Etiology and PathogenesisTop
1. Etiologic agent: Human papillomavirus (HPV) is a nonenveloped, double-stranded DNA virus. More than 200 types of HPV exist.
2. Pathogenesis: HPV infects basal epidermal and squamous epithelial cells. As the infected cells mature and differentiate, replication increases and the cells undergo a transformation leading to the development of exophytic lesions, which are the clinical manifestations of HPV infection. Most HPV infections resolve spontaneously within 1 to 2 years, either representing true “viral clearance” or immune control to below-detectable levels, known as viral latency. Cellular immunodeficiency disorders (eg, HIV, treatment with immunosuppressive agents) are associated with increased HPV replication, persistent HPV infection, as well as poor response to treatment and possibly increased risk of malignancy with high-risk HPV types.
As individual subtypes of HPV show predilection for certain locations, the lesions are categorized into cutaneous HPV infections (most of them known as cutaneous warts) and mucosal HPV infections, including anogenital, oral, and oropharyngeal HPV infection.
Certain types of HPV are designated low-risk types and are responsible for common cutaneous and genital warts. Other, known as high-risk types, integrate into the human DNA and result in neoplastic transformation of the affected cells. These high-risk types, predominantly type 16 (50% of patients) and type 18 (20%), are recognized as the underlying etiologic agents for many cancers, including cervical cancer. Other cancers associated with high-risk type HPV infection include penile, vulvar, vaginal, anal, and head and neck cancers (squamous cell carcinomas of the oral cavity, pharynx, larynx, and paranasal sinuses).
3. Reservoir and transmission: The reservoir of HPV is the infected individual. Viral transmission occurs by sexual contact (in genital HPV infection), by direct contact with cutaneous or mucosal lesions, or rarely vertically, during delivery (low risk of infection).
4. Incubation period: The incubation period is usually 2 to 3 months, but it could range from a few weeks to a few years.
Clinical FeaturesTop
Clinical manifestations of HPV depend on many factors including the genotype, anatomic site of involvement, and immune status of the affected person.
Cutaneous HPV infection can have different presentations, like common warts (also known as verruca vulgaris; Figure 10.11-1), palmar or plantar warts (Figure 10.11-2, Figure 10.11-3), plane or flat warts, and anogenital warts (also known as condylomata acuminata; Figure 10.11-4). Other presentations include periungual warts (around nails) and filiform warts. A summary of mucosal HPV infections: Table 10.11-1.
Cervical dysplastic lesions are detected by pelvic examination, Papanicolaou testing, or biopsy. They are sometimes inconspicuous, flat, and difficult to distinguish from normal mucosa.
A particular form of extensive chronic HPV infection is epidermodysplasia verruciformis, a rare genetic disorder.
DiagnosisTop
Diagnosis of HPV infections is established on the basis of clinical features. If HPV-associated malignancy is suspected, cytologic and histologic examinations should be performed. HPV cannot be cultured or inoculated in animals.
Sexually active individuals with a cervix should be regularly screened for cervical cancer with an HPV DNA detection test, cytology (Papanicolaou test) followed by colposcopy in the case of abnormal microscopic findings (low-grade or high-grade intraepithelial dysplasia), or some combination of these tests. In individuals presenting with anogenital warts it is necessary to perform anoscopy.
Patients with HPV infection should be evaluated for other sexually transmitted infections: syphilis and gonorrhea, as well as HIV, hepatitis B virus (HBV), hepatitis C virus (HCV), and chlamydial infections.
Differential diagnosis for HPV infections is broad and includes molluscum contagiosum, skin tags, benign melanocytic nevi, adnexal tumors, seborrheic keratosis, and condylomata lata of secondary syphilis.
TreatmentTop
Possible treatment options: Table 10.11-2.
There are no known commercially available antiviral agents active against HPV. Surgical excision should be avoided; however, large warts can be sometimes surgically removed with wide local excision if they are not responding to other conventional treatment measures. If the patient is suspected to have HPV-related skin or urogenital malignancy (penile, vulvar, cervical, anal), they should be referred to specialists (gynecologist, urologist, dermatologist, oncologist). Local guidelines for the management of individuals with positive HPV DNA test results or cytologic abnormalities should be followed.
ComplicationsTop
Complications are mostly related to the anatomic location and type of HPV. Cutaneous warts can have impact on social life due to cosmetic appearance. Common warts on hands or around nails can be painful. Plantar warts, when large or deep, can cause significant pain upon standing or walking and can affect ambulation.
Genital condylomata acuminata, especially when extensive, can result in depression, anxiety, sexual abstinence, and even anxiety-related sexual dysfunction. Rarely, condylomata acuminata in the urethra may cause urinary obstruction. Although rare, the presence of genital condylomata acuminata during pregnancy delivery may cause laryngeal papillomatosis in the newborn.
Untreated laryngeal, pharyngeal, and respiratory warts can lead to airway obstruction or hoarseness.
High-risk HPV types (16, 18, and other) can cause neoplastic transformation, resulting in penile, cervical, anal, vulvar, vaginal, and oropharyngeal cancers.
PrognosisTop
In immunocompetent patients with common nonneoplastic HPV lesions, the prognosis is good. In patients with HPV-related malignancies, the prognosis depends on the stage of the disease at presentation and available treatment options.
PreventionTop
Vaccination: see Vaccines: Human Papillomavirus.
