Ganesan G, Ponniah S, Sundaram V, et al. Whole lung irradiation as a novel treatment for COVID-19: Final results of the prospective randomized trial (WINCOVID trial). Radiother Oncol. 2022 Feb;167:133-142. doi: 10.1016/j.radonc.2021.12.024. Epub 2021 Dec 25. PMID: 34958809; PMCID: PMC8709793.
Eroglu SE, Algin A, Bulut SSD, et al. Diagnostic performance of thorax CT in mildly symptomatic COVID-19 patients: The importance of atypical CT findings. North Clin Istanb. 2021 Oct 19;8(5):425-434 doi: 10.14744/nci.2021.81557. eCollection 2021. PMID: 34909580; PMCID: PMC8630726.
Hossein H, Ali KM, Hosseini M, Sarveazad A, Safari S, Yousefifard M. Value of chest computed tomography scan in diagnosis of COVID-19; a systematic review and meta-analysis. Clin Transl Imaging. 2020;8(6):469-481. doi: 10.1007/s40336-020-00387-9. Epub 2020 Oct 12. PMID: 33072656; PMCID: PMC7549426.
Pang C, Hou Q, Yang Z, Ren L. Chest computed tomography as a primary tool in COVID‑19 detection: an update meta‑analysis. Clin Transl Imaging. 2021;9(4):341-351. doi: 10.1007/s40336-021-00434-z. Epub 2021 May 26. PMID: 34055674; PMCID: PMC8149579.
Mohammad Karam M, Althuwaikh S, Alazemi M, et al. Chest CT versus RT-PCR for the detection of COVID-19: systematic review and meta-analysis of comparative studies. JRSM Open. 2021 May 15;12(5):20542704211011837. doi: 10.1177/20542704211011837. eCollection 2021 May. doi: 10.1177/20542704211011837. PMID: 34035931; PMCID: PMC8127597.
Tabatabaei SMH, Talari H, Moghaddas F, Rajebi H. Computed Tomographic Features and Short-term Prognosis of Coronavirus Disease 2019 (COVID-19) Pneumonia: A Single-Center Study from Kashan, Iran. Radiol Cardiothorac Imaging. Published online April 20, 2020. doi: 10.1148/ryct.2020200130.
Rubin GD, Ryerson CJ, Haramati LB, et al. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology. 2020 Apr 7:201365. doi: 10.1148/radiol.2020201365. [Epub ahead of print] PubMed PMID: 32255413.
Bernheim A, Mei X, Huang M, et al. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology. 2020 Feb 20:200463. doi: 10.1148/radiol.2020200463. [Epub ahead of print] PubMed PMID: 32077789.
Wong HYF, Lam HYS, Fong AH, et al. Frequency and Distribution of Chest Radiographic Findings in COVID-19 Positive Patients. Radiology. 2019 Mar 27:201160. doi: 10.1148/radiol.2020201160. [Epub ahead of print] PubMed PMID: 32216717.
Vaseghi G, Mansourian M, Karimi R, et al. Clinical characterization and chest CT findings in laboratory-confirmed COVID-19: a systematic review and meta-analysis. medRxiv doi: 10.1101/2020.03.05.20031518.
Dobranowski J, Dobranowski AJ, Levinson AJ. The Portable (AP) Chest X-ray: The critically ill patient. In: Discover Radiology: Chest X-Ray Interpretation. J2d Publishing Inc; 2014:706-730.
IntroductionTop
Chest radiography (x-ray) and computed tomography (CT) are the most often used imaging modalities in the care of critically ill patients. Both are commonly available.
Chest radiography has the advantage of being available as a portable study, mitigating the need for transporting patients to the radiology department. Portable chest radiography examinations are valuable in assessing the placement of lines, tubes, and other devices. In addition, they are useful in identifying complications of ventilation and following the progression of parenchymal lung changes. However, portable chest radiography has limited value in the detection of early disease.
CT has multiple advantages over conventional chest radiography and other imaging modalities. CT scans display the chest anatomy at a high-contrast resolution and without issues related to the superimposition of structures. Modern CT scanners allow for fast acquisition of axial scans, which can also be viewed in coronal or sagittal planes. High-resolution CT imaging allows for visualization of fine details of the normal and abnormal lung parenchyma. CT scanning of the thorax with contrast injection is essential for the evaluation of suspected pulmonary embolism.
