Dr Derek Chu, clinician scientist at McMaster University, connects with Dr Roman Jaeschke to discuss the just-published meta-analysis from The Lancet that reviews evidence for the use of physical distancing, facemasks, and eye protection in the prevention of coronavirus transmission.
References
Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. Published online June 1, 2020. doi:10.1016/S0140-6736(20)31142-9. Accessed June 2, 2020.Click here for Publications of the Week discussing findings of the study.
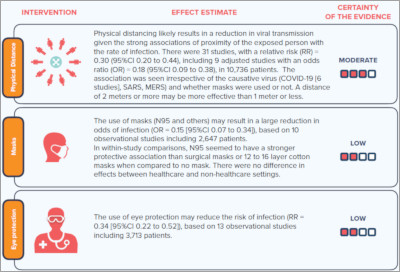
Infographics
Click to view the full image.
Infographic summarizing findings of The Lancet publication courtesy of the meta-analysis authors.
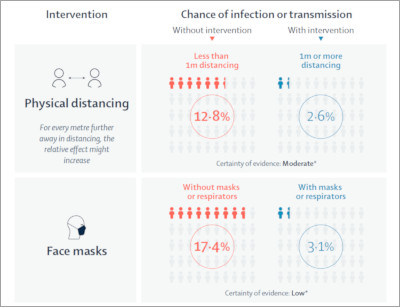
Click to view the full image.
Infographic summarizing findings of The Lancet publication.
Transcript
Roman Jaeschke, MD, MSc: Good morning. Welcome to another edition of McMaster Perspective. I have the pleasure of reintroducing Dr Derek Chu, who’s the first author of a systematic review and meta-analysis published in The Lancet on the efficacy of measures that we all hear are advocated: social or physical distancing, masks, and eye shields. I have to say these are fascinating results.
I’ll start by asking Dr Chu to tell us in a few words the history of this analysis and his interpretation of the results.
Derek Chu, MD, PhD: Thank you so much. I’m glad to be here. I’ll be speaking on behalf of the COVID-19 SURGE (Systematic Urgent Review Group Effort) group authors, who are behind this World Health Organization (WHO)-commissioned rapid review.
At the end of March, we were able to assemble a team of about 40 individuals, led by a number of McMaster-associated investigators, including Holger Schünemann, Elie Akl, and myself, to try to address the question of physical distancing, mask use, as well as eye protection. Although my specialty background is both being a general internist and a clinical immunologist and allergist, the impact of coronavirus disease 2019 (COVID-19) has been widespread and germane to all specialties. I thought this was a very important topic to address in the context of the current pandemic, plans to reopen, and future pandemics.
We were able to very rapidly synthesize the global literature from over 20,000 records and distill them down to about 44 observational, or nonrandomized, studies evaluating quantitatively the impact of physical distancing measures, eye protection, as well as mask use. In total, there were about 26,000 participants from 16 countries and 6 continents, of which about 6500 had COVID-19.
For the physical distancing measures, we found that there was a dose response between how close an individual was to somebody infected and their risk of transmission. Going from 0 meters to 1 meter and to 2 meters, each time the relative effect would be doubled. At a cutoff of about 1 meter, this was approximately an adjusted odds ratio of 0.18.
Roman Jaeschke: So a 5-fold decrease in the risk of infection achieved by maintaining the distance of 1 meter. That’s quite amazing. And if I’m correct, your baseline risk of transmission was about 15%. So from 15 out of 100 you went down to about 3 out of 100.
Derek Chu: That’s correct.
Roman Jaeschke: With 1 meter.
Derek Chu: Exactly. This was an association that we were able to find in both health-care settings and community settings. It helps to inform precisely what is the optimal safe distance but also how to inform contact tracing, what is the distance at which someone’s going to be at risk for transmission, and how to model future efforts to plan for how to come out of the current lockdown and how to plan for future pandemics.
Roman Jaeschke: I have to say we keep hearing about the importance of distancing but these numbers are truly staggering. They probably will change my behavior at the moment.
Going from 1 meter to 2 meters, if I heard correctly, halves the risk again.
Derek Chu: Correct. The relative risk reduction increases by about 2-fold, which we’re able to see by metaregression. This means that it may be worthwhile to rethink what our standard should be. Although 1 meter is quite effective, there may well be a need to create a uniform standard, because guidance varies globally. Some jurisdictions use 1 meter, other use 2 meters, and we may want to settle on 2 meters.
Roman Jaeschke: I guess it depends on how many people are around to allow this extent of distancing. This is incredibly useful knowledge of the extent to which physical distancing affects the infection rate. Any other comments on this part?
Derek Chu: One implication is trying to find a uniform standard for contact tracing and optimal physical distancing. One subtle but perhaps important implication is that countries using the imperial system could benefit from moving towards a defined standard of 2 or more meters. If we think about the typical 6-feet rule, this is actually short, it’s 1.8 meters. But the metaregression and the findings of this study show that increasing this to 2 meters or more, which should be about 6.5 or 7 feet, would make a significant difference.
Roman Jaeschke: We’ll see how our colleagues in the United States react to this and whether they’ll change the imperial system to a different one.
We’ve talked about distancing. How about masks? What have you found there?
Derek Chu: The mask question has been quite contentious for some time and debated heavily between different pandemic scenarios. You might recall that history has taught us that even after the Spanish flu universal masking was quite common.
