Definition, Etiology, PathogenesisTop
1. Definition: The epiglottis is part of the structures comprising the superior portion of the larynx, which are collectively referred to as the supraglottis (Figure 17.9-1). Epiglottitis describes inflammation of the mucosa of the epiglottis (Figure 17.9-2). It is frequently associated with inflammation of other parts of the supraglottis, in which case the condition is referred to as supraglottitis.
2. Etiology: Epiglottitis may be either infectious or noninfectious. Infectious epiglottitis has historically been related to Haemophilus influenzae type b (Hib) infection. However, since the introduction of Hib vaccination, Hib infection is rare in vaccinated populations. Data on relevant pathogens in the vaccine era are incomplete; non–type b Haemophilus influenzae and Streptococcus species appear to be the most prevalent pathogens, although a wide variety of bacteria have been implicated. Staphylococcus aureus can rarely be a causative organism.
Noninfectious epiglottitis can be caused by a number of factors, among which trauma is the most common. Thermal trauma of the epiglottis is especially common in patients using makeshift filters to smoke crack cocaine but may occur with any type of inhalation burn. Blunt trauma to the neck may cause swelling of the supraglottic structures. Iatrogenic trauma, typically from a traumatic intubation, also causes injury to supraglottic structures. Finally, external beam radiation treatments for cancers of the upper aerodigestive tract often cause long-standing inflammation of the supraglottis.
Angioedema is another potential noninfectious cause of epiglottitis. Angioedema of the epiglottitis may be caused by a hypersensitivity reaction, various protein deficiencies (sometimes lumped together under the term hereditary angioedema), or medications, such as angiotensin-converting enzyme inhibitors.
3. Pathogenesis: Swelling of the upper airway causes airway obstruction in two ways. First, it reduces the airway lumen. Second, it is often associated with thickened secretions and impaired clearance of secretions. Epiglottitis may lead to deep neck space infections or abscesses. These infections can spread through the neck to cause septic thrombophlebitis of the internal jugular vein and inferiorly to cause mediastinitis.
Clinical FeaturesTop
The clinical presentation of epiglottitis depends on etiology. Infectious epiglottitis may present with a viral prodrome, fever, odynophagia, muffled voice, and drooling.
The key clinical feature of epiglottitis is respiratory distress, and its degree can vary significantly. Determining the severity of distress is the most important part of the clinical assessment.
Patients in severe distress are unable to lie flat, often sitting up and leaning forward (“tripoding”). They have markedly increased work of breathing with recruitment of accessory muscles of respiration and nasal flaring. Stridor is usually inspiratory and varies with the degree of obstruction and respiratory effort. Patients have difficulty managing their secretions and may be drooling.
Critically, patients may have normal oxygen saturations, and only as they tire will their oxygen saturations begin to decrease. This reduction in oxygen saturation presages imminent respiratory arrest. Consequently, using oxygen saturations as a marker of severity in epiglottitis may lead to disaster.
Patients with less severe obstruction and respiratory distress have little or no increased work of breathing. They are able to speak in complete sentences and easily tolerate lying on their back. They should have no difficulty handling their secretions.
DiagnosisTop
The diagnosis of epiglottitis is primarily made on the basis of the initial history and physical examination. Assessing the patient’s level of respiratory distress and stabilizing the airway take precedence over performing any diagnostic tests. Furthermore, before the patient is transferred from the safety of an emergency room setting to the radiology department, it is critical that their condition is stable for the transfer. Radiology departments are often poorly equipped to handle respiratory arrests.
1. Fiberoptic nasolaryngoscopy: Fiberoptic endoscopy of the upper airway is usually performed by the otolaryngology consultant service. It allows excellent visualization of the supraglottic structures and is key to diagnosing epiglottitis. It can be performed in the emergency room in awake patients in almost all situations. Special consideration is likely necessary in the very rare pediatric patient presenting with epiglottitis, in whom the theoretical risk of inducing laryngospasm requires that any endoscopic assessment of the airway should be performed in the operating room.
