Definition, Etiology, PathogenesisTop
Jaundice (icterus) is yellow or yellowish coloration of the sclera, mucous membranes, and skin caused by the accumulation of bilirubin in tissues.
Jaundice becomes visible at bilirubin levels >43 micromol/L (~2.5 mg/dL), first in the sclera, then on the skin. It resolves in the reverse order. Bilirubin, an end product of heme metabolism, is conjugated in the liver, excreted in the biliary tree, and stored in the gallbladder. Excess heme degradation, disruption to bile flow, or disruption of any step in the bile metabolism may result in hyperbilirubinemia (predominantly unconjugated or conjugated hyperbilirubinemia, depending on etiology) and clinically manifest as jaundice.
Classification based on etiology:
1) Predominately unconjugated (indirect) hyperbilirubinemia is usually due to excess hemoglobin destruction or its compromised stability and survival. Specific causes:
a) Extravascular or intravascular hemolysis: Congenital hemolytic anemia, immune hemolytic anemia, erythrocyte damage (artificial heart valves, march hemoglobinuria, thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, disseminated intravascular coagulation, sickle cell anemia), infection (sepsis, malaria, toxoplasmosis), severe burns, hypersplenism, and paroxysmal nocturnal hemoglobinuria.
b) Impaired conjugation of bilirubin with glucuronic acid: Gilbert syndrome or Crigler-Najjar syndrome.
2) Predominately conjugated (direct) hyperbilirubinemia or mixed hyperbilirubinemia is usually due to cholestasis (obstructive jaundice), destruction of hepatocytes, or both:
a) Intrahepatic cholestasis: Primary biliary cholangitis, hepatotoxicity (acute alcoholic hepatitis, biologic toxins [fungi, plant alkaloids] or inorganic toxins [carbon tetrachloride, alcohol]), malignancy (lymphoma, liver tumors), sepsis, viral hepatitis, viral infection without inflammation and with extensive necrosis of hepatocytes (yellow fever, dengue, and other hemorrhagic fevers), bacterial infections (leptospirosis, secondary and congenital syphilis), infiltrative diseases (sarcoidosis and amyloidosis), inherited disorders (Dubin-Johnson syndrome, Rotor syndrome), chronic liver disease of any etiology, and liver disease associated with pregnancy.
b) Extrahepatic cholestasis: Choledocholithiasis, malignancy (pancreatic cancer, lymphoma, cholangiocarcinoma, extrinsic compression from other malignancies), sclerosing cholangitis, HIV cholangiopathy, infection (parasitic).
DiagnosisTop
Take a history and perform physical examination. Jaundice is often associated with pruritis, dark urine, and pale stool, all of which are nonspecific. Clinicians should seek information regarding liver toxicity or injury secondary to prescribed medications and over-the-counter (herbal) supplements. It is also important to assess for viral hepatitis risk factors (IV drug use, unscreened blood transfusions, needlestick injuries, consumption of contaminated food and water, poor sanitation, high-risk sexual activity, HIV status), occupation, travel history, family history of liver disease or hemoglobinopathies, previous intraabdominal surgeries, and history of chronic liver disease. In addition, jaundice should be evaluated in the context of other presenting clinical signs and symptoms including sepsis and malignancy (eg, weight loss, night sweats).
The Courvoisier sign (a palpable nontender gallbladder in patients presenting with jaundice) may be a sign of underlying malignancy. Jaundice in the context of end-stage liver disease/cirrhosis (eg, ascites, splenomegaly, spider angiomas, nail clubbing) may be suggestive of acute-on-chronic decompensation of liver disease. Infection should be strongly considered in patients who present with signs of sepsis (possibly with right upper quadrant abdominal pain).
Differential diagnosis of jaundice: Figure 1.24-1. In the differential diagnosis of yellowish coloration of the skin, consider excess beta-carotene in the skin (carotenemia) associated with excessive intake of preparations containing carotene or drinking large amounts of carrot juice.
