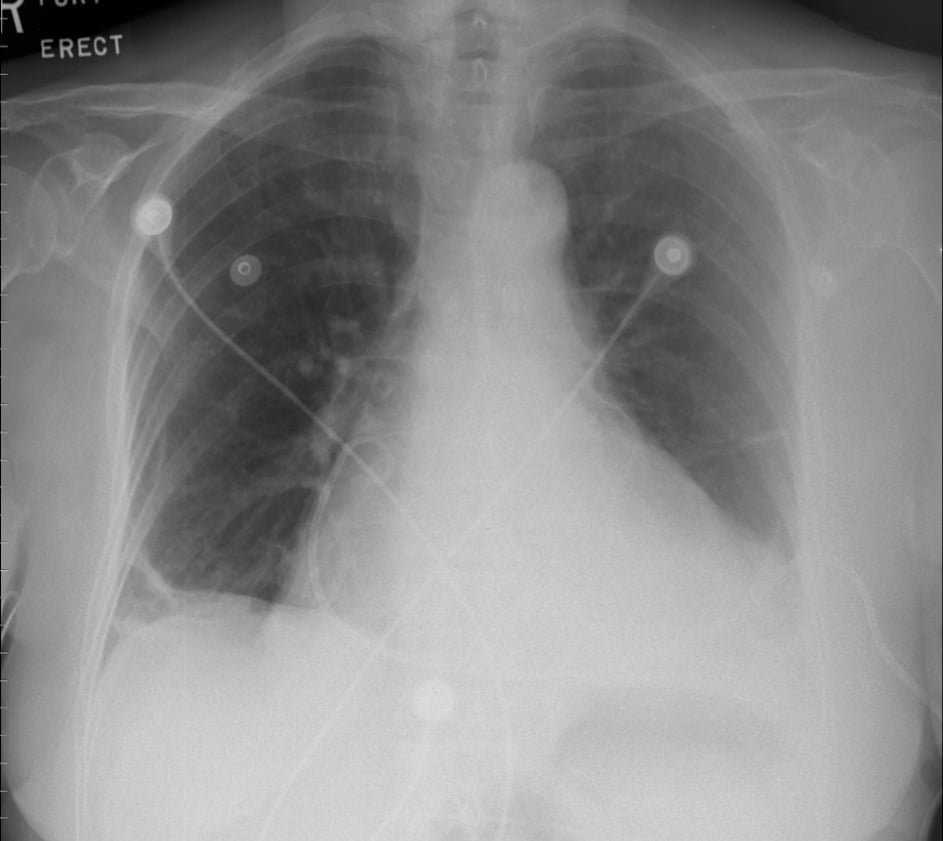
Figure 3.5-2. Chest radiography of a patient with cardiac tamponade after pericardiocentesis. Figure courtesy of Dr Craig Ainsworth.
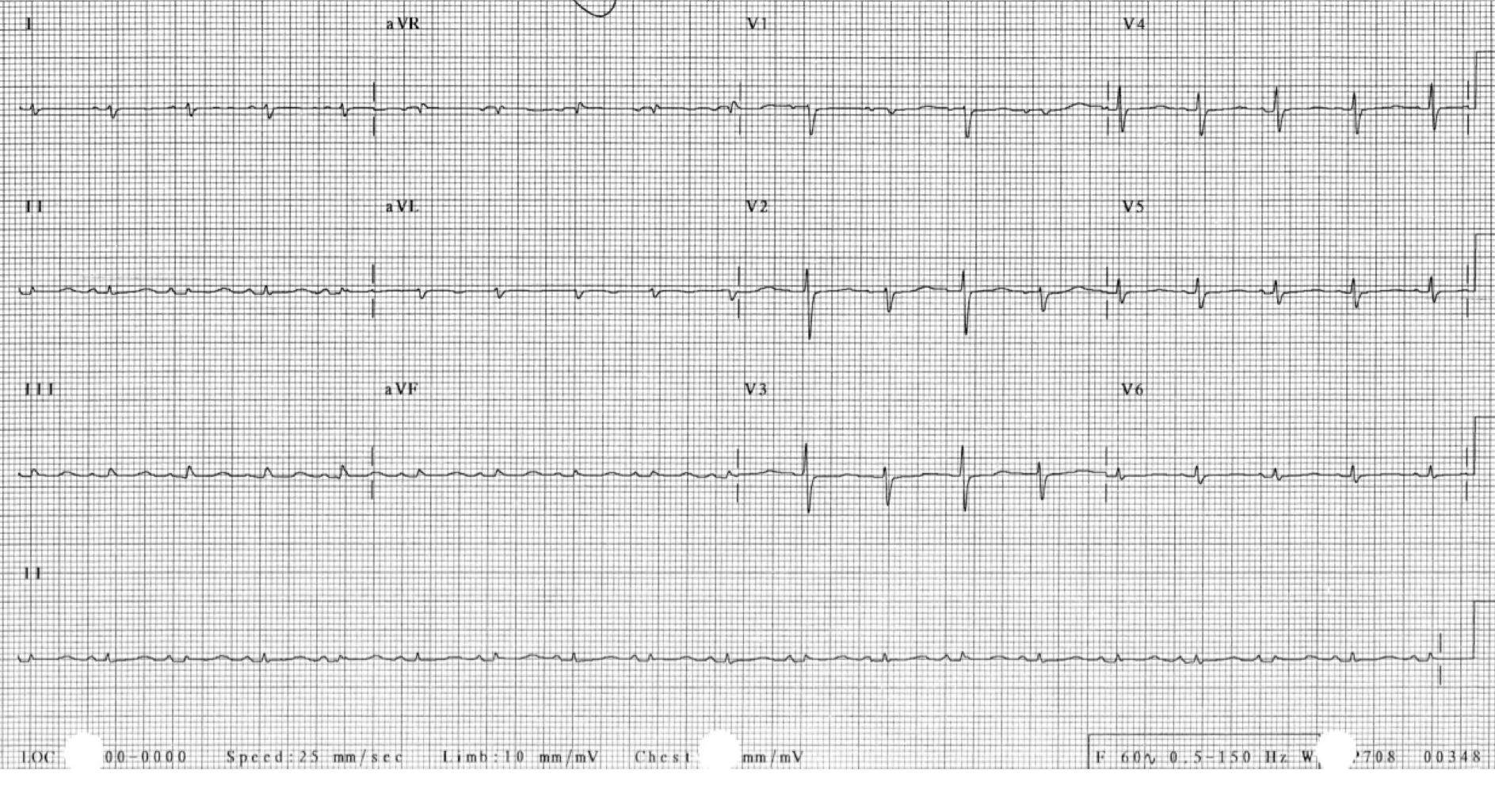
Figure 3.5-3. Electrical alternans of the QRS complex in a patient with cardiac tamponade. Figure courtesy of Dr Craig Ainsworth.
