Cho SH, Kim DW, Gevaert P. Chronic Rhinosinusitis without Nasal Polyps. J Allergy Clin Immunol Pract. 2016 Jul-Aug;4(4):575-82. doi: 10.1016/j.jaip.2016.04.015. Review. PubMed PMID: 27393771; PubMed Central PMCID: PMC4939221.
Peters AT, Spector S, Hsu J, et al; Joint Task Force on Practice Parameters, representing the American Academy of Allergy, Asthma and Immunology, the American College of Allergy, Asthma and Immunology, and the Joint Council of Allergy, Asthma and Immunology. Diagnosis and management of rhinosinusitis: a practice parameter update. Ann Allergy Asthma Immunol. 2014 Oct;113(4):347-85. doi: 10.1016/j.anai.2014.07.025. PubMed PMID: 25256029.
Kaplan A. Canadian guidelines for acute bacterial rhinosinusitis: clinical summary. Can Fam Physician. 2014 Mar;60(3):227-34. Review. PubMed PMID: 24627376; PubMed Central PMCID: PMC3952756.
Kaplan A. Canadian guidelines for chronic rhinosinusitis: Clinical summary. Can Fam Physician. 2013 Dec;59(12):1275-81, e528-34. PubMed PMID: 24336538; PubMed Central PMCID: PMC3860922.
Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012 Mar;50(1):1-12. doi: 10.4193/Rhino50E2. PubMed PMID: 22469599.
Desrosiers M, Evans GA, Keith PK, et al. Canadian clinical practice guidelines for acute and chronic rhinosinusitis. Allergy Asthma Clin Immunol. 2011 Feb 10;7(1):2. doi: 10.1186/1710-1492-7-2. PubMed PMID: 21310056; PubMed Central PMCID: PMC3055847.
Brozek JL, Bousquet J, Baena-Cagnani CE, et al; Global Allergy and Asthma European Network; Grading of Recommendations Assessment, Development and Evaluation Working Group. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010 Sep;126(3):466-76. doi: 10.1016/j.jaci.2010.06.047. PubMed PMID: 20816182.
Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD006394. Review. Update in: Cochrane Database Syst Rev. 2016;4:CD006394. PubMed PMID: 17636843.
Definition, Etiology, PathogenesisTop
Rhinosinusitis refers to inflammation of the mucosa, nasal cavities, and sinuses (previously termed sinusitis). It is classified as:
1) Acute rhinosinusitis (<4 weeks’ duration, complete resolution of symptoms) or recurrent acute rhinosinusitis (≥4 episodes per year).
2) Chronic rhinosinusitis (CRS) (>12 weeks’ duration; as defined by Canadian guidelines, >8 weeks’ duration) with nasal polyps (CRSwNP) or without nasal polyps (CRSsNP).
3) Subacute rhinosinusitis (4-12 weeks’ duration).
The etiology of acute rhinosinusitis is usually infectious (viral: common cold, usually lasting <5 days; nonviral: worsening of symptoms after 5 days of illness or symptoms lasting ≥10 days). The complex interaction between inflammatory cells, obstruction of the sinus ostia, impairment of mucociliary clearance, and involvement of the adjacent bones all play a role in the development of acute and even more so chronic rhinosinusitis. Causes of obstruction of the sinus ostia include allergic and nonallergic rhinitis, infections, anatomic defects of the nasal cavity (eg, nasal septal deviation), and other factors. Etiologic factors causing acute rhinosinusitis include rhinoviruses (up to 50%), other viruses, Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and (rarely) other bacteria or fungi. In chronic rhinosinusitis, allergic hyperresponsiveness directed against colonizing bacteria (especially Staphylococcus aureus) or fungi, or chronic infection may play a role.
Clinical Features and Natural HistoryTop
1. Symptoms: Nasal purulent discharge, postnasal discharge, nasal obstruction (congestion), hyposmia or anosmia, headache, halitosis (unpleasant breath odor), dental pain, cough (caused by postnasal drip), or facial pressure localized to the affected sinus.
