Shear NH, ed. Litt’s Drug Eruptions and Reactions Manual. 27th ed. CRC Press; January 19, 2021.
Litt’s Drug Eruptions and Reactions database. CRC Press – Taylor & Francis Group. Accessed September 28, 2020. http://www.drugeruptiondata.com
Chang WC, Abe R, Anderson P, et al. SJS/TEN 2019: From science to translation. J Dermatol Sci. 2020;98(1):2-12. doi: 10.1016/j.jdermsci.2020.02.003. Epub 2020 Mar 7. PMID: 32192826; PMCID: PMC7261636.
Dodiuk-Gad RP, Chung WH, Valeyrie-Allanore L, Shear NH. Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: An Update. Am J Clin Dermatol. 2015;16(6):475-493. doi: 10.1007/s40257-015-0158-0. PMID: 26481651.
Sassolas B, Haddad C, Mockenhaupt M, et al. ALDEN, an algorithm for assessment of drug causality in Stevens-Johnson Syndrome and toxic epidermal necrolysis: comparison with case-control analysis. Clin Pharmacol Ther. 2010;88(1):60-68. doi: 10.1038/clpt.2009.252. Epub 2010 Apr 7. PMID: 20375998.
Definition, Etiology, PathogenesisTop
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are life-threatening diseases characterized by mucocutaneous reactions, predominantly induced by drugs. SJS is idiopathic in 25% to 50% of cases. The term toxic epidermal necrolysis spectrum (TENS) has been proposed to define SJS and TEN as manifestations of a single disease entity. SJS involves skin detachment in <10% of body surface area (BSA); SJS/TEN overlap, in 10% to 30%; and TEN, in >30%. The annual incidence is 1.2 to 6 cases per 1,000,000 for SJS and 0.4 to 1.2 per 1,000,000 for TEN.
The etiology includes a combination of several known risk factors such as:
1. Drugs: The most commonly implicated are allopurinol, nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics (especially sulfonamides and penicillins), anticonvulsants (carbamazepine, lamotrigine, and phenytoin), and antiretrovirals.
2. Genetic predisposition: Genetic variants of cytochrome P450 2C (CYP2C) lead to decreased clearance of drugs (eg, anticonvulsants) and increased retention of active metabolites. SJS/TEN has been found to be related to the prevalence of susceptibility alleles in populations of specific ethnicities. For example, the United States Food and Drug Administration (FDA) recommends testing the human leukocyte antigen (HLA)-B*15:02 in Asian populations prior to exposure to carbamazepine. Carriers of HLA-B*5801 are also at a higher risk of allopurinol-induced SJS/TEN.
3. Environment: Immunocompromised patients, such as those with HIV/AIDS and those receiving chemotherapy or a combination of radiotherapy and anticonvulsants, are at increased risk. Infection by agents such as Mycoplasma pneumoniae, herpes simplex virus, and coxsackievirus A6 have also been described to affect susceptibility.
The pathogenesis of the disease is complex. A delayed-type drug hypersensitivity reaction is considered the underlying cause. It involves a variety of cytotoxic T cells, natural killer (NK) cells, and several cytokines, which eventually lead to apoptosis and epidermal necrolysis.
Clinical Features and Natural HistoryTop
SJS/TEN can affect all ethnicities and is more common in women than in men (2:1). The age of presentation ranges between 2 and 78 years, with a mean age of 25 years. The classic latency period is 4 to 28 days and the disease develops as late as 8 weeks after exposure. For anticonvulsants, reactions can occur in the first 2 months of treatment. In the case of re-exposure to the drug, latency can be as short as 2 days.
1. General symptoms: Prodromal phase fever (often >39 or 40 degrees Celsius), sore throat, cough, fatigue, and skin tenderness may occur 1 to 3 days prior to appearance of skin manifestations.
2. Cutaneous manifestations: In early stages SJS/TEN starts as erythematous macules and patches; some of them may have a dusky red or purpuric center creating targetoid-like lesions in some patients. Patches and macules gradually coalesce (Figure 4.7-1, Figure 4.7-2). As the eruption progresses, the skin may take on a characteristic gray hue (Figure 4.7-3). Patients develop flaccid bullae, and then the skin starts to detach from the underlying dermis, creating scalded, raw, and bleeding dermis (Figure 4.7-1, Figure 4.7-2, Figure 4.7-3, Figure 4.7-4). Tense bullae may sometimes be seen on palms and soles, where the skin is thicker. SJS/TEN typically starts on the trunk and later spreads to the neck, face, and extremities. Distal portions of limbs are usually less involved or sometimes spared, but palms and soles are affected in early stages.