When we looked at the data for COVID-19, we understood there was some confusion as to whether the biologic rationale of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) being aerosolized or not should dictate what mask is more effective. By systematically analyzing all available data across severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and COVID-19, we were able to find that firstly, mask use had a strong association with protection in both health-care settings and community settings, and secondly, there appears to be a potential hierarchy in the effectiveness of masks and respirators. Respirators mean a number of different things. The most common that we’ll be familiar with are N95, and they have similar names in other jurisdictions, such as in China or Europe. The facemasks, such as surgical masks or multilayer cotton or gauze masks, were less effective in comparison to the respirators.
Roman Jaeschke: If I read the results correctly, the first impression I had is that the efficacy of masks was similar to 1 meter of physical distancing or to 2 meters in the case of potentially more effective masks. That’s just eyeballing the effect.
The other issue, obviously, is the relative safety or efficacy of those masks. We have more surgical masks than N95 masks. The efficacy and benefit of using one versus the other may depend on the underlying risks of acquiring infection. Correct?
Derek Chu: Absolutely correct. The implications of this study are that we must consider not only the potential efficacy or effectiveness of the individual mask types and the setting in which they’re used, but also the baseline risk that the wearer is going to be facing and contextual considerations, such as acceptability, feasibility, and values and preferences.
Roman Jaeschke: I’m using an N95 mask and it’s not easy to have it on for 10 minutes, and certainly it’s not easy to have it on for longer periods.
If I read the numbers correctly, the surgical masks take away about two-thirds of the risks, the N95 may be taking another two-thirds of what is left, or they may take 90% of the underlying risk versus surgical masks taking about 70%; these are obviously approximations. And there is the issue of inconvenience and functioning in those masks, which differs as well. What should we advise people? What would be the clinical implications? You probably were discussing this extensively among your colleagues.
Derek Chu: It’s exactly how you’ve articulated it. Those are some of the key issues. First of all, we have to consider the use of masks for the health-care setting and for the community setting. For the health-care setting, it may be worthwhile to give consideration to the rational use of masks right now and upscaling production of respirators for future use.
Secondly, we have to consider in which situations people will be at highest risk in order to use the highest level of protection to take away those last two-thirds [of the risk]. As you summarized, both surgical masks and respirators are highly effective. That incremental benefit from a surgical mask to a respirator may be most helpful in those that are going to face a very high-risk situation. However, [it is challenging to formulate] the exact policies to dictate what are the highest-risk situations.
The other thing is that when we think about baseline risk from a methodologic perspective, typically we think of it as a long-term static number. In reality, as we face patients day to day and interact with them, the baseline risk can change rapidly and dynamically. So it may be worthwhile to consider that under specific scenarios N95 respirators would be more frequently used than, say, surgical masks. But in more general scenarios, where the baseline risk is quite static, perhaps that two-third risk reduction is meaningful enough as a protection and minding resources at the current time.
Roman Jaeschke: And availability, obviously.
If I were to summarize this for a layperson who hears about it from an expert, we should start using N95 respirators in the highest-risk situations and as their availability increases, we could start using them in lower-risk situations, assuming that people are willing to endure the inconvenience of those masks.
This is correct assuming that our data, or your data, are valid. These were all observational studies. Is there enough uncertainty to continue with randomized controlled trials (RCTs) to establish the existence and extent of benefit?
Derek Chu: You’re right. Even though we found a very strong association with protection, we were very cautious and mindful not to be overly confident in the quantitative estimates of effect, the precise value that we have estimated with meta-analysis. We rated the overall certainty of the body of evidence for the quantitative estimates as low, even though there were very strong signals for protection. To gain much higher confidence in the actual estimates of effect, we do need rigorous RCTs.
Secondly, we may be more confident in the qualitative estimate or direction of effect, but knowing the precise magnitude is going to be quite critical to improve our understanding of COVID-19 in the future.
Roman Jaeschke: I find the results of this meta-analysis very useful and fascinating.
You told us about physical distancing and masks. What are your conclusions from looking at the effects of using eye protection?
Derek Chu: When it comes to eye protection, the best-studied interventions were goggles or full face shields, and these were also highly effective for reducing transmission. Therefore, this should be considered perhaps as being routine for high-risk situations, but one might also consider using eye protection—perhaps even extrapolated to simple eyeglasses or spectacles—for the community setting. This is particularly important during close quarters contacts or as we think about reopening safely.
Roman Jaeschke: This applies to coronaviruses only or coronaviruses and influenza?
Derek Chu: We specifically studied all coronaviruses that are associated with epidemics—SARS, MERS, and COVID-19—for the eye protection situations.
Roman Jaeschke: How big is this risk? We obviously think about sneezing, coughing, and even breathing. How to compare the risks associated with eye transmission? Is it comparable?
Derek Chu: The overall risk reduction with the use of eye protection was quite significant, on the order of a 5-fold reduction in the adjusted odds ratio. This does mean that it can have a meaningful effect, particularly when we think about mucosal transmission being a quite common route of transmission.
Roman Jaeschke: So again, with close contact it’s similar to the efficacy of masks.
Derek Chu: Yes.
Roman Jaeschke: Thank you very much. Fascinating results on all 3 fronts: physical distancing, masks, and eye protection. I am pretty sure this meta-analysis will influence how we all behave. Thank you so much.
Derek Chu: Thanks again.
 English
English
 Español
Español
 українська
українська