Stevens SM, Woller SC, Kreuziger LB, et al. Antithrombotic Therapy for VTE Disease: Second Update of the CHEST Guideline and Expert Panel Report. Chest. 2021 Dec;160(6):e545-e608. doi: 10.1016/j.chest.2021.07.055. Epub 2021 Aug 2. Erratum in: Chest. 2022 Jul;162(1):269. doi: 10.1016/j.chest.2022.05.028. PMID: 34352278.
Definition, Etiology, PathogenesisTop
Superficial thrombophlebitis refers to inflammation of the veins located above the fascial layer that is usually accompanied by thrombosis of varying severity.
Thrombophlebitis of varicose veins accounts for ~90% of all cases of superficial thrombophlebitis, more frequently affecting the medial greater (long) saphenous vein, less often the lateral lesser (short) saphenous vein. The mechanism of thrombophlebitis includes stasis in the varicose veins and abnormalities of the venous wall, which lead to thrombosis and subsequent inflammation of the venous wall.
Idiopathic superficial thrombophlebitis usually affects the lesser saphenous vein or the greater saphenous vein but may develop in any superficial vein (Figure 3.19-1).
Recurrent superficial thrombophlebitis usually occurs in the same area of the affected leg. Migratory superficial thrombophlebitis may precede or coexist with thromboangiitis obliterans (Buerger disease [Figure 3.19-2]), Behçet disease (see Behçet Disease), or with adenocarcinomas (Trousseau sign), most frequently pancreatic cancer. The risk of concomitant deep vein thrombosis (DVT) is low (~5%).
Catheter-related superficial thrombophlebitis (excluding catheters inserted directly into the central vein) most frequently affects the superficial veins of the upper extremities, less frequently the superficial veins of the lower extremities. It is caused by the insertion and long-term use of peripheral venous catheters. Factors contributing to the development of thrombophlebitis include large-bore catheters, central venous catheters inserted via a peripheral vein (eg, antecubital vein), infection, hypercoagulability, hormone treatment, and irritants (eg, drugs or potassium chloride administered via the catheter).
Purulent superficial thrombophlebitis may develop in patients with bacteremia persisting for >72 hours despite appropriate antimicrobial therapy, particularly in patients with indwelling venous catheters. The most frequent etiologic factors include Staphylococcus aureus, streptococci, and gram-negative rods.
Clinical Features and Natural HistoryTop
Signs of superficial thrombophlebitis include painful localized edema and erythema of the skin. In the case of superficial thrombophlebitis of the varicose veins, they can be easily palpated as a nodular or cord-like thickening. In patients with catheter-related superficial thrombophlebitis, the signs are observed in the area of the affected vein. Drawing blood from the catheter is impossible if a thrombus is blocking its entry. In some patients (5%-13%) the condition may be asymptomatic. Patients with purulent superficial thrombophlebitis additionally develop fever, severe erythema, pain, and purulent exudate in the area of the affected vein.
Untreated superficial thrombophlebitis usually resolves spontaneously after several days or weeks, but it can progress to DVT or pulmonary embolism in 1% to 2% of patients. Patients with thrombophlebitis of the greater saphenous vein, especially if the thrombus is in close proximity to the adductor canal, are likely at higher risk of DVT. Within several months varicose veins usually undergo at least partial recanalization.
DiagnosisTop
Diagnosis is based on clinical manifestations. In the case of catheter-related superficial thrombophlebitis, cultures may reveal the etiologic agent (the specimen is usually the tip of the removed catheter). Diagnostic tests are not necessary in localized superficial thrombophlebitis, particularly when it is catheter related or caused by irritants. In patients with superficial thrombophlebitis of the varicose veins of the lower extremities, perform ultrasonography to localize the head of the thrombus and determine its distance from the deep venous system, because thrombophlebitis of the greater (long) saphenous vein that is in close proximity to the saphenofemoral junction may extend to the deep venous system. In patients with migratory thrombophlebitis without an apparent cause, perform a thorough diagnostic workup to exclude malignancy. In patients with thrombophlebitis of previously normal (nonvaricose) veins, consider underlying causes such as oral contraceptive use, vasculitis (eg, Behçet disease), or thrombophilia.
TreatmentTop
1. Catheter-related superficial thrombophlebitis: In patients with a short peripheral catheter, stop using the catheter and remove it. In cases of mild to moderate pain, use nonsteroidal anti-inflammatory drugs (NSAIDs) (oral or topical; agents: see Table 18.12-2) or heparin (topical gel) until the resolution of symptoms, but no longer than for 2 weeks.
The use of heparin at therapeutic doses for DVT (eg, enoxaparin 1 mg/kg bid) is not recommended. Low-dose antithrombotic treatment (eg, fondaparinux 2.5 mg once daily, enoxaparin 40 mg once daily, or rivaroxaban 10 mg once daily) could be considered if symptoms from superficial thrombophlebitis persist despite catheter removal. The duration of treatment should be ~4 weeks, but it can be decreased if symptoms resolve promptly and if the catheter is removed.
Assess the catheter site for signs of inflammation or abscess.