The scalp is usually not involved, but alopecia may occur in patients receiving radiotherapy. Nail involvement with paronychia or onycholysis can be observed.
Mucosal involvement (oral, ocular, nasal, anogenital) including the epithelium of the respiratory and gastrointestinal tracts is present in >90% of patients.
Oral involvement occurs in almost all patients, while ocular involvement is seen in ~80% of patients. Oral manifestations include blisters, ulcers, and eroded hemorrhagic plaques on the lips, tongue, cheeks, palate, and gums. Lesions are tender and painful, often associated with an impaired ability to eat, drink, or swallow. Early in the disease eyes often feel scratchy, gritty, and dry.
Subsequent ocular manifestations include photophobia, conjunctivitis, and defects of membranes, pseudomembranes, or both, or of the corneal epithelium, conjunctival epithelium, or both (corneal melt, perforation, infectious keratitis).
3. Hematologic manifestations: Anemia and cytopenias are frequent. Neutropenia is rare but has an impact on prognosis.
4. Pulmonary manifestations: Early pulmonary dysfunction with respiratory distress syndrome (pneumonitis) is observed in 25% of patients. Bronchitis/bronchiolitis with obstructive impairment, bronchiectasis, and respiratory tract obstruction can also occur.
5. Gastrointestinal (GI) manifestations: Dysphagia is the most common feature. Diarrhea and abdominal distention could lead to bowel perforation. Hepatitis and cholestasis can be present.
6. Renal manifestations and electrolyte disorders: In the acute-phase renal failure, tubular necrosis, hematuria, and microalbuminemia are not rare.
7. Infections: Sepsis due to Staphylococcus aureus and Pseudomonas aeruginosa infections is the primary cause of mortality. Factors predictive of bacteremia include hemoglobin ≤100 g/L, existing cardiovascular disease, BSA involvement ≥10%, hypothermia (<36 degrees Celsius), and procalcitonin ≥1 microg/L within 24 hours of blood culture sampling.
8. Other: Multiple organ failure is observed in 23% of patients. Inhibition of insulin secretion, insulin resistance, and hypercatabolic state are frequent.
Sequelae observed in the chronic stage:
1) Cutaneous: Scarring (46%) is common. Irregular pigmentation (77%), milia (15%), urticaria (15%), eruptive melanocytic nevi, chronic pain and pruritus (53%) are frequent. Nail dystrophies including pigmentation, ridging, and anonychia are also seen.
2) Mucosal: Mucosal changes include gingival synechia and recession, dental alteration, xerostomia, hypogeusia, and increased saliva acidity. However, these features are not correlated with their severity in the acute stage.
3) Genital/urogynecologic: Severe SJS/TEN can lead to genital scarring, dyspareunia, and vaginal adhesions in women and to urethral stenosis in both women and men.
4) Ocular complications: Eye complications are present in 64% to 89% of patients and include dry eyes (44%), chronic pain, symblepharon (33%), conjunctival synechiae, entropion, ingrown eyelashes (22%), photophobia (54%), chronic conjunctivitis (22%), and lacrimal duct scarring (22%). The spectrum of ocular syndromes is present in 35% of patients and ranges from sicca to blindness (11%).
5) Bronchiolitis obliterans and interstitial lung disease: Usually seen in the first 6 months of the recovery stage. Increased cough, dyspnea, and airflow obstruction associated with diffuse centriacinar nodules and ground-glass opacities on x-ray should alert the physician to the possibility of this condition.
6) Other: Depression (29%), anxiety (53%), tinnitus, limb amputations, lupus erythematosus, Hashimoto thyroiditis, and irreversibly decreased renal function in patients with preexisting chronic disease can also occur.
DiagnosisTop
We suggest using the mnemonic RASH (remember: appearance/morphology, systemic involvement, histology) and the assessment protocol of 5 d’s (drug exposure, differential diagnosis, determine probabilities of causality, and determine severity [see the SCORTEN scale below]) in the diagnostic workup of SJS/TEN.
1. Physical examination for signs that can suggest skin detachment and are helpful for diagnosis. These include:
1) Nikolsky sign: If there is no exfoliation, applying mechanical pressure with the finger on erythematous zones induces skin detachment and is indicative of SJS/TEN.