2. Physical findings: Fever (may be low grade), mucosal reddening and edema, nasal discharge, postnasal drip, tenderness of the areas of affected sinuses.
3. Natural history: Acute viral rhinosinusitis usually resolves spontaneously (improvement as early as after 48 hours). Superimposed bacterial infection should be suspected in case of worsening of symptoms at 5 days or no improvement after 7 to 10 days. The course of chronic rhinosinusitis may include periods of remission and recurrence.
DiagnosisTop
Diagnosis according to the 2011 Canadian clinical practice guidelines:
1) Acute bacterial rhinosinusitis (ABRS): Diagnosis requires:
a) ≥2 symptoms of PODS (facial pain/pressure/fullness; nasal obstruction; nasal purulence/discolored postnasal discharge; hyposmia/anosmia [smell]), one of which must be O or D; and
b) Symptom duration >7 days without improvement.
2) CRS: Diagnosis requires:
a) ≥2 symptoms of CPODS (facial congestion/fullness; facial pain/pressure; nasal obstruction/blockage; purulent anterior/posterior nasal drainage; hyposmia/anosmia [smell]); and
b) ≥1 objective finding on endoscopy or computed tomography (CT).
CRS may be overdiagnosed (incorrectly diagnosed when not present) due to the overlap of symptoms with other disease entities.
Following the above criteria, there is a need for an objective finding to confirm diagnosis. Of note, a large proportion of patients diagnosed in the past as having rhinosinusitis do not fulfill these criteria when evaluated by a nonotolaryngologist.Evidence 1Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to indirectness. Novis SJ, Akkina SR, Lynn S, Kern HE, Keshavarzi NR, Pynnonen MA.A diagnostic dilemma: chronic sinusitis diagnosed by non-otolaryngologists. Int Forum Allergy Rhinol. 2016 May;6(5):486-90. doi: 10.1002/alr.21691. Epub 2016 Jan 11. PubMed PMID: 26750399; PubMed Central PMCID: PMC4856571.
1. Laboratory tests: Elevated erythrocyte sedimentation rate (ESR) and white blood cell counts in bacterial rhinosinusitis. Elevated serum IgE in allergic CRS.
2. Imaging studies: Indicated in CRS and in the case of suspected complications. CT of the sinuses (possibly radiography) reveals sinus opacifications, fluid levels, mucosal thickening or polyps, anatomic defects predisposing to rhinosinusitis, and complications of the disease. This test is not recommended in the case of uncomplicated ABRS, as patients with a viral upper respiratory tract infection will likely have sinus opacification. Magnetic resonance imaging (MRI) is used in the diagnostic workup of fungal rhinosinusitis or malignancy.
3. Microbiology: Routine nasal culture is not recommended for the diagnosis of ABRS. When required because of an unexpected clinical course (resistance to treatment), sinus aspirates can be obtained, usually by endoscopically guided culture or, rarely, by maxillary tap.
4. Other studies used in the diagnostics of causes and complications of rhinosinusitis include anterior rhinoscopy, endoscopy of the nasal cavity and sinuses, as well as diagnostic tests for allergies, immune deficiencies, and cystic fibrosis.
This includes differential diagnosis of rhinitis, headache, and chronic cough.
TreatmentTop
1. ABRS: Management algorithm: Figure 17.20-1.
1) Nasal lavage using isotonic or hypertonic saline.
2) Nonsteroidal anti-inflammatory drugs in case of pain.
3) Nasal decongestants (see Allergic Rhinitis): There is limited evidence supporting the use of nasal decongestants. They should be used only for a short course (<5 days) to avoid rhinitis medicamentosa.