2. Lateral neck radiography: A lateral neck radiograph may show thickening of the epiglottis (the “thumb” sign). However, this finding is not pathognomonic of epiglottitis. The gold-standard investigation remains fiberoptic visualization. Suspicious clinical findings require further investigation with fiberoptic endoscopy regardless of the results of lateral neck radiography. Lingual tonsillitis may give the false impression of a positive thumb sign by obliterating the vallecular space.
3. Complete blood count, electrolytes.
4. Chest radiographs: Chest radiographs are performed to exclude concomitant intrathoracic problems.
5. Computed tomography (CT) scan of the neck and upper mediastinum: A contrast-enhanced CT scan of the neck can be useful to exclude the possibility of a deep neck abscess, especially in patients whose infection fails to respond to standard intravenous antibiotics or who have significant restriction of neck movement. It should only be ordered in patients stable enough to be transferred to the radiology department.
1. Croup: A consideration only in children. Epiglottitis is extremely rare in children, especially in infants and toddlers, the demographic most affected by croup. Croup typically presents with a viral prodrome, has a gradual onset, and is associated with barking cough. Conversely, when it does occur in children, epiglottitis has a rapid onset and causes significant airway distress.
2. Airway foreign body: A consideration mostly in children. Any history of aspiration should be taken seriously. Usually the diagnosis requires laryngoscopy or bronchoscopy in the operating room.
3. Lingual/palatine tonsillitis: Patients with tonsillitis may present with a muffled voice and noisy, snoring-like breathing. Infection of the palatine tonsils is visible on intraoral examination.
4. Laryngeal cancer: Laryngeal cancer may present as an obstructing lesion. It should be considered part of diagnosis in individuals with a smoking history. Occasionally, these patients may be misdiagnosed as having an exacerbation of obstructive pulmonary disease. Diagnosis requires fiberoptic endoscopy.
5. Subglottic stenosis: This usually presents with a gradual onset of worsening stridor and shortness of breath. It is often but not always associated with a history of prolonged intubation.
6. Paradoxical vocal fold movement: An idiopathic disorder. It requires fiberoptic endoscopy for diagnosis. Speech language therapy is the most common form of treatment.
7. Laryngomalacia: The most common cause of stridor in infants. This is almost always non–life-threatening. Diagnosis requires fiberoptic endoscopy.
TreatmentTop
Management of epiglottitis revolves around management of the airway. Patients with severe respiratory distress require immediate transfer to the operating room for an awake intubation or awake tracheostomy. Both anesthesia and otolaryngology services should be consulted. A team approach should be used to decide whether intubation or tracheostomy will be chosen as the primary management strategy. The team should also have at least one back-up plan in case the first strategy fails.
If specialty services do not exist and the patient is in extremis and unsafe to transfer to another institution, local airway expertise should be sought urgently and the airway should be controlled in whatever manner is deemed the safest and most expeditious.
While management of a severely distressed patient can be very difficult, the need for aggressive intervention is usually obvious. Sometimes equally challenging is deciding how to manage patients in less extreme distress; often they can be monitored in a step-down unit or intensive care unit and managed conservatively. The decision to use conservative management is based on both the history of how fast any airway distress is progressing and on the current status of the patient.
1. Antibiotics: Third-generation cephalosporins are the usual choice for treatment of infectious epiglottitis. Both cefotaxime and ceftriaxone are commonly used, as they have a broad spectrum of action. Knowledge of local flora is helpful in guiding antibiotic management. Some authors advocate the addition of vancomycin to the standard antibiotic regime as empiric treatment for methicillin-resistant Staphylococcus aureus.
2. Glucocorticoids: Only very limited evidence is available.Evidence 1Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to only case series describing use of steroids in this setting. Glynn F, Fenton JE. Diagnosis and management of supraglottitis (epiglottitis). Curr Infect Dis Rep. 2008 May;10(3):200-4. PubMed PMID: 18510881. The use of glucocorticoids is controversial, yet it is common in the initial period, especially if a conservative approach is being taken towards the airway. The goal of glucocorticoid use is to reduce airway swelling but it is not without risk, as it may worsen glucose control in patients with diabetes mellitus and reduce immune competency. The decision to use glucocorticoids should be taken carefully. Dexamethasone is commonly chosen because of its high glucocorticoid potency. The dose varies greatly and depends on the patient’s premorbid conditions; an average first dose of 4 to 8 mg and a daily dose of 8 to 16 mg may be reasonable. Typically, the use of glucocorticoids is reassessed daily based on the patient’s symptoms and findings on fiberoptic examination.