2) Asboe-Hansen sign: Flaccid bullae can be displaced laterally if pressure with the thumb is applied.
2. Determining drug exposure and probabilities of causality: An extensive clinical history, including all medications, especially new drugs in the 8 weeks prior to skin reaction, should be taken. It is useful to construct a time line including relevant information for each drug (starting day, dosage, discontinuation day, onset of prodromal symptoms and rash). The probability of causality for each medication should be determined based on previous reports (unlikely, possible, plausible, probable, very probable). The literature (PubMed) and Litt’s Drug Eruption and Reaction Manual and database should be analyzed. Drugs taken intermittently, such as vitamins, sedatives, pain relievers, laxatives, and natural products, must be considered. The ALDEN algorithm has been created to help evaluate the causality of medications and identify not only the most probable problematic drug but also the most harmless one and the ones that could be safely administered in the future.
3. Histopathology: In early lesions scattered apoptotic keratinocytes in the basal and immediate suprabasal layers of the epidermis are often seen. Later stages show subepidermal blisters with overlying confluent necrosis of the entire epidermis and a sparse perivascular infiltrate composed of lymphocytes. Immunohistochemistry shows lymphocytes (CD8+) and macrophages in the epidermis as well as CD4+ lymphocytes in the papillary dermis. Immunofluorescence is required to differentiate SJS/TEN from other autoimmune bullous disorders.
4. Laboratory tests:
1) Serum biochemistry:
a) Complete blood count with differential; glucose, electrolytes, and bicarbonate (arterial) levels; creatinine and urea levels; liver profile; and amylase (inflammatory marker) levels should be investigated. A mild or moderate elevation of hepatic enzymes can be present. These tests are useful to predict prognosis.
b) Serum granulysin levels, cytolytic protein of NK cell levels, and cytotoxic CD8+ lymphocyte count were found to be increased in blister fluid and serum of patients with SJS/TEN. A few studies suggested that the serum granulysin level may be a predictor of disease when SJS/TEN is suspected and may also be useful as a prognostic marker if increased serum levels correspond with poor outcomes. However, serum granulysin measurement is not commercially available in Canada and most of the world.
c) Blood cultures and urinalysis should be performed as indicated to monitor for secondary infections.
2) Imaging: Chest x-ray or computed tomography (CT) should be performed to assess pulmonary involvement.
3) Other investigations and procedures can be considered based on disease severity and involvement of other organs (eg, endoscopy or colonoscopy for GI involvement). Further tests should be considered and performed in specific settings:
a) Pharmacogenomic testing: Identification of biomarkers of disease (HLA alleles) can help prevent the disease and establish early diagnosis and treatment.
b) Molecular testing: Recent advances include enzyme-linked immunospot (ELISpot) assay to detect drug-specific interferon release, cytokine panel, and gene polymerase chain reaction (PCR).
1. Erythema multiforme: Targetoid lesions are distributed on the extremities and face. Mucosal involvement is observed in severe cases. Association with fever and arthralgia is frequent. Risk factors include infections with herpes simplex virus, Mycoplasma pneumoniae, and other pathogens. The disease is rarely induced by drugs.
2. Staphylococcal scalded skin syndrome (SSSS): SSSS is more common in children and presents with perioral and periorbital lesions with radial scale/crust but without intraoral involvement. Histopathology shows subcorneal splitting with normal epidermis.
3. Drug reaction with eosinophilia and systemic symptoms (DRESS): Patients typically have diffuse, erythematous skin lesions accompanied by facial edema and eosinophilia. On histologic examination necrosis is usually absent and a dermal infiltrate with eosinophils is seen.
4. Acute generalized exanthematous pustulosis (AGEP): Patients typically have small, diffuse, nonfollicular pustules and exfoliation. Peripheral neutrophilia is also observed. Histopathology usually shows subcorneal pustules and no necrosis.
5. Generalized fixed drug eruption: Blistering involves a small BSA and there are areas of intact skin. Mucosal involvement is rare or mild, there is no prodrome, and the patient looks generally well. The patient has a history of similar local reactions.
6. Acute graft-versus-host disease (GVHD): Severe cases of acute GVHD can mimic SJS/TEN with diffuse erythroderma, desquamation, bullae, positive Nikolsky sign, and ulceration of mucous membranes. Severe acute GVHD can also present with epidermal necrosis on histologic examination. A history of recent bone marrow and allogeneic hematopoietic stem cell transplant is the key to the diagnosis.
