Causes and PathogenesisTop
Sensory disturbances may present as reduced sensation (eg, impairment of ≥1 type of sensory perception), positive symptoms (eg, abnormal sensory perception in the form of paresthesias [pins and needles] or hypersensitivity to sensory stimuli [hyperesthesia, allodynia (pain due to a stimulus that usually does not provoke pain), and/or pain]), or both.
Causes: Conditions that damage peripheral receptors located in various tissues and organs, sensory fibers in peripheral nerves, ascending tracts in the spinal cord and brainstem, sensory nuclei in the brainstem and thalamus, and cortical centers in the parietal lobe.
Sensory disturbances can occur in isolation but can also be associated with motor weakness or other neurologic signs that help identify the location of the disturbance (eg, lower motor neuron signs, such as hypotonia and loss of reflexes, suggest a peripheral nerve dysfunction; see Muscular Weakness (Paresis and Paralysis)). The presence of pain typically suggests pathology of a peripheral nerve, plexus, nerve root, or dorsal horn ganglion. Brief and transient paresthesias are not suggestive of nervous system damage.
Patterns and causes of specific types of sensory symptoms based on the location of nervous system lesions: Table 1.38-1.
DiagnosisTop
1. History and physical examination: Determine the type and severity of sensory symptoms, distribution of sensory abnormalities, and circumstances in which they have occurred. The sense of touch is examined by touching the patient’s body with your finger or cotton swab. The sense of pain is examined with a sharp pin. The sense of temperature is examined with a cold object. The sense of vibration is examined with a 128 Hz tuning fork. The sense of position is examined by moving a joint. When examining for sensory abnormalities, compare the symmetric parts of the body, precisely determine the boundaries of sensory abnormalities, compare them with the areas of innervation by specific peripheral nerves and nerve roots (Figure 1.38-1), compare them with the patterns of sensory loss based on the location of the lesion (Table 1.38-1), and identify associated motor or pathognomonic signs (see Muscular Weakness (Paresis and Paralysis)).
2. Diagnostic studies: Imaging studies (computed tomography [CT], magnetic resonance imaging [MRI]) of the brain or spinal cord (or both) as well as electrophysiologic tests (sensory nerve conduction studies, somatosensory evoked potentials), depending on the suspected location of the lesion.