3. Racemic epinephrine: The use of inhaled racemic epinephrine may allow temporary stabilization of airway distress to facilitate transfer to the operating room for definitive airway management. Racemic epinephrine is usually given as a nebulized solution (commonly a 2.25% solution with the usual dose of 0.5 mL).
4. Heliox: Heliox is a mixture of helium and oxygen, which allows for less turbulent inhalations in patients with epiglottitis. Like racemic epinephrine, heliox should only be used to temporarily stabilize a patient prior to definitive airway control.
1. Intubated patients require care in an intensive care unit. Tracheotomized patients require care in a step-down unit or specialized head and neck surgery unit.
2. Patients who are not intubated require close observation in a specialized unit with a tracheostomy tray at the bedside.
3. Intravenous rehydration and venous thromboembolism prophylaxis are used as necessary.
ComplicationsTop
Epiglottitis may lead to abscess formation within the structures of the larynx or in the adjacent deep neck spaces. Retropharyngeal abscess can cause descending mediastinitis.
PrognosisTop
Prognosis is excellent. Early recognition and prompt treatment of airway distress in the vaccine era has led to a mortality rate <1%.
FiguresTop
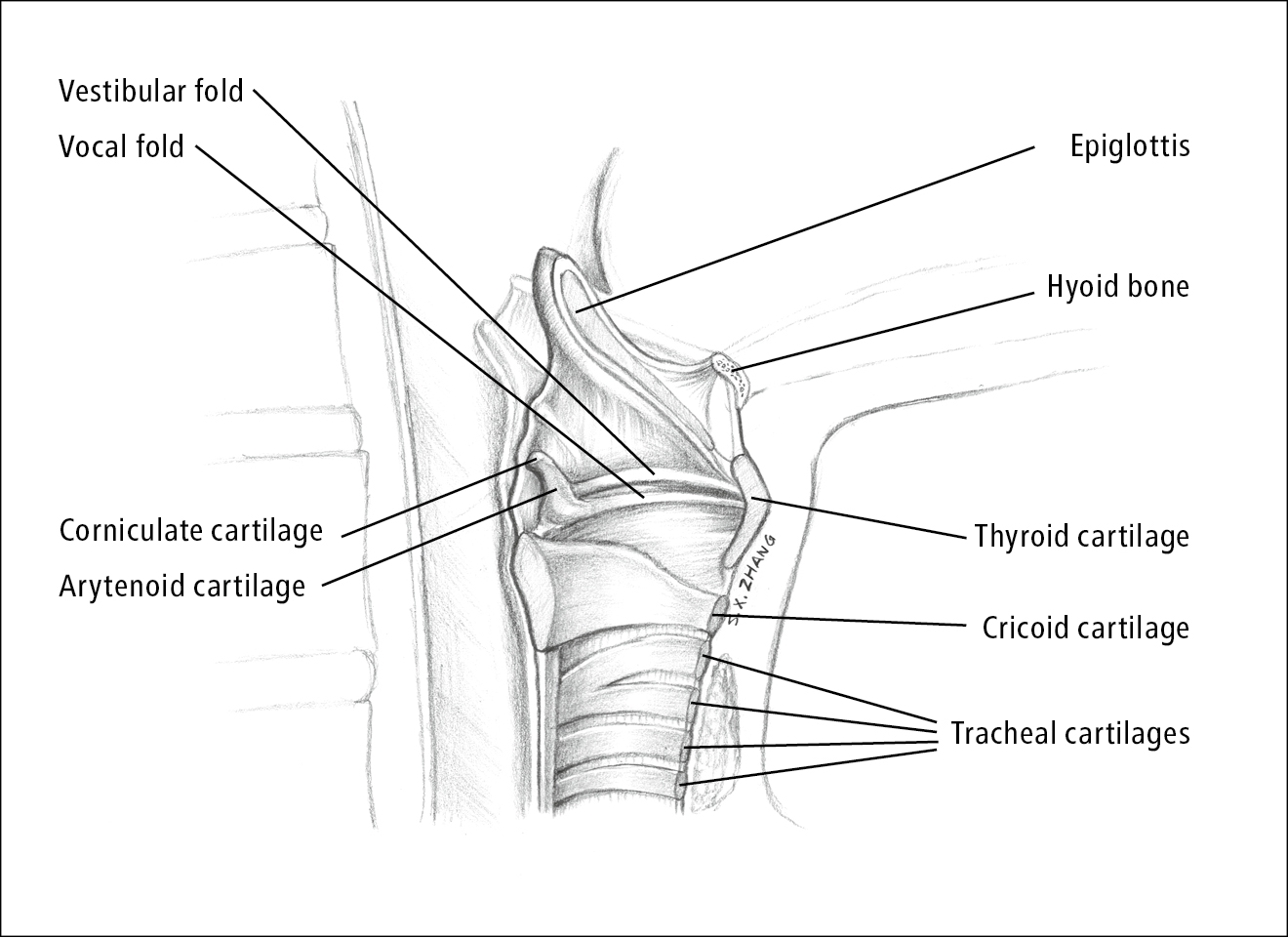
Figure 17.9-1. Larynx anatomy. Illustration courtesy of Dr Shannon Zhang.
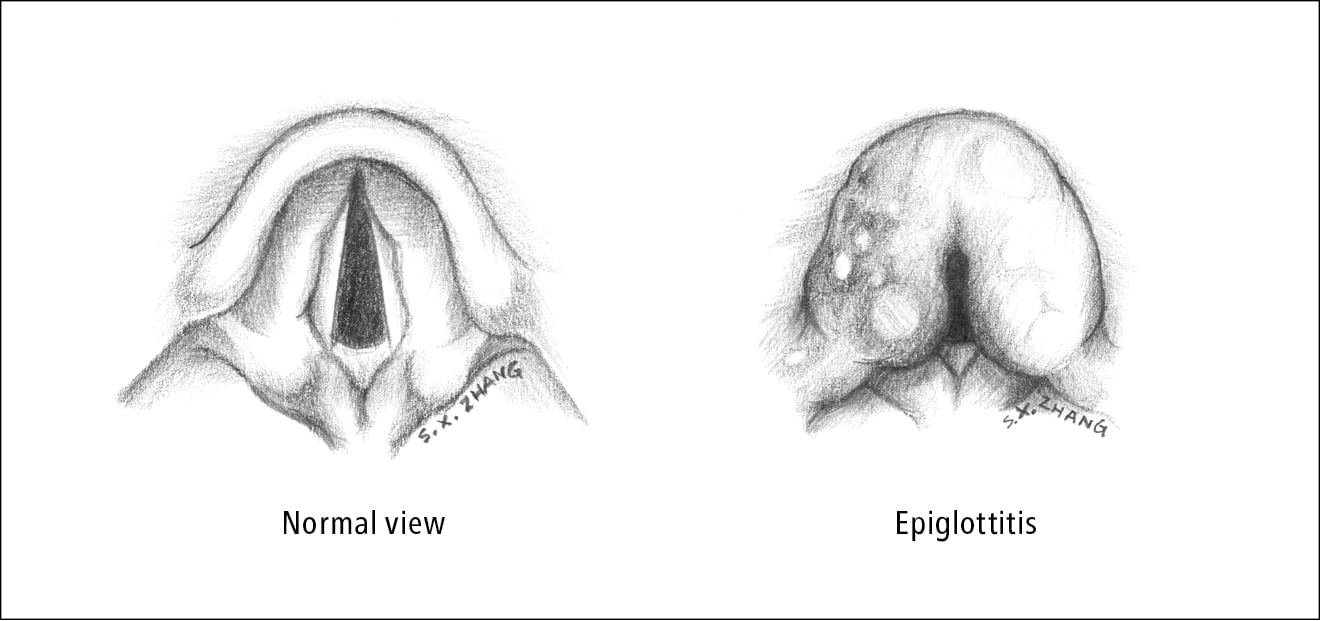
Figure 17.9-2. Epiglottitis. Illustration courtesy of Dr Shannon Zhang.