IndicationsTop
On April 7, 2020, the Fleischner Society published a consensus statement regarding the role of chest imaging in patient management during the coronavirus disease 2019 (COVID-19) pandemic.
1. Main recommendations:
1) Imaging is not routinely indicated as a screening test for COVID-19 in asymptomatic individuals.
2) Imaging is not indicated for patients with mild features of COVID-19 unless they are at risk for disease progression.
3) Imaging is indicated for patients with moderate to severe features of COVID-19 regardless of COVID-19 test results.
4) Imaging is indicated for patients with COVID-19 and evidence of worsening respiratory status.
5) In a resource-constrained environment with limited access to CT, chest radiography may be preferred in patients with COVID-19 unless features of worsening respiratory status warrant the use of CT.
2. Additional recommendations:
1) Daily chest radiographs are not indicated in stable intubated patients with COVID-19.
2) CT is indicated in patients with functional impairment, hypoxemia, or both after recovery from COVID-19.
3) COVID-19 testing is indicated in patients with incidentally detected findings suggestive of COVID-19.
Chest RadiographyTop
Chest radiography examinations performed in patients with COVID-19 show a spectrum of findings, from normal in early disease to patchy or diffuse asymmetric air-space opacities in later stages (Figure 20.1-1, Figure 20.1-2). The opacities may show bilateral lower-zone and peripheral predominance with peak visualization at 10 to 12 days from the onset of symptoms.
Computed TomographyTop
For the CT scan, the patient is supine. The examination is performed with images acquired during full inspiration and with a single breath hold. A low-dose technique can be used, which allows for adequate lung parenchyma visualization while minimizing the radiation dose to the patient. No intravenous (IV) contrast is necessary.
If pulmonary embolism is clinically suspected, the CT scan should be performed following IV contrast administration and according to a pulmonary embolism protocol. The lung parenchyma will also be adequately visualized on such scans. Appropriate modifications to the protocol need to be made if the patient is ventilated, uncooperative, or cannot take and hold a deep breath. In these patients the image quality may be significantly reduced.
CT scans performed in patients with COVID-19 show several parenchymal lung changes:
1) Ground-glass opacities (Figure 20.1-3, Figure 20.1-4): Areas of lung opacification (too white) that do not obscure underlying bronchial structures or blood vessels.
2) Consolidation (Figure 20.1-5, Figure 20.1-6): An area of lung opacification that obscures underlying bronchial structures or blood vessels.
3) Linear opacities.
4) Bronchial wall thickening (Figure 20.1-7).
5) Reverse halo sign (Figure 20.1-8): An area of ground-glass opacity surrounded by a concentric ring of consolidation.
6) “Crazy paving” pattern (Figure 20.1-9): The appearance of ground-glass opacity with associated interlobular and intralobular septal thickening.
Additional rare CT findings include pleural effusion and pericardial effusion.
The most common CT lung findings in early disease are ground-glass opacities, consolidation, or a combination of ground-glass opacities and consolidation (Table 20.1-1). The lung opacities are usually round with a peripheral distribution (Table 20.1-2).
At later stages of the disease there is further progression of ground-glass opacities and consolidation. The total number of lobes involved and the extent of involvement of each lobe can significantly increase. The “crazy paving” pattern and the reverse halo sign have been seen.
The importance of atypical CT findings on chest CT in mildly symptomatic patients with COVID-19 has been investigated in a recently published article. The CT findings of COVID-19 pneumonia were described as being typical versus atypical:
1) Typical thoracic CT findings: Bilateral and multifocal ground-glass opacities, “crazy paving” appearance, consolidation (multiple foci with irregular contours, generally located peripherally in the lower lobe), peribronchovascular thickening, air bronchogram, halo sign, reverse halo sign, air bubble sign, subpleural and parenchymal bands in the lungs.
2) Atypical thoracic CT findings: Central involvement, isolated upper lobe involvement, solitary involvement, peribronchovascular involvement, lobar consolidation, tree-in-bud pattern, nodules, pleural effusion, pericardial effusion, subpleural sparing, white lung (diffuse infiltration involving the lung).
CT sensitivity was higher when atypical COVID-19 CT findings were included compared with interpreting typical findings alone. This result suggested that the absence of typical COVID-19 findings should not exclude COVID-19. The fact that patients with atypical CT findings have a higher 30-day mortality rate also supports this argument. The study showed that any new CT abnormalities, whether typical or atypical, should be considered in favor of COVID-19 pneumonia in a patient presenting with mild COVID-19 symptoms.