Superficial vein thrombosis is not an indication for routine removal of the peripherally inserted central venous catheter, particularly if it is functioning and required for medically necessary treatments (eg, administration of antibiotics).
2. Purulent superficial thrombophlebitis: Remove the source of infection (eg, a catheter) and use antimicrobial treatment, which should optimally be targeted; if ineffective, consider drainage or resection of the affected segment of the vein.
3. Superficial thrombophlebitis affecting a lower extremity vein segment ≥5 cm: Subcutaneous fondaparinux 2.5 mg/d, low-molecular-weight heparin at a prophylactic dose, or oral rivaroxaban 10 mg/d (see Table 3.20-9) for ≥4 weeks. In selected patients with severe extensive superficial thrombophlebitis, typically involving the entire length of the greater saphenous vein, consider therapeutic-dose anticoagulation as used in DVT treatment (eg, a vitamin K antagonist [acenocoumarol or warfarin] at a dose adjusted to maintain the international normalized ratio [INR] in the range of 2.0-3.0, in combination with heparin for 5 days, and continued as monotherapy for ≥4 weeks). Additional indications for anticoagulation treatment (in patients with thrombophlebitis affecting a segment <5 cm) include thrombophlebitis in the area of the saphenofemoral junction, severe clinical manifestations, history of venous thromboembolism or superficial vein thrombosis, active malignancy, and recent surgery. Once acute inflammation and edema have subsided, consider using appropriate compression stockings.
Localized superficial vein thrombosis (thrombus involving a short vein segment [<5 cm] located far from the saphenofemoral junction) probably requires no anticoagulation therapy. Use NSAIDs (oral or topical) to alleviate the symptoms.
FiguresTop
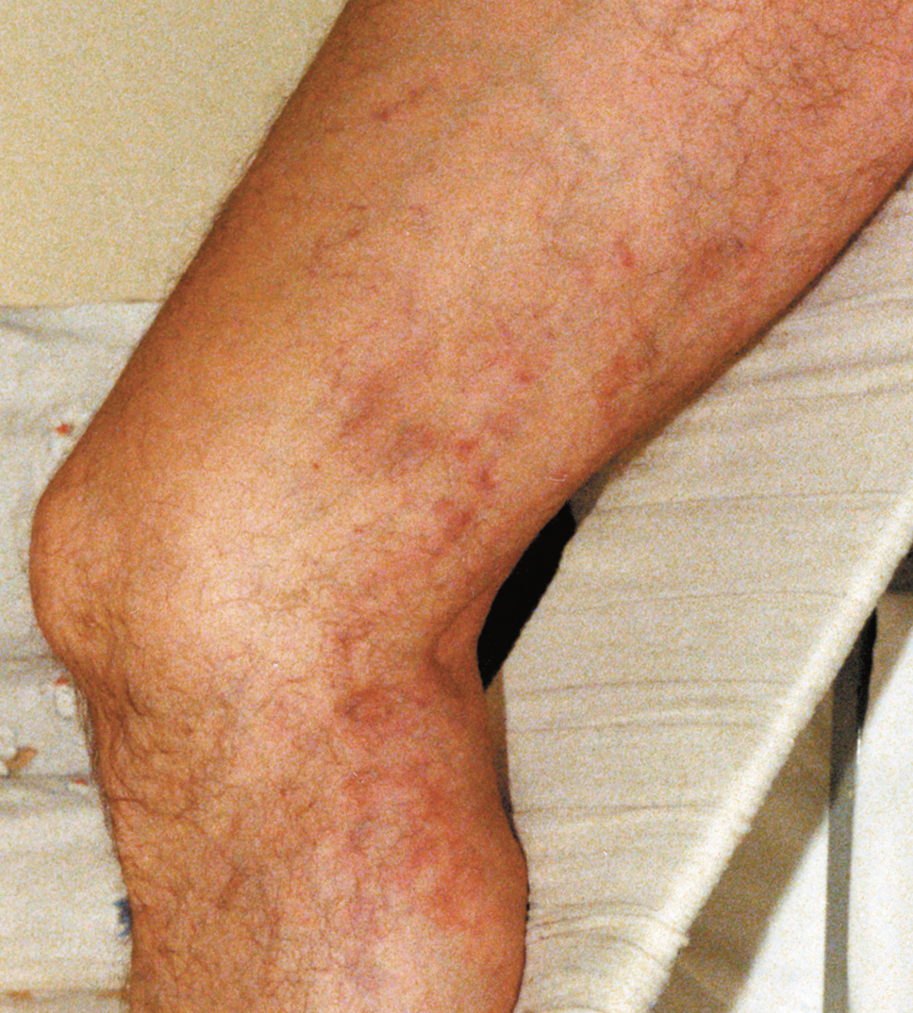
Figure 3.19-1. Varicose phlebitis of the great saphenous vein. Figure courtesy of Dr Leszek Masłowski.

Figure 3.19-2. Thromboangiitis obliterans. Superficial phlebitis coexisting with features of limb ischemia. Figure courtesy of Dr Leszek Masłowski.