4) Antibiotics should not be used in patients with acute uncomplicated rhinosinusitis. Indications: Figure 17.20-1. The literature suggests antibiotic treatment of ABRS may shorten the time to symptom resolution, although most studies show similar disease progression with ultimately similar rates of resolution in patients receiving antibiotics or placebo. However, there are no high-quality data on individuals with severe sinusitis or immunocompromised status. First-line therapy is amoxicillin 1.5 to 2 g every 12 hours. Second-line therapy includes amoxicillin/clavulanic acid (amoxicillin 1.5-2 g every 12 hours) and cephalosporins (eg, cefuroxime 0.5 g every 12 hours); in case of allergic reactions to beta-lactam antibiotics, administer macrolides (eg, clarithromycin 0.5 g every 12 hours or azithromycin 0.25-0.5 g every 24 hours for 3 days or a single dose of 2 g).
5) Intranasal corticosteroids (INCSs): Indications: Figure 17.20-1. There is significant evidence to suggest that INCSs improve symptoms and the time to symptom resolution. They are recommended as monotherapy for mild to moderate ABRS and are useful for preventing future episodes in patients with recurrent ABRS.
6) Antihistamines: Useful only in patients with allergies.
2. CRS: Management algorithm: Figure 17.20-2.
1) INCSs are the mainstay of CRS treatmentEvidence 2Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to indirectness and the risk of bias. Chong LY, Head K, Hopkins C, Philpott C, Schilder AG, Burton MJ. Intranasal steroids versus placebo or no intervention for chronic rhinosinusitis. Cochrane Database Syst Rev. 2016 Apr 26;4:CD011996. doi: 10.1002/14651858.CD011996.pub2. Review. PubMed PMID: 27115217. with significant evidence for benefit in CRSwNP (decrease in polyp size and prevention of regrowth); studies involving patients with CRSsNP are more limited. The 2012 European Position Paper on Rhinosinusitis and Nasal Polyps concluded INCSs are effective and not associated with major adverse effects. Agents and dosage: see Allergic Rhinitis.
2) Oral corticosteroids: A short course is effective in reducing polyp size in patients with refractory CRS. There is limited evidence for corticosteroid use in patients with CRSsNP, although such therapy may be beneficial in those with severe symptoms.
3) Antibiotics may be beneficial in the setting of bacterial CRSsNP, but there is very limited evidence for short-course antibiotics compared with placebo. Long-term low-dose macrolide therapy has some evidence of benefit in patients with normal serum IgE and CRSsNP.Evidence 3Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to imprecision. Head K, Chong LY, Piromchai P, et al. Systemic and topical antibiotics for chronic rhinosinusitis. Cochrane Database Syst Rev. 2016 Apr 26;4:CD011994. doi: 10.1002/14651858.CD011994.pub2. Review. PubMed PMID: 27113482. The benefits are currently thought to be due to the anti-inflammatory rather than anti-infective properties of macrolides.
4) Topical or oral antihistamines: Used only in patients with allergies.
5) The benefits of nasal lavage are not entirely clearEvidence 4Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to the risk of bias, imprecision, and heterogeneity. Chong LY, Head K, Hopkins C, et al. Saline irrigation for chronic rhinosinusitis. Cochrane Database Syst Rev. 2016 Apr 26;4:CD011995. doi: 10.1002/14651858.CD011995.pub2. Review. PubMed PMID: 27115216. with suggestions of little benefit of low-volume (5 mL) nebulized saline spray compared with INCSs and some benefit of daily large-volume (150 mL) saline irrigations with a hypertonic solution compared with placebo.
Ear, nose, and throat (ENT) specialist consultation is indicated when diagnostic doubts are present or treatment is not effective. In selected patients polypectomy or endoscopic sinus surgery (ESS) is used.
ComplicationsTop
The complications of bacterial rhinosinusitis include orbital cellulitis, orbital abscess, osteomyelitis of the sinus walls, cavernous sinus thrombosis, meningitis, and brain abscess.