CT has a relatively high false-positive rate but in patients with acute cardiorespiratory presentations unremarkable CT scans and negative reverse transcriptase–polymerase chain reaction (RT-PCR) test results are likely to be reassuring. It is highly recommended to use a combination of different diagnostic tools to achieve appropriate sensitivity and specificity.
Simultaneous observation of ground-glass opacities and other features of viral pneumonia on a CT scan is optimal to detect COVID-19. However, it is suggested to make the final diagnosis based on both CT scan and RT-PCR test results, as none of those diagnostic modalities is reliable alone.
Imaging also has a role in monitoring treatment response in worsening COVID-19 and in evaluating new treatments such as whole lung irradiation as well as anticoagulation in case of pulmonary embolism.
Tables and FiguresTop
|
CT characteristics |
Bernheim et al |
Tabatabaei et al |
|
GGO |
34% |
88% |
|
Consolidation |
2% |
54% |
|
GGO or consolidation |
78% |
– |
|
GGO + consolidation |
41% |
– |
|
No GGO, no consolidation |
22% |
– |
|
Bronchial wall thickening |
12% |
– |
|
COVID-19, coronavirus disease 2019; CT, computed tomography; GGO, ground-glass opacity. | ||
|
Adapted from Radiology. 2020 Feb 20:200463 and Radiol Cardiothorac Imaging. doi: 10.1148/ryct.2020200130. | ||
|
CT characteristics of opacities |
Bernheim et al |
Tabatabaei et al |
|
Rounded |
54% |
26% |
|
Linear |
7% |
25% |
|
Crazy paving |
5% |
15% |
|
Reverse halo |
2% |
10% |
|
Peripheral distribution |
52% |
– |
|
No axial lung distribution |
48% |
– |
|