7. Paraneoplastic pemphigus (PNP): Immunofluorescence is often required to differentiate this condition from SJS/TEN.
TreatmentTop
Management of SJS/TEN is complex and should be based on a multidisciplinary approach involving intensivists, dermatologists, ophthalmologists, gastroenterologists, urologists, gynecologists, pharmacologists, immunologists, and later psychiatrists.
1. Discontinuation of the causative drug or the most probable culprit is essential. Avoid other high-risk drugs and monitor the patient for secondary cutaneous adverse drug reactions.
2. Supportive treatment must be administered in an intensive care unit. The patient should be managed in a sterile environment and intravenous catheters should be placed in the noninvolved skin. Temperature regulation (bed with temperature control, aluminum sheets), airway protection, fluid replacement to achieve balance, nutritional control, and pain management should be a priority. Antibiotic prophylaxis is not recommended, but monitoring for infections is mandatory (blood cultures, urinalysis).
3. Wound care is suggested once daily. Healing of areas detached is usually completed in 3 weeks. There are no specific guidelines, but bioactive skin substitutes, semisynthetic or synthetic dressings (silicone dressing, nonadherent layered materials), and topical antibiotics should be considered. Bath with a solution of chlorhexidine 1 mL/5000 mL or spraying the skin bid to tid may be helpful in maintaining the pH balance and avoiding superficial secondary infections. Nondetached areas must be kept dry and not manipulated. Detached areas and pressure sites should be covered with petrolatum gauze. The use of isotonic sterile sodium chloride solution and antibiotic ointments is recommended. Measures for the prevention and management of pressure ulcers should be taken.
4. The mouth should be rinsed several times a day and the anogenital region can be managed with silver nitrate solution (0.5%).
5. Early initiation of intravaginal steroids such as 0.1% betamethasone valerate every 12 hours externally to the vulva may prevent scarring and future strictures. Topical sulfa-containing medications should be avoided.
6. Mild ocular disease can be managed with saline rinses, preservative-free eye lubricants, and eye drops. For more severe eye involvement, topical glucocorticoids and topical antibiotics can be used. In severe cases the placement of the amniotic membrane in the first week could help preserve vision and avoid chronic complications.
Systemic Pharmacologic Treatment
1. IV immunoglobulin (IVIG): The use of IVIG is controversial. Although earlier observational studies suggested a possible benefit, currently there is little or no evidence to support the use of IVIG solely as first-line therapy.
2. Systemic glucocorticoids: The use of systemic glucocorticoids is also controversial. It remains not entirely clear whether these drugs confer a survival benefit in patients with SJS/TEN.
3. Combination of IVIG and systemic glucocorticoids: Limited data are available, but a few small studies suggested that the combination of both treatments may help reduce mortality.
4. Cyclosporine: Although data on the use of cyclosporine are still limited, there is growing evidence that cyclosporine at a dose of 3 to 5 mg/kg/d for 7 to 30 days may reduce mortality and progression of skin detachment. It is believed that cyclosporine can decrease T cell–mediated response and Fas/FasL expression.
5. TNF-alpha inhibitors: There are limited data on the effectiveness of TNF-alpha inhibitors; however, data on etanercept administered as a 25- to 50-microg subcutaneous injection twice a week are promising and suggest a larger healing and mortality benefit than that observed for systemic glucocorticoids (prednisolone at 1-1.5 mg/kg/d).Evidence 1Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to risk of bias and imprecision. Zhang S, Tang S, Li S, Pan Y, Ding Y. Biologic TNF-alpha inhibitors in the treatment of Stevens-Johnson syndrome and toxic epidermal necrolysis: a systemic review. J Dermatolog Treat. 2020 Feb;31(1):66-73. doi: 10.1080/09546634.2019.1577548. Epub 2019 Feb 19. PMID: 30702955. Wang CW, Yang LY, Chen CB, et al; the Taiwan Severe Cutaneous Adverse Reaction (TSCAR) Consortium. Randomized, controlled trial of TNF-α antagonist in CTL-mediated severe cutaneous adverse reactions. J Clin Invest. 2018;128(3):985. doi: 10.1172/JCI93349. Epub 2018 Feb 5. PMID: 29400697; PMCID: PMC5824923.