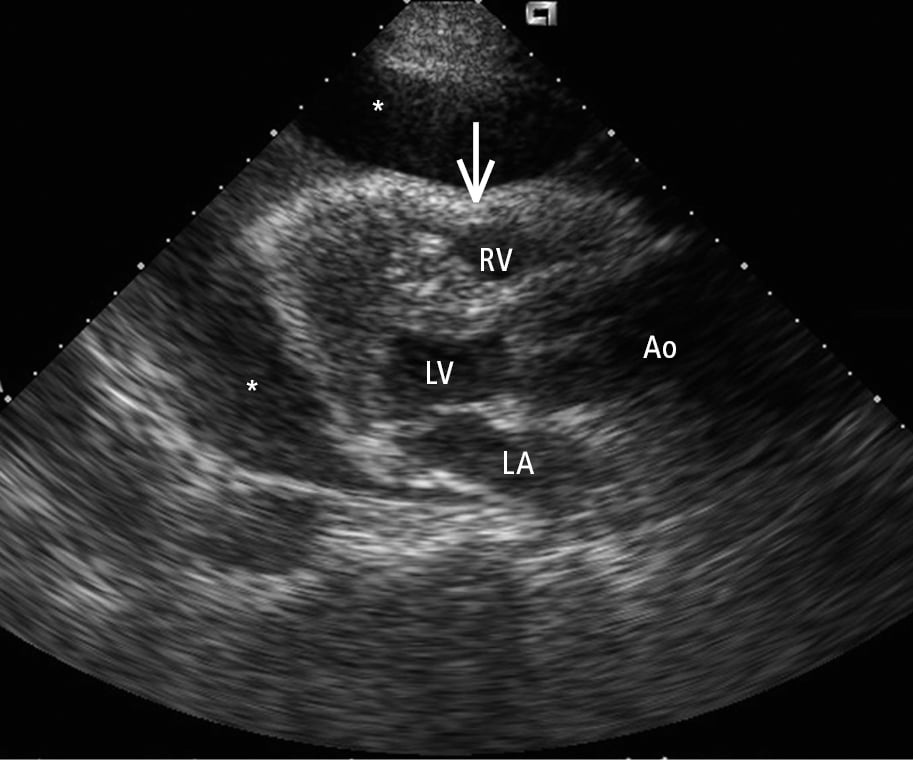
Figure 3.5-4. Transthoracic echocardiography (TTE), parasternal long-axis view: a large pericardial effusion (asterisks) and compression of the right-sided chambers of the heart (arrow). Ao, aorta; LA, left atrium; LV, left ventricle; RV, right ventricle.