COVID-19, coronavirus disease 2019; CT, computed tomography. | ||
|
Adapted from Radiology. 2020 Feb 20:200463 and Radiol Cardiothorac Imaging. doi: 10.1148/ryct.2020200130. | ||
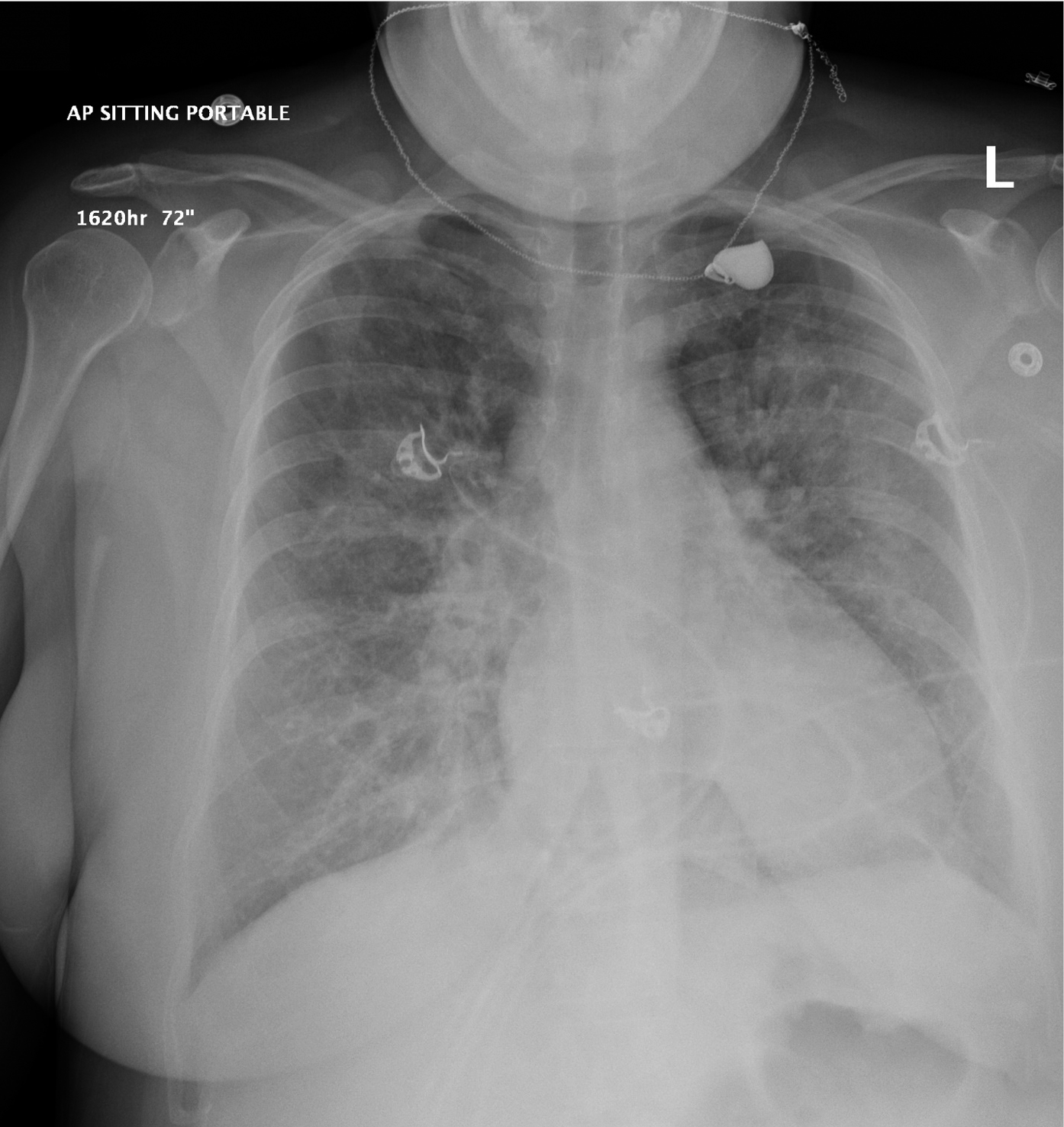
Figure 20.1-1. Anteroposterior (AP) chest radiography. A 35-year-old female patient (case #1) with chest pain. Diffuse patchy opacities in both lungs.
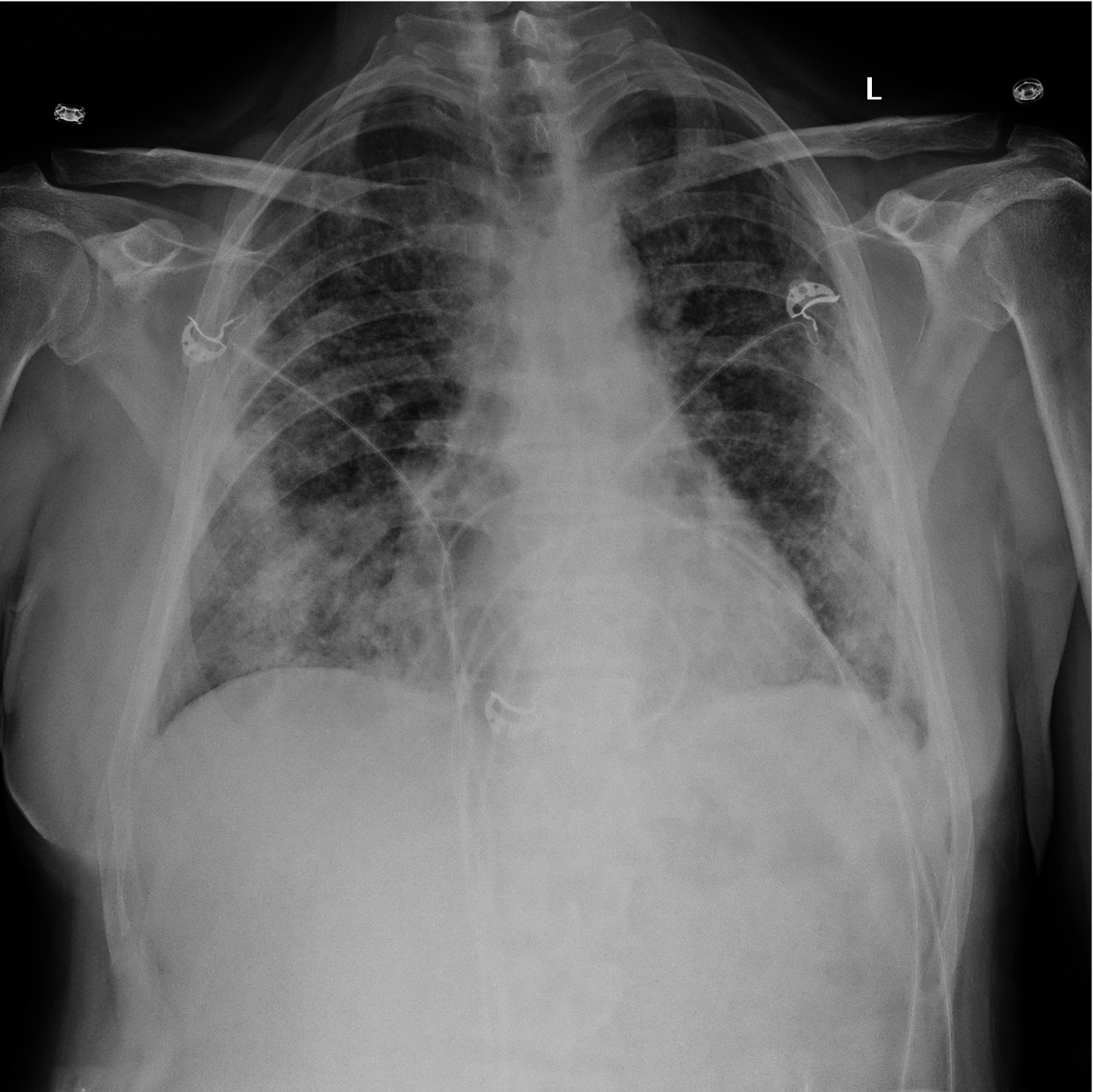
Figure 20.1-2. Anteroposterior (AP) chest radiography. A 65-year-old male patient (case #2) with cough and fever. Diffuse patchy opacities in both lungs, predominantly within the lower lobes and peripherally.
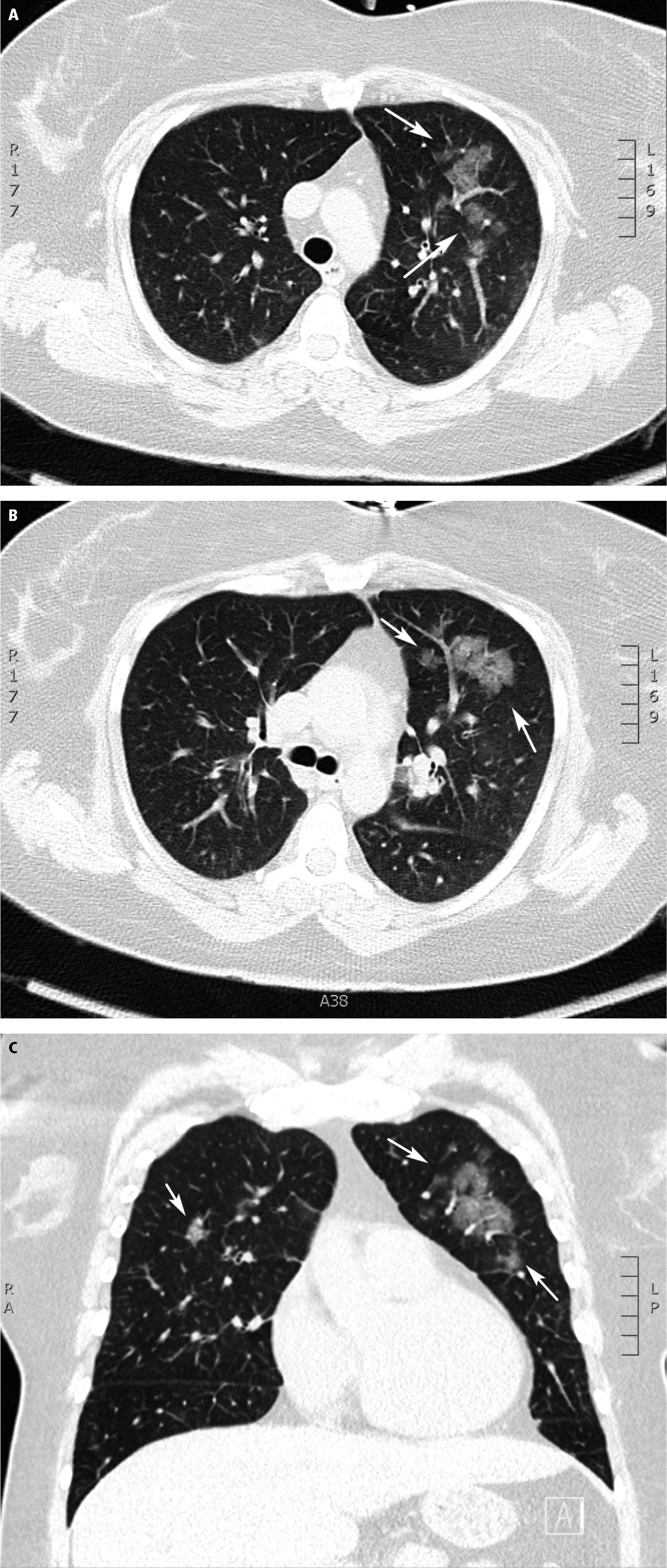
Figure 20.1-3. Computed tomography (CT) of a 35-year-old female patient (case #1) shows rounded ground-glass opacities (arrows) in axial (A, B) and coronal (C) planes.