FiguresTop
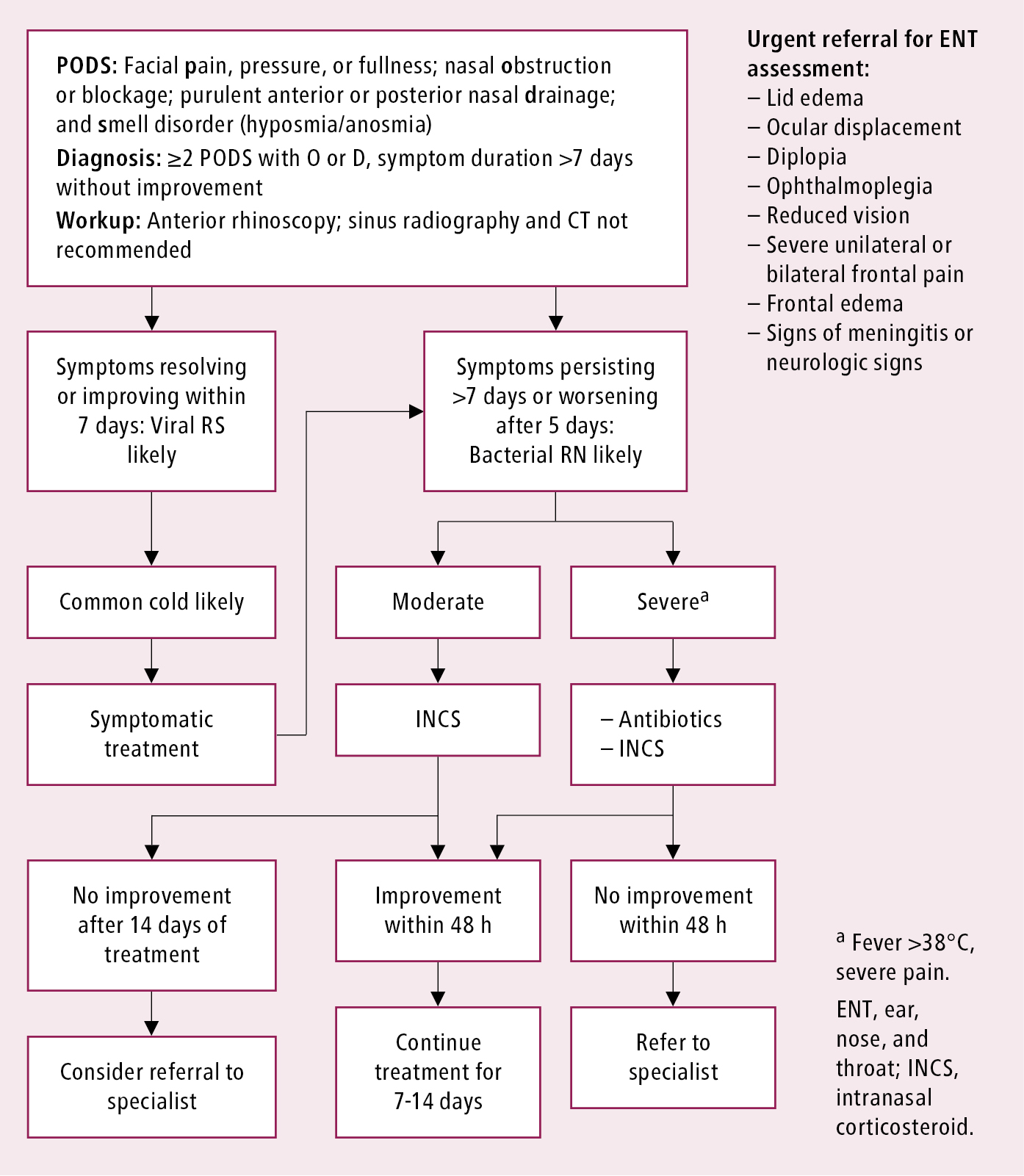
Figure 17.20-1. Management algorithm of adults with acute rhinosinusitis. Adapted from Rhinology. 2012 Mar;50(1):1-12.