Tables and FiguresTop
|
Lesion location |
Pattern of sensory disturbances |
Possible causes |
|
Peripheral nerve |
Pain and paresthesia in area innervated by affected nerve followed by sensory loss involving all sensory functions |
Mononeuropathy (compression, injury) |
|
Nerve root |
Pain worsened by activities increasing intraspinal pressure (eg, cough, defecation), paresthesia within areas innervated by respective nerve roots followed by sensory loss involving all sensory functions |
Radiculopathy (disc herniation, acute inflammatory demyelinating polyradiculopathy, severe degenerative lesions of spine, tumor) |
|
Spinal cord lesion |
– Sensory loss below lesion level – Hemicord syndrome: ipsilateral loss of vibration and position sense with contralateral loss of pain and temperature sense |
Trauma, tumor, demyelination, infection, ischemia or hemorrhage, of spinal cord |
|
Anterior spinal artery syndrome |
Sensory loss below lesion level, dissociated sensory loss: loss of pain and temperature with preserved vibration and position sense (with paralysis) |
Anterior spinal artery thrombosis |
|
Posterior columns of spinal cord |
Loss of vibration and position sense with preserved pain and temperature (with loss of reflexes) |
Subacute combined degeneration of spinal cord (in vitamin B12 deficiency), tabes dorsalis (neurosyphilis) |
|
Trigeminal nerve or nucleus |
Sensory loss in face in distribution of the trigeminal nerve or branches |
Inflammation, demyelination, tumor |
|
Thalamus or posterior limb of internal capsule |
Sensory loss of pain and temperature on contralateral side of face, arm, and leg, including trunk; chronic thalamic pain syndrome may occur later |
Ischemic or hemorrhagic stroke, tumor, demyelination |
|
Parietal cortex |
Inability to assess stimulus intensity and location, impaired graphesthesia (ability to recognize letters or numbers traced on skin), loss of 2-point discrimination (ability to recognize 2 simultaneously applied stimuli as separate), extinction (inability to recognize 1 of 2 simultaneously applied tactile stimuli on symmetric body regions), astereognosis (inability to recognize objects held in hand without visual inspection) |
Ischemic or hemorrhagic stroke, tumor |
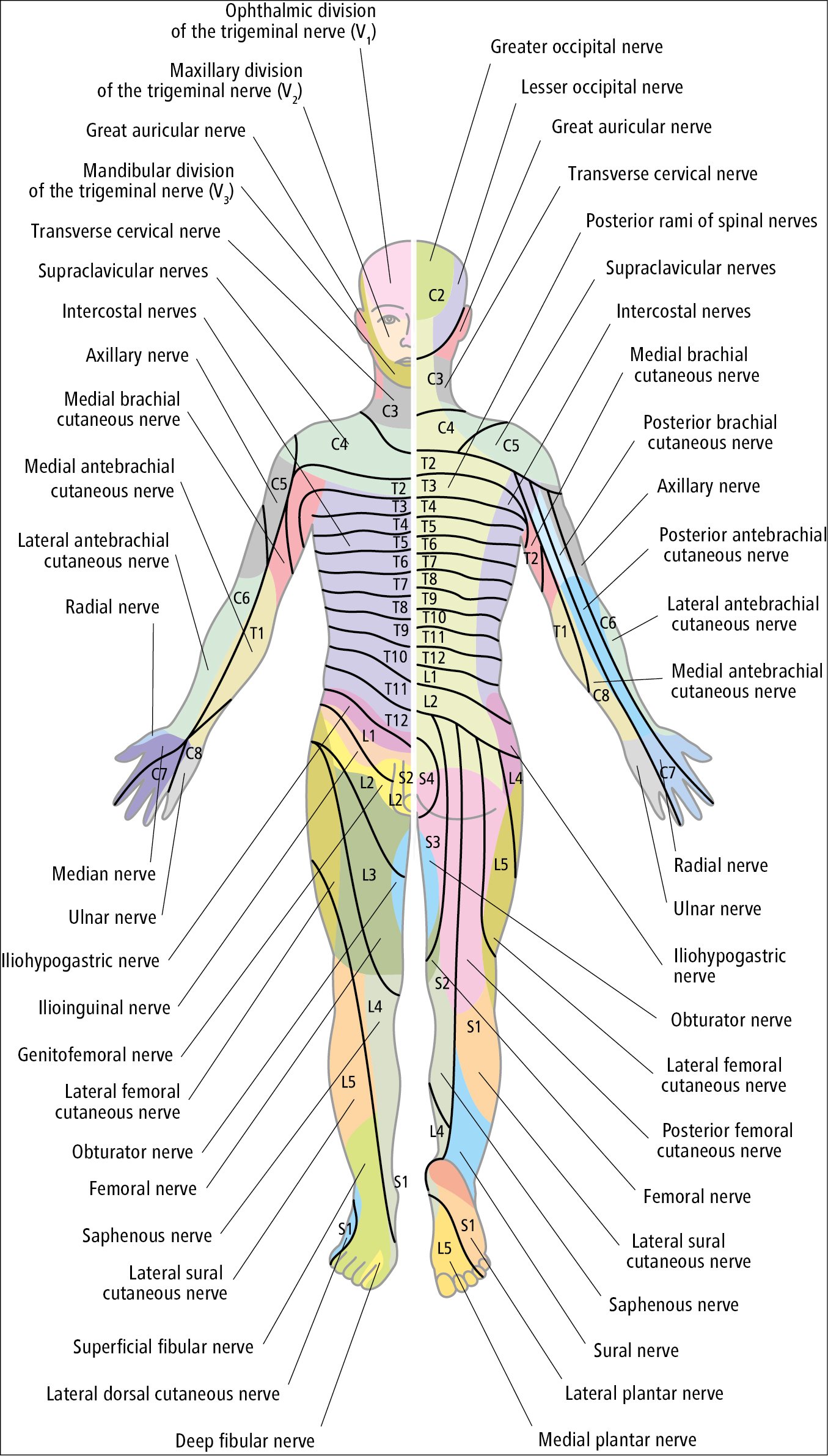
Figure 1.38-1. Cutaneous fields of peripheral nerves and dermatomal map of nerve root innervation of the skin.