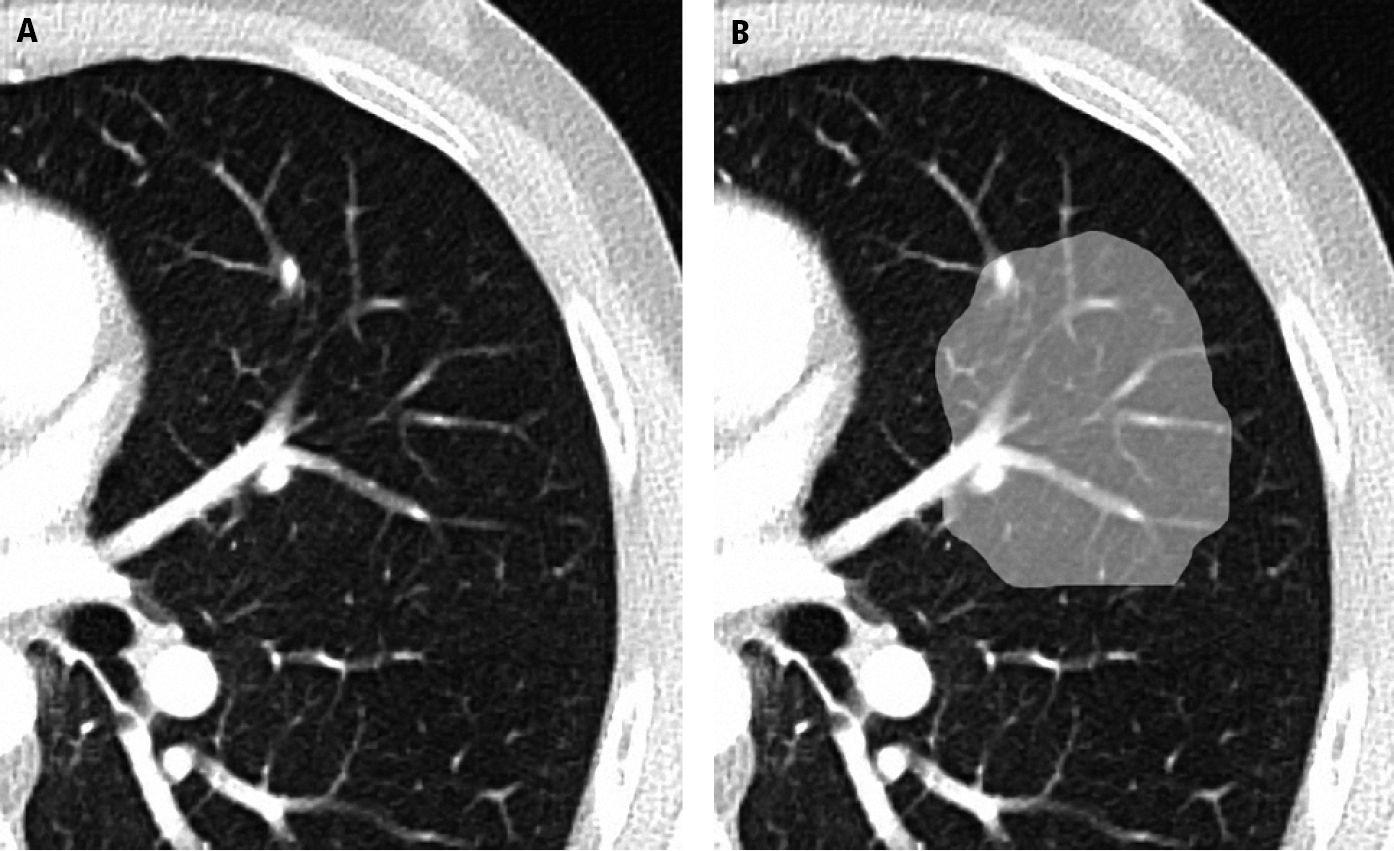
Figure 20.1-4. Axial computed tomography (CT) of the thorax showing a normal lung (A) and ground-glass opacity (B). Note that normal lung structures remain visible despite the opacity. Figure manipulated to enhance learning points using image editing software.
