Study Description and Recorded ParametersTop
1. Exercise stress testing may cause complications and is therefore performed in the presence of a physician in a room equipped with advanced cardiac life support (ACLS) equipment.
2. Electrode placement:
1) Precordial leads V1 to V6 as in standard electrocardiography (ECG) study (see Standard Electrocardiography).
2) Limb leads:
a) Left arm: Left subclavian fossa, medial to the deltoid muscle attachment.
b) Right arm: Right subclavian fossa, medial to the deltoid muscle attachment.
c) Left leg: In the left anterior axillary line, halfway between the lowest rib and the iliac spine.
d) Right leg: Below the lowest right rib.
3. Parameters monitored during exercise stress testing:
1) ECG is monitored continuously. It is recorded every 1 minute and then at 1, 3, 6, and 9 minutes during recovery.
2) Blood pressure (BP) is measured every 3 minutes during exercise and recovery.
4. Stress testing protocol:
1) Cycle ergometer: Start at 50 W, or at 25 W in patients with known coronary artery disease or reduced physical capacity. Increase the load by 25 W every 3 minutes.
2) Treadmill: There are many stress testing protocols using various belt speeds and grades. The most frequently used one is the Bruce protocol (Table 20.2-1). In the elderly and in patients with heart failure or hypertension, a modified protocol is indicated (with smaller load increments every 1-2 min), allowing the exercise duration to be extended to 8 to 12 minutes. A short warm-up before the test is necessary.
The stress load may be increased up to a point when the maximum heart rate is achieved (~220 minus age), when the patient develops signs and symptoms warranting termination of the test (symptom-limited exercise stress test), or until 85% to 90% of the maximum heart rate is achieved (submaximal stress test).
Absolute indications for terminating an exercise stress test before reaching the target heart rate include the patient’s request (in all cases), decrease in systolic blood pressure (SBP) by >10 mm Hg compared with baseline accompanied by other signs and symptoms of ischemia (chest pain regardless of severity, ST-segment depression indicating a positive or equivocal stress test result), angina, dizziness, presyncope, cyanosis or pallor, sustained ventricular tachycardia, second-degree or third-degree atrioventricular (AV) block, ST-segment elevation in leads with no abnormal Q waves or QS complexes present (except for leads V1, aVL, and aVR), or problems with ECG or BP monitoring.
Relative indications for terminating an exercise stress test include an SBP decrease by >10 mm Hg compared with baseline with no other signs and symptoms of ischemia, SBP >250 mm Hg, diastolic blood pressure (DBP) >115 mm Hg, escalating chest pain (not typical for angina), ST-segment depression >2 mm, multiform premature ventricular contractions, nonsustained ventricular tachycardia, supraventricular tachycardia, bradyarrhythmia, and bundle branch block difficult to distinguish from ventricular tachycardia.
ContraindicationsTop
1. Absolute contraindications: Acute myocardial infarction (within 2 days), unstable coronary artery disease not controlled by medical therapy, symptomatic arrhythmia, severe symptomatic aortic stenosis, decompensated heart failure, recent pulmonary embolism or pulmonary infarction, acute endocarditis, acute pericarditis, acute myocarditis, acute aortic dissection, insufficient physical capacity to perform an exercise stress test.
2. Relative contraindications: Left main coronary artery stenosis, moderate or severe aortic stenosis with symptoms of unconfirmed association with the stenosis, hypertrophic cardiomyopathy with a high resting pressure gradient, systolic or diastolic hypertension (BP ≥200/110 mm Hg), tachyarrhythmia, bradyarrhythmia, acquired high-degree AV block, recent stroke or transient ischemic attack, electrolyte disturbances, severe anemia, thyrotoxicosis.
Patient PreparationTop
1. Instruct the patient not to eat or smoke 3 hours prior to the test and to avoid strenuous exercise 12 hours prior to the test.
2. When possible, discontinue drugs that may interfere with interpretation of the test results (particularly beta-blockers) if the test is performed to confirm or exclude ischemic heart disease. Testing to assess prognosis in patients with known coronary artery disease is performed without drug discontinuation.
3. Take a history and perform physical examination and standard ECG to make sure there are no contraindications to the exercise stress test.
Result InterpretationTop
1. Criteria for a positive exercise stress test result (measurement of ST-segment deviations: Figure 20.2-1):
1) Horizontal or downsloping ST-segment depressions ≥1 mm.