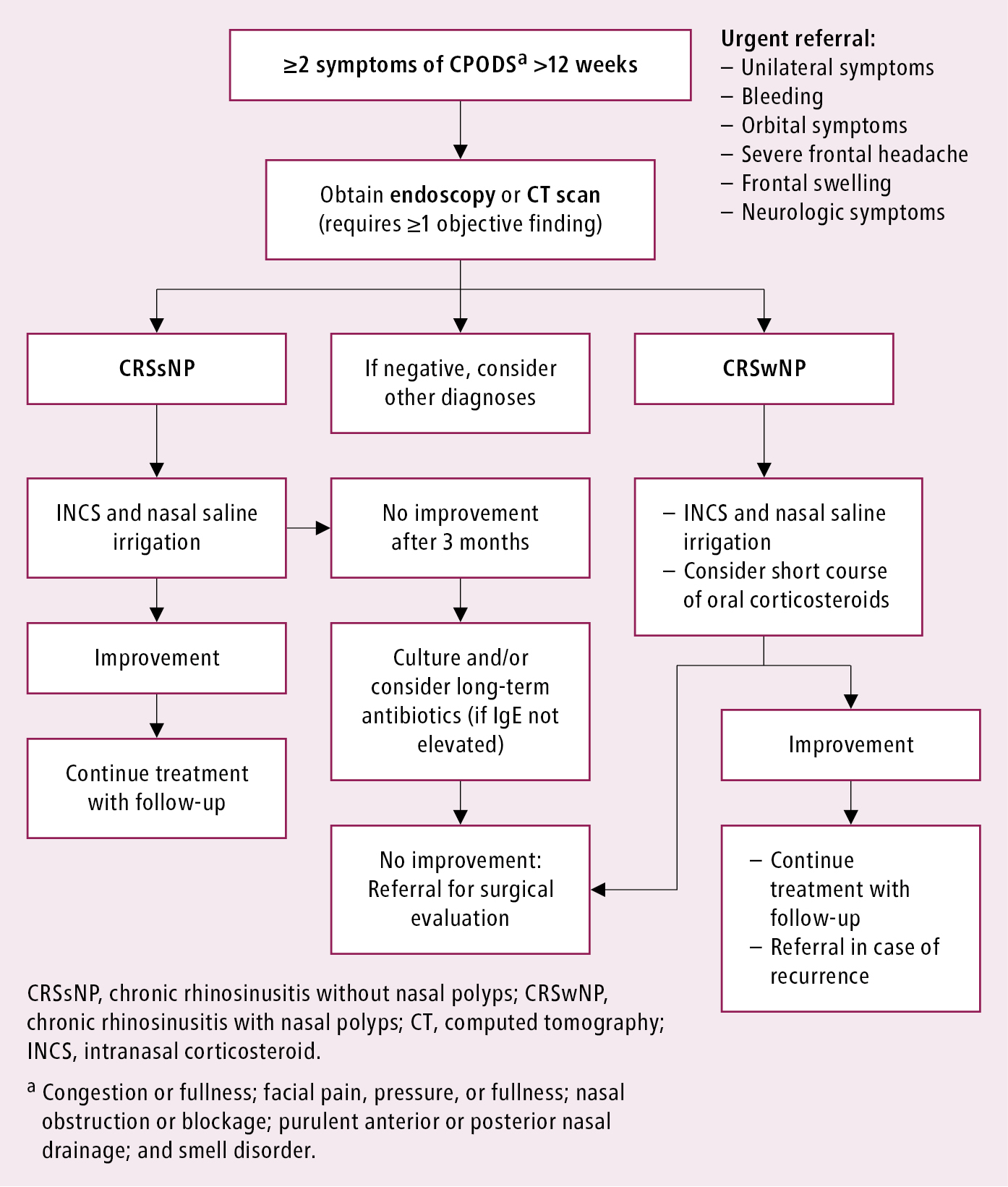
Figure 17.20-2. Management algorithm of adults with chronic rhinosinusitis. Adapted from Can Fam Physician. 2013;59(12):1275-81 and Rhinology. 2012;50(1):1-12.