FiguresTop
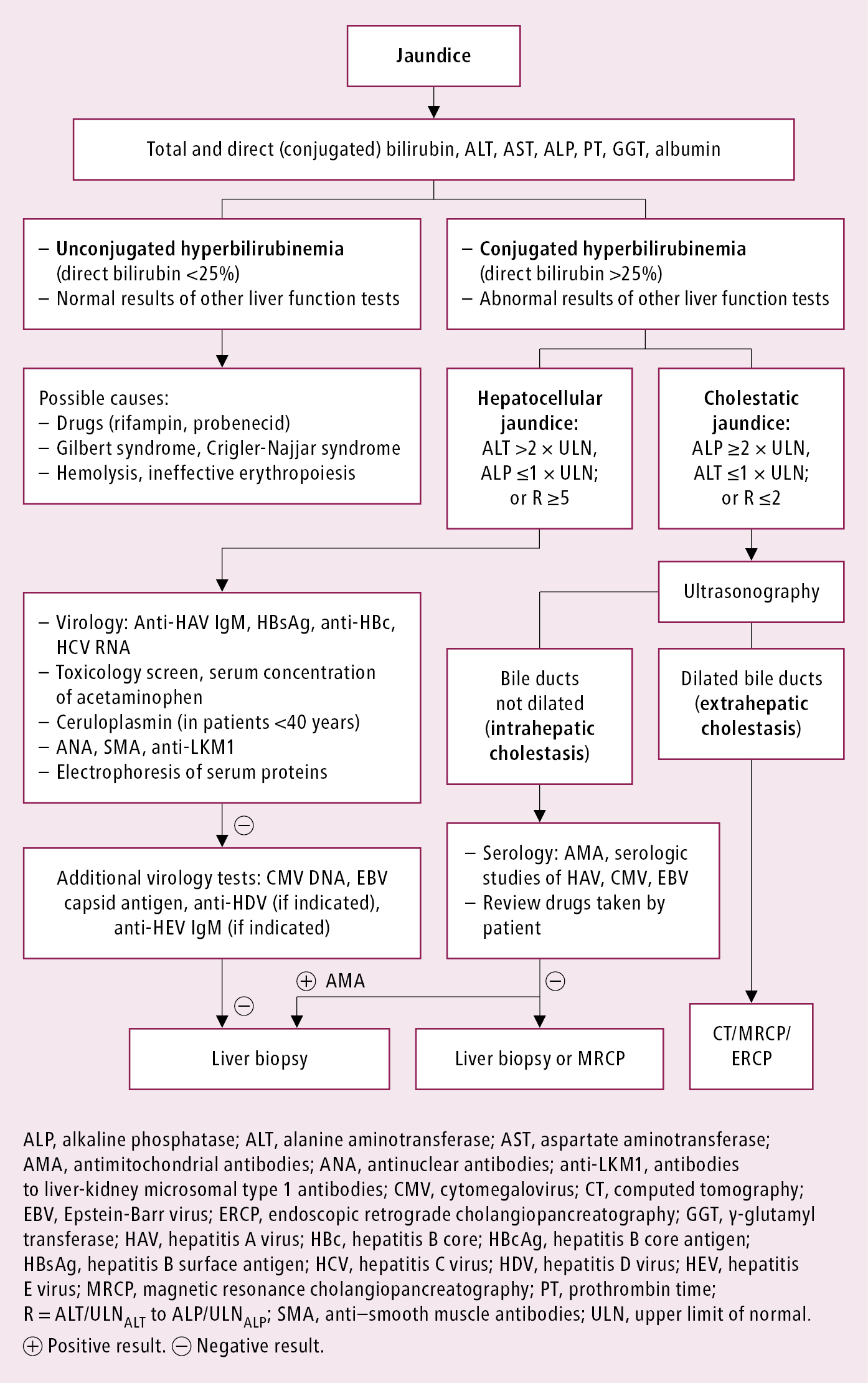
Figure 1.24-1. Diagnostic algorithm of jaundice.