Definition, Etiology, PathogenesisTop
Acute cholangitis is a segmental or diffuse acute inflammation of the intrahepatic or extrahepatic bile ducts caused by infection due to impaired or blocked bile outflow (see Figure 7.1-3). Pathogens most commonly involved include Escherichia coli, Klebsiella spp, Enterococcus spp, Enterobacter spp, Streptococcus spp, and Pseudomonas aeruginosa; anaerobic pathogens are involved in 15% of cases.
Risk factors—causes of cholestasis—include choledocholithiasis, tumors obstructing bile outflow (infiltrates in the bile ducts or the papilla of Vater, external compression), postinflammatory and iatrogenic strictures of the bile ducts, primary sclerosing cholangitis, and compression of the bile ducts by a pancreatic cyst or enlarged lymph nodes.
Clinical Features and Natural HistoryTop
Typical clinical signs are the Charcot triad: severe pain of the biliary colic type located in the right upper abdominal quadrant or in the central epigastrium, fever, and jaundice. When hypotension and impaired mental status are additionally present, the syndrome is termed the Reynolds pentad. Tenderness of the right upper abdominal quadrant with abdominal guarding may also be found on clinical examination. Patients may develop septic shock. Untreated bacterial cholangitis is usually fatal.
DiagnosisTop
1. Laboratory tests: Results are similar to those found in patients with choledocholithiasis and additionally include an elevated white blood cell count with a shift to the left in the differential blood count. Severe cholangitis may be accompanied by features of sepsis.
2. Imaging studies: Ultrasonography or computed tomography (CT), magnetic resonance imaging (MRI), or magnetic resonance cholangiopancreatography (MRCP) may reveal dilated intrahepatic and extrahepatic bile ducts, cholelithiasis, or other causes of bile flow abnormalities. In patients with acute cholangitis in whom the cause of obstruction is unclear or the identified abnormalities are amenable to local intervention, urgent endoscopic retrograde cholangiopancreatography (ERCP) (Figure 7.1-1) is the optimal diagnostic technique that allows for simultaneous therapeutic intervention.Evidence 1Strong recommendation (benefits clearly outweigh downsides; right action for all or almost all patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to some heterogeneity among mostly observational studies. Poh BR, Ho SP, Sritharan M, et al. Randomized clinical trial of intraoperative endoscopic retrograde cholangiopancreatography versus laparoscopic bile duct exploration in patients with choledocholithiasis. Br J Surg. 2016 Aug;103(9):1117-24. doi: 10.1002/bjs.10207. Epub 2016 Jun 15. PMID: 27302483. Park CS, Jeong HS, Kim KB, et al. Urgent ERCP for acute cholangitis reduces mortality and hospital stay in elderly and very elderly patients. Hepatobiliary Pancreat Dis Int. 2016 Dec;15(6):619-625. PMID: 27919851. Kiriyama S, Takada T, Strasberg SM, et al; Tokyo Guidelines Revision Committee. TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2013 Jan;20(1):24-34. doi: 10.1007/s00534-012-0561-3. PMID: 23307001. Khashab MA, Tariq A, Tariq U, et al. Delayed and unsuccessful endoscopic retrograde cholangiopancreatography are associated with worse outcomes in patients with acute cholangitis. Clin Gastroenterol Hepatol. 2012 Oct;10(10):1157-61. doi: 10.1016/j.cgh.2012.03.029. Epub 2012 Apr 13. PMID: 22507875.
Diagnosis is based on the characteristic clinical features and results of laboratory or imaging studies.
Other causes of fever and epigastric pain: acute cholecystitis, acute biliary pancreatitis, liver abscess, acute viral hepatitis, diverticulitis, intestinal perforation.
TreatmentTop
All patients should be assessed for severe sepsis and treated appropriately as needed.
1. Stop oral intake of food and fluids.
2. Administer IV fluids. Usually start with isotonic crystalloids.
3. Analgesics and spasmolytics are used as in biliary colic (see Cholelithiasis).
4. Empiric broad-spectrum antimicrobial treatmentEvidence 2Strong recommendation (benefits clearly outweigh downsides; right action for all or almost all patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to indirectness. Solomkin JS, Mazuski JE, Bradley JS, et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis. 2010 Jan 15;50(2):133-64. doi: 10.1086/649554. Erratum in: Clin Infect Dis. 2010 Jun 15;50(12):1695. Dosage error in article text. PMID: 20034345. Kiriyama S, Takada T, Strasberg SM, et al; Tokyo Guidelines Revision Committee. TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2013 Jan;20(1):24-34. doi: 10.1007/s00534-012-0561-3. PMID: 23307001.: Treatment should include coverage for gram-negative bacteria and anaerobes; our regimens, adjusted for local resistance patterns, may include piperacillin/tazobactam, imipenem, or a combination of a third-generation cephalosporin and metronidazole. For moderate to severe cholangitis, antibiotic treatment for 4 days is noninferior to antibiotic treatment for 8 days.