1. Sunlight exposure should be avoided; use of protective clothing and sunscreens with a sun protection factor (SPF) ≥30 is recommended.
2. Scarring of the skin can be managed with scar massage, silicone sheeting, and pressure dressings. Laser treatment has also been described (with 595-nm pulsed-dye and fractional ablative carbon dioxide lasers).
3. Sunglasses with ultraviolet protection and eye lubricants should be used. Some patients require special lenses to the ocular surface or surgery.
4. Exercise and physiotherapy are important measures to prevent complications and restore physical function. Passive movement and stretching are recommended to prevent contractures.
5. Pulmonary rehabilitation must be started before discharge. Treatment includes antibiotics, bronchodilators, and steroids. However, these treatments do not reverse the deterioration of pulmonary function. Reopening of the obstructed bronchi using a balloon catheter is controversial, as restenosis can occur.
Follow-UpTop
Periodic evaluation should be performed in the first year after discharge. Severe presentation is a risk factor for mortality in the first 3 months. Serious comorbidities and age influence mortality between 90 days and 1 year after the skin reaction.
The patient and their family members must receive an educational session before discharge. A full review of complications affecting the skin and other organs should be conducted. Potential short- and long-term implications on quality of life and mental health should also be taken into account. Formal evaluation of psychologic distress and referral for mental health support should be considered.
Patients and their families should be provided with information on the diagnosis and the drugs to avoid or the ones that are safe to take in the future. They should be advised to use a medical ID alert bracelet. Family counseling is important due to genetic predisposition.
The use of patch testing to confirm causality after discharge is controversial. Until now there has been no reliable test (including patch testing) for the identification of the causative drug. There is also an ethical issue with the possibility to induce the same reaction, another hypersensitivity to a drug that the patient was not previously sensitized to, or anaphylactic reaction.
PrognosisTop
The disease progresses within 4 to 5 days following initial presentation. The course is unpredictable, but identifying the causal agent and discontinuing its use highly correlates with better prognosis. Mortality is 1% to 5% for SJS and 30% to 50% for TEN. Death is more common in the elderly and those with extensive skin involvement.
Estimated prognosis can be obtained by applying the severity of illness score (SCORTEN) scale (www.mdapp.co), which is based on 7 prognostic factors, each adding 1 point to the final score:
1) Age >40 years.
2) Heart rate >120/min.
3) Glucose level >14 mmol/L.
4) Serum bicarbonate level <20 mmol/L.
5) >10% of BSA involved.
6) Serum urea level >10 mmol/L.
7) Presence of malignancy.
The mortality for 0 to 1 point is estimated at 3%; 2 points, 12%; 3 points, 35%; 4 points, 58%; and ≥5 points, ~90%.
The number of medications used, serum creatinine level, neutropenia, lymphopenia, and thrombocytopenia have also been linked to poor outcome.
Special ConsiderationsTop
1. Children and young people: The incidence of SJS/TEN is lower in children compared with adults (0.4 cases per 1,000,000 children per year vs 0.8 per 1,000,000 adults per year). The most commonly identified causative drugs are anticonvulsants in 60% of patients (carbamazepine, phenobarbital, and lamotrigine) followed by antibiotics in 26% (sulfonamides and penicillins). The most frequently implicated infectious agent is herpes simplex virus (19.7%). Mortality also seems to be lower for both SJS (0%-4%) and TEN (16%) in this age group. Predictors of mortality include large BSA involved, renal failure, underlying malignancy, sepsis, and epilepsy.
2. Immunosuppressed patients: Immunosuppressed patients (eg, HIV-positive patients treated with nevirapine) are at higher risk of developing SJS/TEN.
3. Pregnancy: Fetal stress may result in premature labor, and secondary vaginal scarring can occur due to injuries sustained during labor, which can lead to long-term painful lesions, stenosis, vaginal adenosis, and telangiectasia. Cesarean section has been used in many cases to avoid mucous membrane involvement of TEN. Most babies present as healthy, but there are a few reports of simultaneous TEN in newborns.
4. SJS/TEN and coronavirus disease 2019 (COVID-19): Both diseases have been described to share similar pathogenesis (cytokine storm), which raises a speculation that COVID-19 could potentially be treated with etanercept.
FiguresTop

Figure 4.7-1. A patient with TEN involving 90% of body surface area. Erythema, epidermal sloughing, and bullae leaving diffuse, raw-appearing skin regions are apparent. Photograph courtesy of Dr Neil H. Shear.