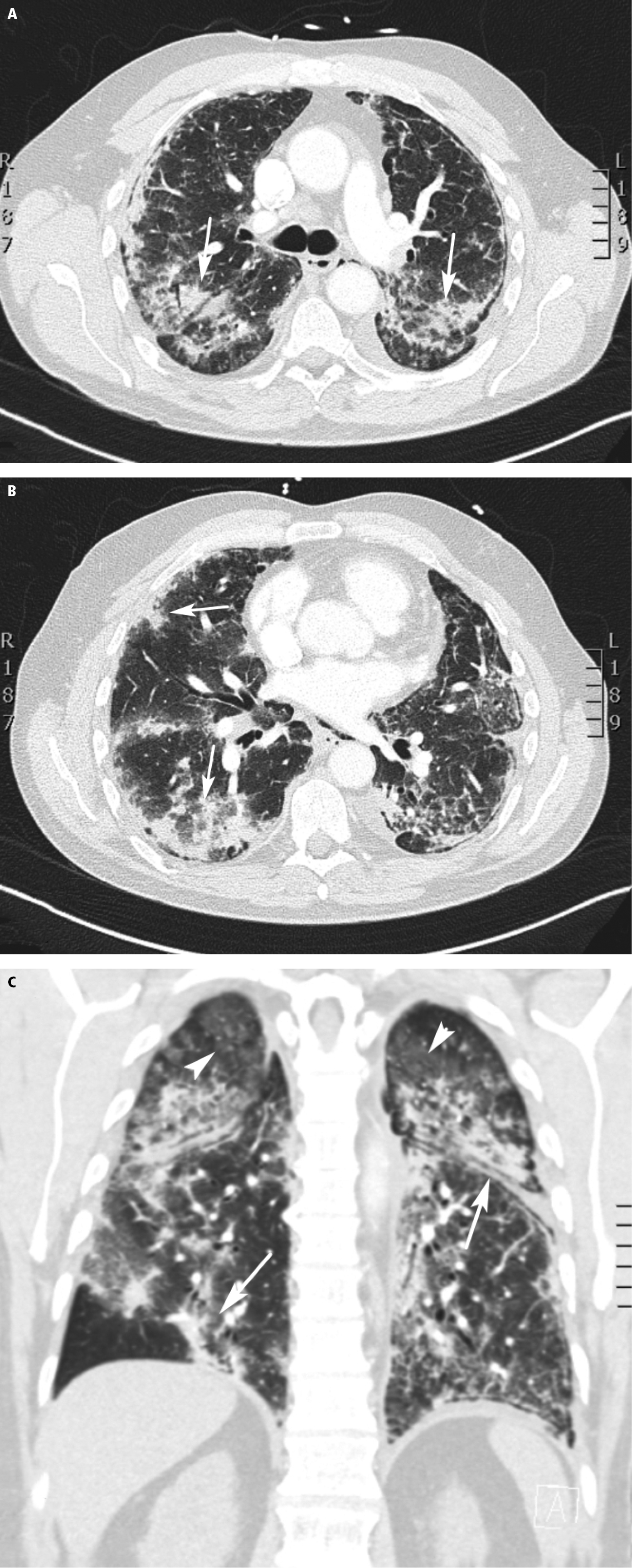
Figure 20.1-5. Computed tomography (CT) of a 65-year-old male patient (case #2) shows areas of consolidation (arrows) in axial (A, B) and coronal (C) planes. Rounded ground-glass opacities (arrowhead) and consolidation (arrows) are visible.
