Bickley LS, Szilagyi PG, Hoffman RM, Soriano RP. Bates’ Guide to Physical Examination and History-Taking. 13th ed. Wolters Kluwer Health; 2023.
Libby P, Bonow RO, Mann DL, et al; eds. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Elsevier; 2021.
Simel DL, Rennie D, Keitz SA. The Rational Clinical Examination: Evidence-Based Clinical Diagnosis. McGraw-Hill; 2009.
Walker HK, Hall WD, Hurst JW. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Butterworths; 1990.
There are 4 main areas of auscultation: Figure 1.18-1. Their central points are:
1) The fifth left intercostal space medial to the midclavicular line (apex): Mitral valve area (M).
2) The fourth and fifth intercostal spaces near the lower sternal border: Tricuspid valve area (T).
3) The second left intercostal space near the upper sternal border: Pulmonary valve area (P).
4) The second right intercostal space near the upper sternal border: Aortic valve area (A).
Place the patient in a supine position and auscultate the heart. Instruct the patient to breathe steadily. When necessary, ask the patient to stop breathing on inspiration or expiration or to change their body position. Right-sided murmurs are usually louder on inspiration due to increased venous return from negative intrathoracic pressure created by inspiration. Palpate the carotid or radial pulse simultaneously to orient your auscultation to the first heart sound (S1; occurs before pulse upstroke) and the second heart sound (S2; occurs after upstroke).
FiguresTop
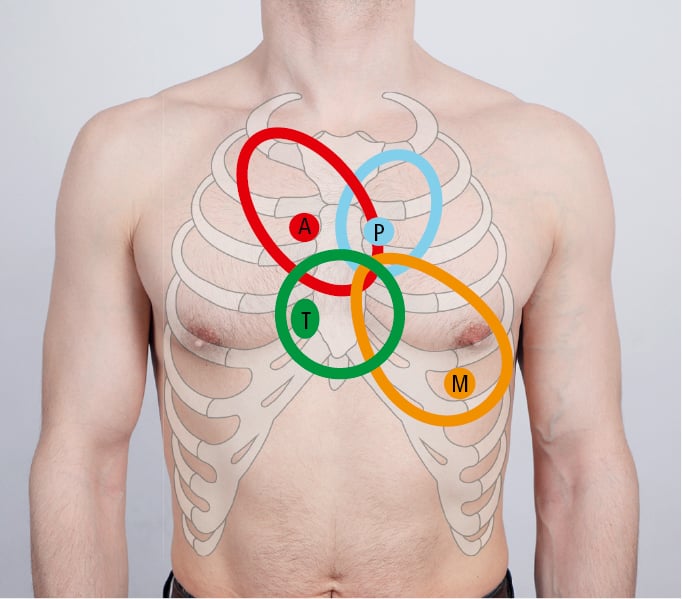
Figure 1.18-1. Areas of auscultation of the heart.