1. The treatment of choice is ERCP with endoscopic sphincterotomy. This may apply even to patients with cholangitis without stones shown on imaging studies.Evidence 3Strong recommendation (benefits clearly outweigh downsides; right action for all or almost all patients). Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to imprecision and indirectness. Kiriyama S, Takada T, Strasberg SM, et al; Tokyo Guidelines Revision Committee. TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2013 Jan;20(1):24-34. doi: 10.1007/s00534-012-0561-3. PMID: 23307001. Hui CK, Lai KC, Wong WM, Yuen MF, Lam SK, Lai CL. A randomised controlled trial of endoscopic sphincterotomy in acute cholangitis without common bile duct stones. Gut. 2002 Aug;51(2):245-7. PMID: 12117888; PMCID: PMC1773318. When necessary, treatment is combined with stenting of the bile ducts to facilitate normal bile drainage.
2. Percutaneous drainage under ultrasonographic or computed tomographic (CT) guidance is used in patients in whom anatomical abnormalities render endoscopic treatment impossible.Evidence 4Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to the observational nature of studies. Kiriyama S, Takada T, Strasberg SM, et al; Tokyo Guidelines Revision Committee. TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2013 Jan;20(1):24-34. doi: 10.1007/s00534-012-0561-3. PMID: 23307001. Takada T, Hanyu F, Kobayashi S, Uchida Y. Percutaneous transhepatic cholangial drainage: direct approach under fluoroscopic control. J Surg Oncol. 1976;8(1):83-97. PMID: 1249944.
3. Surgical drainage is used when other forms of biliary drainage are not feasible or have failed; it is performed very rarely.
FiguresTop
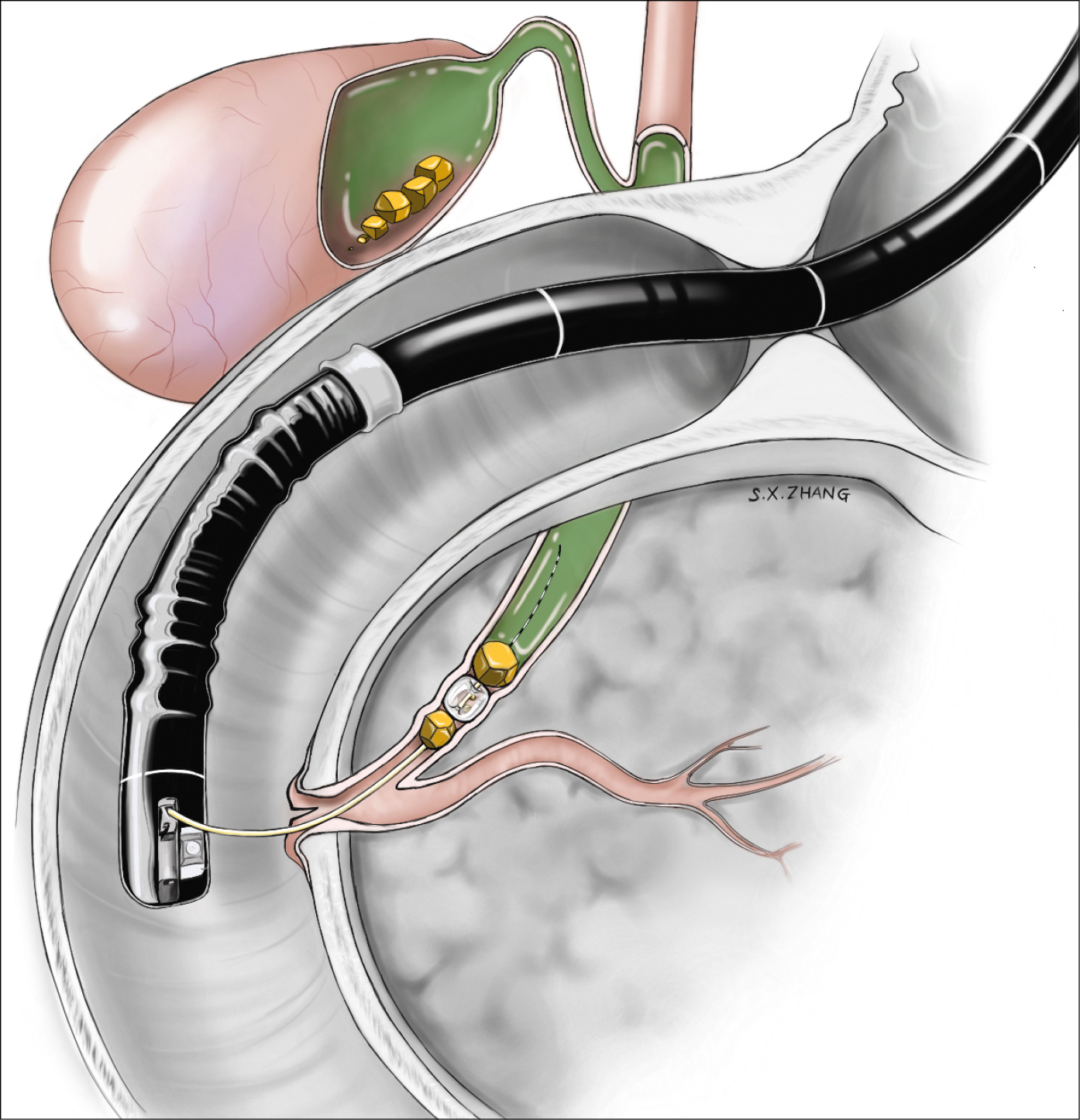
Figure 7.1-1. Endoscopic retrograde cholangiopancreatography (ERCP) with stone extraction. Illustration courtesy of Dr Shannon Zhang.