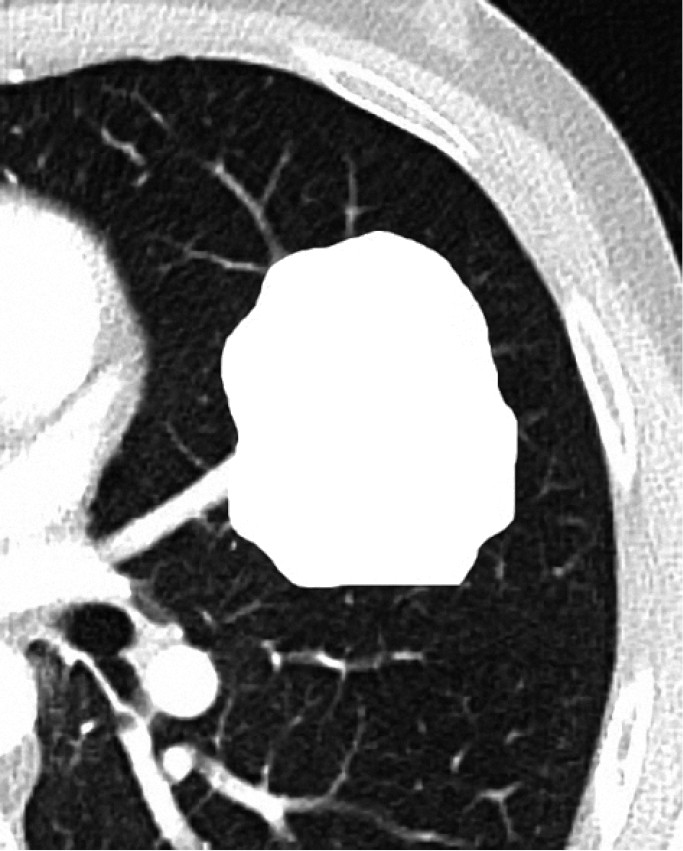
Figure 20.1-6. Axial computed tomography (CT) of the thorax showing lung consolidation (consolidated lung). Note that normal lung structures are not visible as distinct separate structures. Figure manipulated to enhance learning points using image editing software.

Figure 20.1-7. Coronal computed tomography (CT) of a 35-year-old patient (case #1) shows thickened bronchi (arrows).

Figure 20.1-8. The reverse halo sign. Figure manipulated to enhance learning points using image editing software.
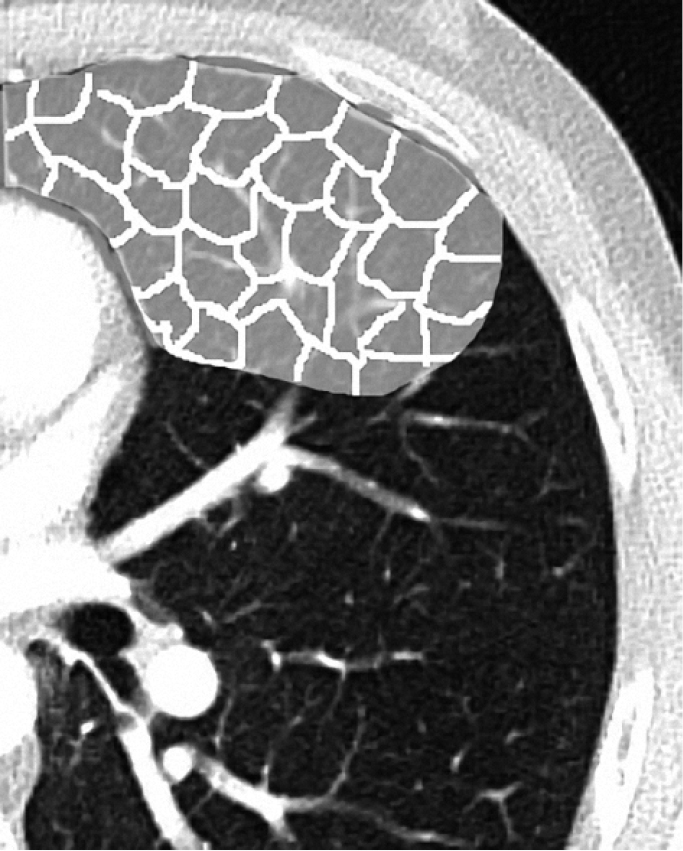
Figure 20.1-9. The “crazy paving” pattern. Figure manipulated to enhance learning points using image editing software.