2) ST-segment elevations ≥1 mm in leads with no abnormal Q waves or QS complexes present (except for leads V1, aVL, and aVR). ST-segment elevations in leads with abnormal Q waves present due to prior myocardial infarction may reflect abnormal left ventricular wall motion or reversible ischemia in the peri-infarct zone.
Equivocal exercise stress test results: Upsloping ST-segment depressions ≥1 mm within 60 to 80 milliseconds of the J point.
In patients with ST-segment depressions present at baseline, the depressions seen on the ECG recorded during the exercise stress test are to be assessed relative to the baseline ST segment, not the PR segment. In patients with ST-segment elevations present at baseline, the reference point is the PR segment, not the baseline ST-segment shift.
Right bundle branch block does not affect the interpretation of an ECG stress test except for leads V1 to V3 (ST-segment depression in these leads is of no diagnostic value). However, it is not possible to establish a reliable interpretation of exercise stress test results in the presence of left bundle branch block or preexcitation.
2. Causes of false-positive or false-negative exercise stress test results compared with coronary angiography for reference:
1) False positive: Myocardial ischemia caused by factors other than coronary artery stenosis, mitral valve prolapse, anemia, hypothyroidism, digitalis treatment, hypokalemia, resting ST-segment abnormalities of various etiology.
2) False negative: Insufficient exercise load, single vessel disease, left anterior fascicular block, right ventricular hypertrophy, drugs (eg, beta-blockers, phenothiazines).
ComplicationsTop
Hypotension, syncope, arrhythmia, heart failure, acute coronary syndrome. All these complications may occur during exercise stress testing or recovery.
TABLES AND FIGURESTop
|
Stage |
Belt speed (km/h) |
Grade (%) |
Time (min) |
Stage (MET) |
|
1 |
2.7 |
10 |
3 |
5 |
|
2 |
4.0 |
12 |
3 |
7 |
|
3 |
5.5 |
14 |
3 |
10 |
|
4 |
6.8 |
16 |
3 |
13 |
|
5 |
8.0 |
18 |
3 |
15 |
|
1 MET = resting oxygen consumption of 3.5 mL/kg/min. |
||||
|
MET, metabolic equivalent of task. |
||||
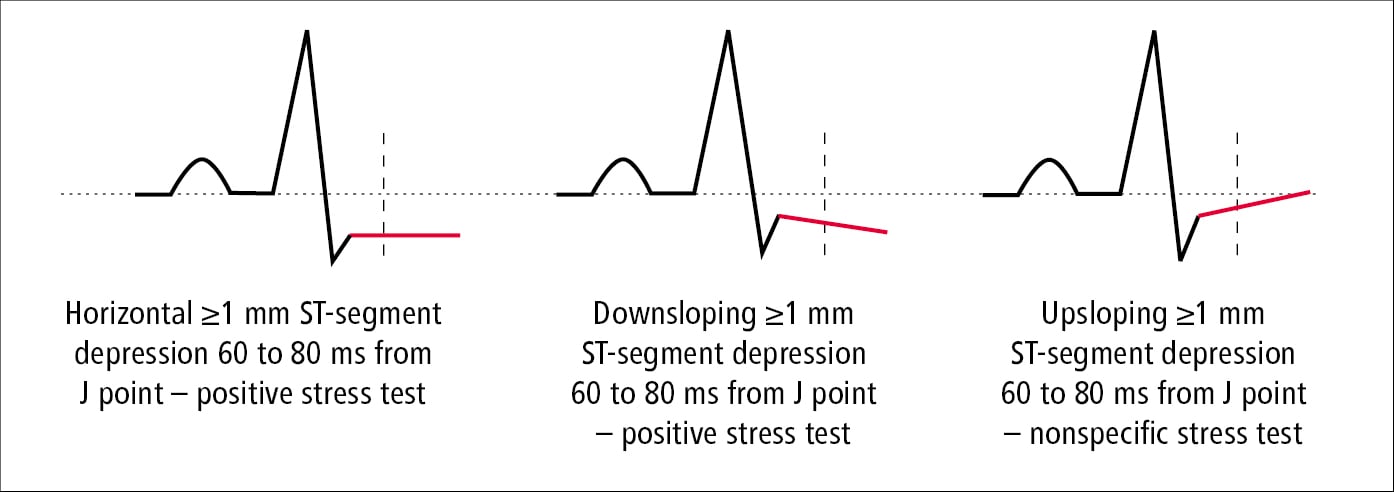
Figure 20.2-1. Measurements of ST-segment depression in an electrocardiographic (ECG) stress test.