Etiology, Pathogenesis, Clinical FeaturesTop
Monoclonal antibodies to epidermal growth factor receptor (EGFR) (eg, cetuximab, panitumumab) and tyrosine kinase inhibitors (TKIs) acting on the signaling pathways activated by the EGFR (eg, gefitinib, erlotinib, afatinib, osimertinib, and lapatinib) cause specific cutaneous toxicities in >80% of patients due to the abundant expression of the EGFR in the skin. The EGFR plays a critical role in the maintenance of skin homeostasis, as it is involved in regulating keratinocyte proliferation. EGFR inhibition leads to arrest of keratinocyte growth and subsequent apoptosis, resulting in skin toxicity.
Initial clinical manifestations include local erythema, edema, pruritus, and paresthesia (burning sensation), most commonly of the upper torso, neck, and face. Later, an acneiform rash characterized by sterile pustules and papules appears on the same erythematous areas (see Figure 13.1-1). The clinical presentation is similar to that of acne, but the lesions vary in size and lack the white and black comedones, which represent the hallmark of acne. Lesions can also be pruritic. Initial pustules are sterile, but superinfection with Staphylococcus aureus can occur. With prolonged exposure to EGFR inhibitors, the patient may develop severe xerosis, telangiectasia, and paronychia around the nails. In severe cases, the cutaneous lesions become more severe, with continuous exfoliation and desquamation. Other late manifestations may include hair loss, alopecia of the scalp, excessive facial hair growth (including excessive eyelash growth), and paronychia.
The cutaneous manifestations are generally mild to moderate. Severe cases can be seen in 8% to 17% of patients, warranting temporary or permanent discontinuation of the offending drug unless a severe, acneiform eruption is not a contraindication to continue anti-EGFR therapy.
TreatmentTop
1. Treatment of the skin manifestations depends on their severity (Table 13.1-1). Consider consultation with a dermatologist or oncologist.
2. Excessive growth of eyebrows, eyelashes, or other facial hair may be treated by different methods of epilation (eg, laser).
3. Patients who develop skin reactions to EGFR inhibitors generally have a better response to treatment and a higher survival rate than others.
Tables AND FIGURESTop
|
Type |
Clinical manifestations |
Treatment |
|
Papulopustular (acneiform) rash |
Grade 1: Papulopustular eruption <10% of BSA |