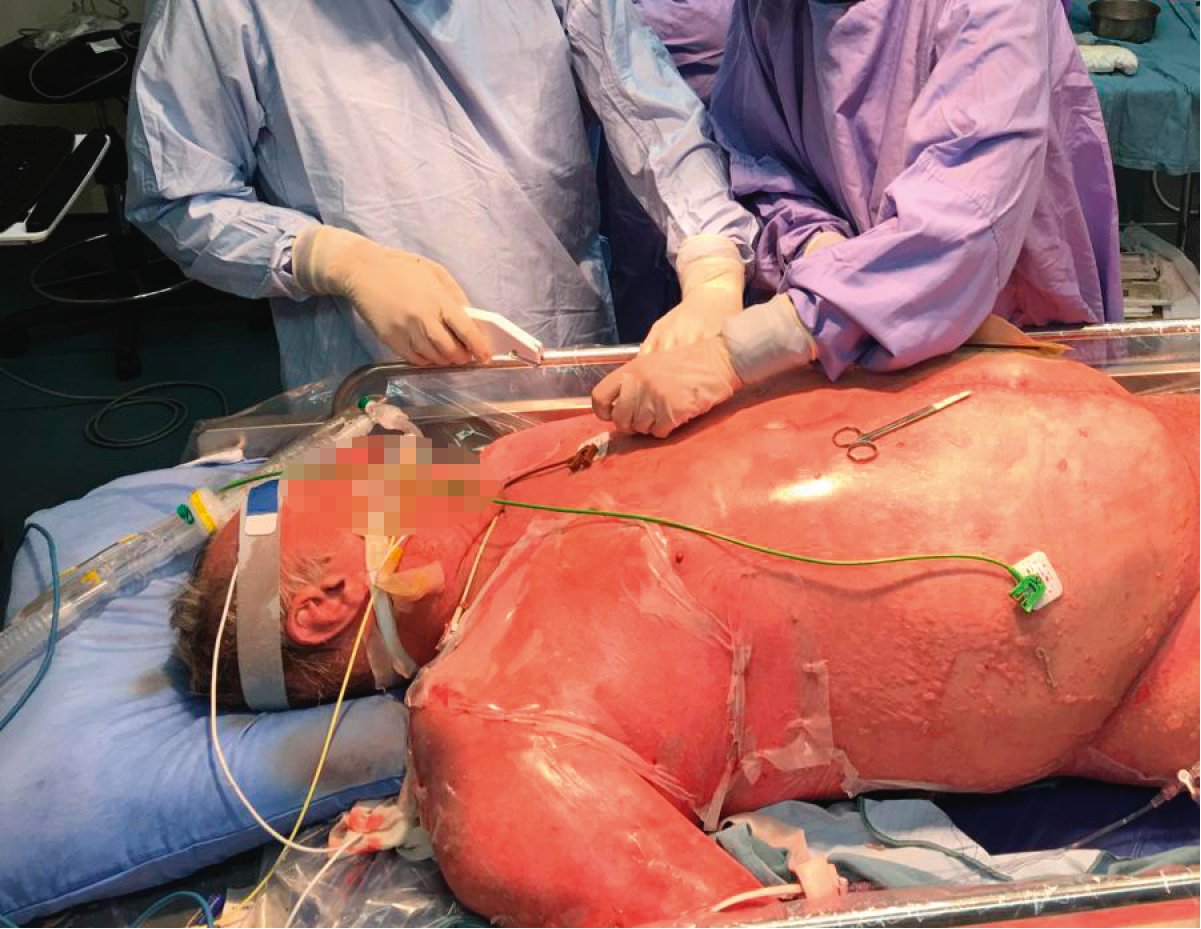
Figure 4.7-2. A patient with TEN. Diffuse erythema and sloughing with bullae and vesicles on the right side of the abdomen. Photograph courtesy of Dr Neil H. Shear.

Figure 4.7-3. Exfoliation and necrosis of the skin on the back and buttocks. Gray hue of the skin is a characteristic feature indicative of disease progression. Photograph courtesy of Dr Neil H. Shear.

Figure 4.7-4. Necrotic lesions and detached skin yielding a “cigarette paper” appearance in a patient with SJS/TEN. Photograph courtesy of Dr Neil H. Shear.