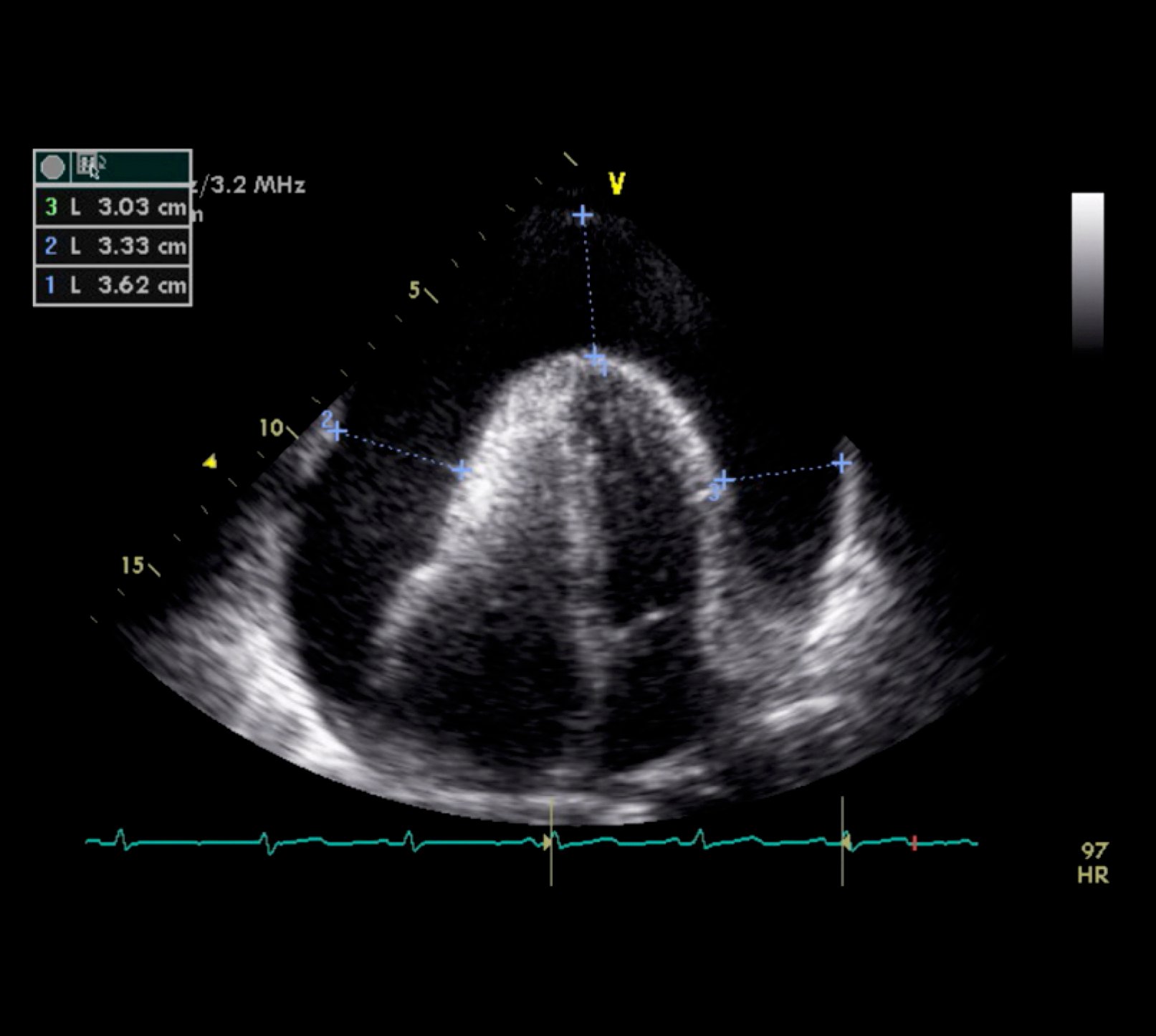
Figure 3.5-5. Transthoracic echocardiography (TTE) showing the apical 4-chamber view and a large pericardial effusion. Figure courtesy of Dr Craig Ainsworth.

Figure 3.5-6. Chest computed tomography (CT): a large pericardial effusion (asterisks).