Topical treatment: Low-potency topical glucocorticoids (eg, 2.5% hydrocortisone cream bid ± topical 1% clindamycin gel or solution), moisturizer |
|
Grade 2: Papulopustular eruption 10%-30% of BSA; limiting iADLs |
Topical treatment: 2.5% hydrocortisone cream bid, moisturizer Systemic treatment: Oral antibiotics with good anti-inflammatory properties, such as doxycycline or minocycline 100 mg PO bid for 7-14 days to assess response and treat for ≥4 weeks Antipruritic treatment: Oral antihistamines (eg, hydroxyzine, cetirizine) Analgesic treatment: Acetaminophen, ibuprofen | |
|
Grade 3: – Papulopustular eruption >30% of BSA – Limiting ADLs |
Dose modification or discontinuation of EGFR inhibitors until severity of skin rash decreases ≤grade 2 Topical treatment: 2.5% hydrocortisone cream bid, moisturizer Systemic treatment: Doxycycline or minocycline 100 mg PO bid for 7-14 days to assess response and treat for ≥4 weeks + prednisone 0.5 mg/kg for 7 days Antipruritic and analgesic treatment: As above | |
|
Grade 4: – Involvement of >30% BSA with serious consequences – Erythroderma (skin desquamation and ulcerations) |
– Discontinuation of EGFR inhibitors and transfer to specialized burn treatment facility – Consider dermatology consultation for treatment with low doses of oral retinoids (eg, isotretinoin or acitretin) | |
|
Dry skin (xerosis) |
Pruritus and dry skin |
General recommendations: Avoid excessive skin exposure to water and soap Emollients: 5%-10% urea and other preparations Antipruritic treatment: Oral antihistamines (eg, hydroxyzine, cetirizine) |
|
Fissures |
Emollients: 5%-10% urea and other preparations | |
|
Inflammation of fingertips |
Emollients: 5%-10% urea, intermittent topical treatment with medium-potency glucocorticoid (eg, fluticasone, betamethasone) | |
|
Paronychia |
General recommendations: Preventive measures (loose footwear, antiseptic baths) Topical treatment: Topical high-potency glucocorticoids (eg, clobetasol propionate for 2 weeks) ± topical antifungal agent (eg, ketoconazole cream bid for 2 weeks) Treatment of infection: Cephalexin (500 mg PO qid) or cloxacillin 500 mg PO qid for 7 days | |
|
bid, 2 times a day; BSA, body surface area; ADL activities of daily living; EGFR, epidermal growth factor receptor; iADL, instrumental activities of daily living; PO, orally; qid, 4 times a day. | ||
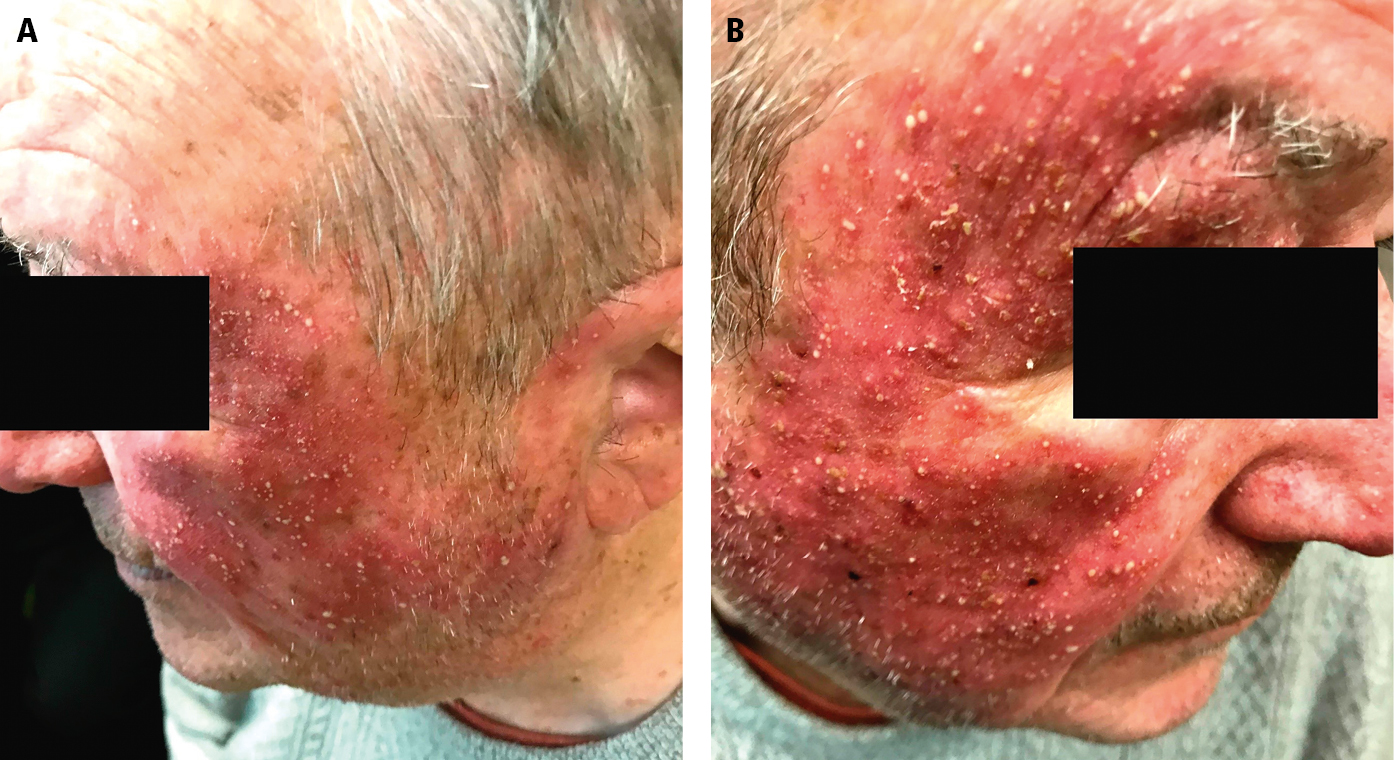
Figure 13.1-1. Diffuse acneiform papules and pustules on the face due to erlotinib treatment in a patient with non–small cell lung cancer.