Etiology and PathogenesisTop
Mechanical obstructions are typically categorized as involving the small or large bowel and may also be classified as being due to intraluminal, intramural, or extramural causes. Small bowel obstructions, which constitute ~75% of mechanical intestinal obstructions, are most commonly caused by intra-abdominal adhesions (from previous surgery, radiation, or other inflammatory processes) or herniae, whereas large bowel obstructions comprise the remaining ~25% and are most commonly caused by tumors, volvulus, and strictures.
The most worrisome complications of intestinal obstruction include bowel necrosis and perforation. Intestinal strangulation may be caused by incarceration of a hernia or by adhesive bands. (An incarcerated hernia refers to any hernia that is nonreducible, whereas a strangulated hernia implies the development of ischemia and/or necrosis.) This usually affects the small intestine but can also involve the mobile (intraperitoneal) portions of the colon. Necrosis of the bowel may develop due to increased pressure in a bilaterally occluded segment, also known as a “closed loop” obstruction. Examples of this phenomenon include incarcerated herniae or large bowel obstruction in the presence of a competent ileocecal valve. Bowel necrosis may also develop by direct compression of mesenteric vessels at the hernia neck. Necrosis may then lead to perforation, peritonitis (usually with development of adynamic ileus), and sepsis.
Less common forms of intraluminal or intramural obstruction include gallstone ileus (caused by gallstones passing through a cholecystoduodenal fistula) or certain parasitic infections, and in exceptional cases tumors of the small intestine. Impacted feces may also impair intestinal passage and sometimes cause symptoms similar to those of mechanical intestinal obstruction.
Clinical FeaturesTop
1. Symptoms: The characteristic triad of symptoms of gastrointestinal (GI) obstruction, which may include abdominal pain, nausea and vomiting, and retention of gas and stools. Typically the pain is paroxysmal and crampy. If pain character changes to being constant and either focal or diffuse, it should be suspicious for bowel ischemia or necrosis with accompanying peritonitis.
2. Signs: Attention on general inspection should be paid to signs of toxicity or hypoperfusion. Volume status assessment should be performed. Abdominal examination should be undertaken, with careful inspection of the entire abdomen and inguinofemoral region for signs of either surgical scars or herniae. High-pitched tinkling bowel sounds have been described in small bowel obstruction. Percussion may reveal lack of liver dullness as a sign of complications (hollow viscus perforation). Palpation should assess for evidence of herniae and for any evidence of peritoneal irritation. A rapidly deteriorating clinical status or physical examination may indicate intestinal necrosis. It is important to note that by the time the patient manifests evidence of peritonitis, irreversible ischemia or bowel necrosis has usually developed.
DiagnosisTop
It is crucial to promptly establish indications for surgery in patients with strangulation and subsequent intestinal ischemia. Diagnostic clues may be provided by examination of the inguinal areas (hernia), presence of postoperative scars (adhesive bands), and history of alternating constipation and diarrhea, as well as progressive impairment of stool and gas passage (colorectal cancer). Digital rectal examination may reveal an anal or rectal tumor or impacted feces.
1. Complete blood count (CBC): A progressive increase in hematocrit and red blood cell counts may be observed that is proportional to the degree of dehydration. A rapid increase in white blood cell counts is often observed in patients with intestinal necrosis.
2. Blood biochemical tests: Because intestinal obstruction may lead to fluid and electrolyte disturbances as well as kidney failure and acidosis, it is necessary to measure serum electrolyte levels, kidney function parameters, and blood gas levels. Other tests may include lactic acid levels and coagulation parameters.
3. Imaging studies:
1) Plain abdominal radiographs in the upright (eg, standing or, in severely ill patients, sitting), supine, and decubitus positions may reveal fluid levels in the distended intestinal loops (Figure 7.2-17). These are caused by a combination of aerophagia and fermentation of stagnant intestinal contents. Bowel loops are typically collapsed distal to the point of obstruction; however, this is not always the case, particularly in early obstruction. A “gasless abdomen” may also be seen in the setting of bowel obstruction in the event that bowel loops are fluid-filled but without significant gaseous distention.
2) Abdominal computed tomography (CT) may reveal the probable cause and location of obstruction. It is also the test of choice to demonstrate the presence of complete versus incomplete obstruction and may identify complications such as necrosis or perforation. Oral and IV contrast should be administered if possible. Rectal contrast is sometimes used in the setting of suspected distal large bowel obstruction but need not be administered in all cases of bowel obstruction.
3) Abdominal ultrasound might be useful if radiologic examinations are contraindicated (eg, in pregnancy). It may reveal small intestinal obstruction but does not indicate the location or cause.
4. Colonoscopy is used for selected causes of large bowel obstruction. In patients with incomplete obstruction it may be possible to introduce the endoscope above the level of obstruction and perform intestinal decompression, which should facilitate preparation for surgery.
TreatmentTop
Patients should always be referred for surgical consultation because mechanical intestinal obstruction often requires surgical treatment; such patients with mechanical small bowel obstruction should likely be admitted under a surgical service.Evidence 1Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to the observational and retrospective nature of data. Oyasiji T, Angelo S, Kyriakides TC, Helton SW. Small bowel obstruction: outcome and cost implications of admitting service. Am Surg. 2010 Jul;76(7):687-91. PMID: 20698371. The need for, and urgency of, intervention should be determined by the surgeon. It may be necessary to prepare the patient for the procedure, particularly by correcting hypovolemia along with associated electrolyte abnormalities. Since surgery may involve exposure to contents of the GI tract, IV antibiotics are administered prior to procedure but are not otherwise indicated on the basis of obstruction alone.
FiguresTop
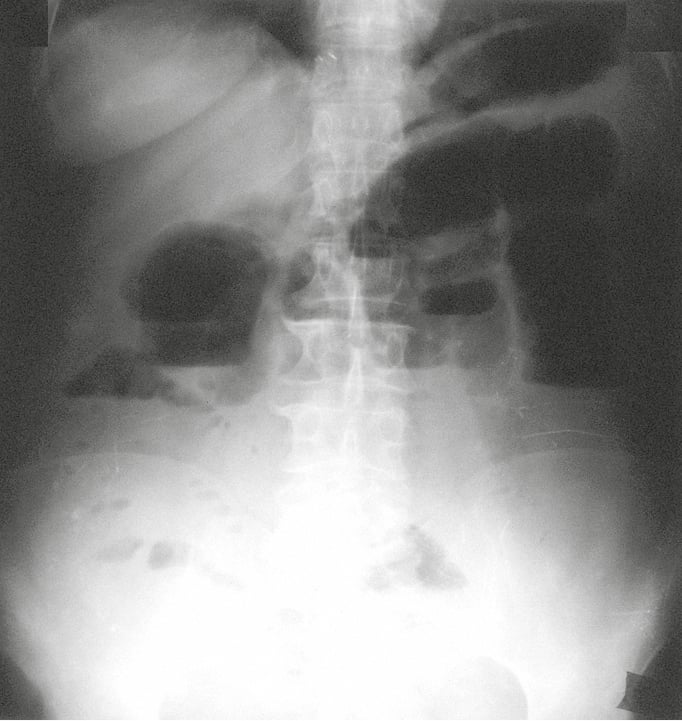
Figure 7.2-17. Plain abdominal radiograph in the standing position. Obstruction of the small intestine with a significant distention of the small intestine and fluid levels visible in a standing position.