Related McMaster Perspective episodes
McCullagh D, Chu D, Jaeschke R. Penicillin allergy in the hospital. McMaster Textbook of Internal Medicine. Published April 10, 2019.References
McCullagh DJ, Chu DK. Penicillin allergy. CMAJ. 2019 Feb 25;191(8):E231. doi: 10.1503/cmaj.181117. PubMed PMID: 30803953; PubMed Central PMCID: PMC6389453.This transcript has been edited to include additional commentary on the issue of cross-reactivity between penicillins and cephalosporins.
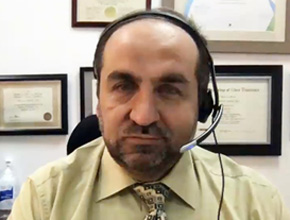
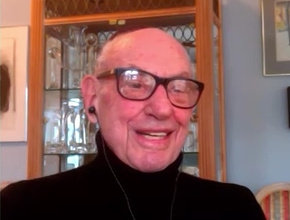
Roman Jaeschke, MD, MSc: Good afternoon, welcome to the second part of the interview on the importance of and testing for penicillin allergy. Previously we were talking about implications for acute in-hospital care [see Penicillin allergy in the hospital]. Now I would like to concentrate on a more outpatient situation, where the patient whom you see for the first or second time says, “By the way, I have a penicillin allergy history.” How should a primary care provider behave in such situations? What should a family doctor think and do?
David McCullagh, MD: I think a family doctor should approach this in the same way as a hospital doctor, although there is probably—or hopefully—less urgency.
A family doctor should be looking at the patient’s penicillin allergy status and thinking that this is a status that in maybe 90% of cases or more is not going to be a true allergy. This has significant detrimental effects both for the patient and for the health-care system. They should be taking a full allergy history of the patient and trying to classify them into one of 3 risk category groups.
Firstly, there would be a patient who is a similar risk category as the general population. This would be someone who has had a known nonimmunologic side effect of the drugs, such as nausea, gastrointestinal disturbance. Those patients should not be labelled with allergy. That allergy status could be removed and the patient could be educated as to why the status is removed and the benefits to them of having that status removed.
Secondly, people with a family history also should not have an allergy status and are at the same risk as the general public. I think a family doctor should be comfortable in removing the allergy status from a patient who falls into that category.
There is a high-risk category, which is a second category that encompasses people who had a severe, delayed, immunologic reaction to penicillin, such as acute interstitial nephritis, toxic epidermal necrolysis, Stevens-Johnson syndrome, or a drug reaction with eosinophilia and systemic symptoms, amongst others. These patients who have a penicillin allergy status confirmed are high risk and should be warned to avoid this class of medications.
The third risk category group is the more interesting and refers to people who have an intermediate status. These are people who maybe do not know their allergy or had a potential IgE-mediated acute hypersensitivity reaction as a distant event, so perhaps a rash when they were a child. These patients would benefit from further evaluation by an allergist and potentially from allergy testing. It would be worthwhile for these patients to be referred to an allergist as an outpatient for further evaluation.
Roman Jaeschke: Thank you. This was the opinion of a person specializing in infectious diseases, Doctor David McCullagh. We also have a person specializing in allergy, Doctor Derek Chu. Derek, these people will be referred to you. How would you proceed?
Derek Chu, MD, PhD: Like Doctor McCullagh said, the first step is to weed out or classify those that are clearly not allergic. When they come to see us, what we are going to be doing is reconfirming that risk stratification. If they are clearly not allergic, we may not even go on to do skin testing and may even avoid challenging them to the drug, because from the history alone it may be clear that they are not allergic whatsoever.
Likewise, we are looking for contraindications, that high-risk category of severe delayed hypersensitivity reactions.
For the middle category, which is going to be the majority of the patients, we would then proceed with skin testing, which is typically intradermal testing to components of penicillin that cause allergic reactions. If they are negative, we would proceed to challenging the patient to the drug. For amoxicillin, it would be something as simple as oral amoxicillin 500 mg times one. If they tolerate that, they can have it removed from their medical record.
Roman Jaeschke: This would follow the intradermal allergy testing to start with, with much smaller amounts of a penicillin substrate, correct?
Derek Chu: Correct. There are miniscule amounts, typically in the order of 20 to 30 microliters. That is a classical approach.
There is some debate as to whether or not one can go directly to challenge without even doing skin testing, but that is controversial.
Roman Jaeschke: The other question on my part would be the cross-reactivity between cephalosporins and penicillins in both directions. The patient may report a penicillin allergy. What is the chance that they are allergic to cephalosporin? Or the other way around: they got Keflex or Cefuroxime on some occasions and they had an untoward reaction, which puts them into a higher-than-low-risk category.
Derek Chu: The best data comes from only one direction, unfortunately, which is penicillin to cephalosporin. The cross-reactivity between penicillins and cephalosporins (any generation) is thought to be low, in the order of 1% to 5%. The other way around is not as well studied, but the general impression is that it is, again, low. How low? Is it the same order of magnitude of a few percent? That is what the data is saying but it is still early days.
Second consideration is that there is a wide library of theoretical cross-reactivity, which has not been borne out by rigorous clinical studies yet. Specific considerations about which drugs may or may not cross-react are largely still in the laboratory phase, without clinical studies, and you may receive varying advice between allergists.
Roman Jaeschke: That is usual for doctors. David, any final advice or words of wisdom?
David McCullagh: I would just reiterate that this intervention is something that is best done as an outpatient and when the patient is well, and not left for a time when the patient is potentially ill or needs an antibiotic. Preplanning and preventative medicine is the best case in this situation and it would be of benefit to both the patient and health-care system at large to clarify or dispel a penicillin allergy label.
Roman Jaeschke: Thank you. My last request would be that you send the link to your article in the Canadian Medical Association Journal. Thank you very much for your time.
 English
English
 Español
Español
 українська
українська