1. Patients should be educated about their conditions and HPV etiology.
2. Patients should be encouraged to use their own towels and tools (shaving machines). Personal tools used for cutting or paring down warts, like pumice stone or nail files, must not be shared. Patients with warts in hair-bearing areas (beard, pubic area) should avoid shaving with razors to reduce the chance of spreading. Patients should not scratch or touch their HPV warts, as this may facilitate spreading. Those with plantar warts should wear appropriate footwear to reduce the chance of transmission.
3. Patients with genital condyloma acuminata should inform their sexual partners that they are at risk of acquiring HPV virus.
4. Health care providers are encouraged to wear proper face protective equipment (eg, masks and face shields) during invasive procedures that can generate aerosols.
Tables and FiguresTop
|
HPV infection |
Characteristics |
|
Anogenital warts (condylomata acuminata) |
– Most common STD in the world – Biggest risk factor is unprotected sex – Present as cauliflower-like lesions on penis, scrotum, vulva, anal and perianal area, pubic, groin – Most commonly caused by low-risk HPV types 6 and 11 |
|
HPV-related anogenital intraepithelial neoplasia and cancers |
– Most commonly caused by high-risk HPV types 16 (50%) and 18, less commonly by types 31, 33, 35 – Can cause bowenoid papulosis; erythroplasia of Queyrat (squamous cell carcinoma in situ of penis skin); and cervical, anal, vulvar, and vaginal cancers |
| Recurrent respiratory papillomatosis |
– Rare condition characterized by recurrent small papillomas in respiratory tract – Most commonly caused by low-risk HPV types 6 and 11 – Most frequently affects larynx but can affect trachea, bronchia, and even lung parenchyma – No cure available; treatment goal is usually to prevent airway obstruction |
|
Focal epithelial hyperplasia (Heck disease) |
– HPV infection of oral mucosa – Most commonly caused by HPV types 13 and 32 – Usually presents as white flat or slightly raised papules on lips, buccal mucosa, or tongue |
|
Conjunctival papilloma |
|
|
Giant condyloma acuminate (Buschke-Löwenstein tumor) |
– Caused by HPV types 6 and 11 – Presents as slowly growing, large, verrucous-appearing tumor in genital areas – Locally invasive |
|
HPV-related oropharyngeal cancer |
– Can be caused by HPV types 16 and 18 – Responsible for oropharyngeal cancer in patients without traditional risk factors associated with head and neck cancers (eg, smoking, alcohol consumption) |
|
HPV, human papillomavirus; STD, sexually transmitted disease. | |
|
Treatment |
Description |
|
Local physical destructive therapy |
– Cryotherapy with liquid nitrogen, electrocautery, and ablative lasers – Cryotherapy with liquid nitrogen is most commonly used for cutaneous and anogenital warts – Repeated sessions every 3-4 weeks required until lesions are fully resolved – Adverse effects include pain, urticarial reaction, blistering, ulceration, posttreatment hypopigmentation or depigmentation in treated areas |
|
Topical salicylic acid preparations |
– Available in different concentrations – Painless, for self-application, lacks adverse effects, can be used without prescription (OTC) – Usually used for cutaneous warts (treatment should last ≤12 weeks) |
|
Topical immunomodulators (imiquimod) |
– Imiquimod is a TLR 7 agonist enhancing immune response against HPV – Topical imiquimod available in Canada in 2 formulations: 5% (Aldara) once a day on 3 nonconsecutive days/wk for up to 16 weeks and 3.75% (Vyloma) once daily for up to 8 weeks – Approved for treatment of external anogenital warts |
|
Podophyllum resin–derived topical cytotoxic therapy |
– Used for treatment of external anogenital warts – Available as podophyllum resin (podophyllin) and podophyllotoxin – Podophyllum resin (podophyllin), marketed in Canada as Podofilm 25%, is applied in office by physician – Podophyllotoxin, marketed in Canada as Condyline, applied by patient bid for 3 consecutive days with 4 days off treatment for up to 4 weeks – Should not be used in pregnancy |
|
Trichloroacetic acid |
– Available in different concentrations; commonly used in 60%-90% concentrations – Can be used for cutaneous and anogenital warts – Treatment applied by physician, resulting in physical destruction of proteins within warts by chemical coagulation – Can cause severe chemical burns if used by inexperienced individuals |
|
Topical fluorouracil |
– Topical fluorouracil is an antimetabolite; topical formulations can be used off-label for cutaneous warts – Can be applied daily (or less frequently) under occlusion for up to 3 months – Usually associated with adverse effects in treated areas (eg, pain, severe irritation, erythema, edema, blistering, ulceration, dyspigmentation, deep scarring) – Should not be used in pregnancy |
|
Sinecatechins |
– Approved for treatment of external anogenital warts – Commercially available in Canada as Veregen – Botanical drug as a green tea extract – Mechanism of action not clear – Applied tid for up to 16 weeks |
|
Other (based on small cases series and case reports) |
– Topical and systemic cidofovir – Systemic and intralesional injection of IFN alpha and IFN beta – Immunotherapy with intralesional injection of Candida albicans antigen – Immunotherapy with intralesional injection of MMR vaccine – Immunotherapy with intralesional injection of Mycobacterium w or BCG vaccine – Oral cimetidine |
|
The provided trade (brand) names are valid for Canada. | |
|
BCG, bacille Calmette-Guérin; bid, 2 times a day; HPV, human papillomavirus; IFN, interferon; MMR, measles, mumps, and rubella; OTC, over the counter; tid, 3 times a day; TLR, toll-like receptor. | |

Figure 10.11-1. Human papillomavirus. Common warts on the dorsum of the hand.

Figure 10.11-2. Human papillomavirus. Palmar warts.
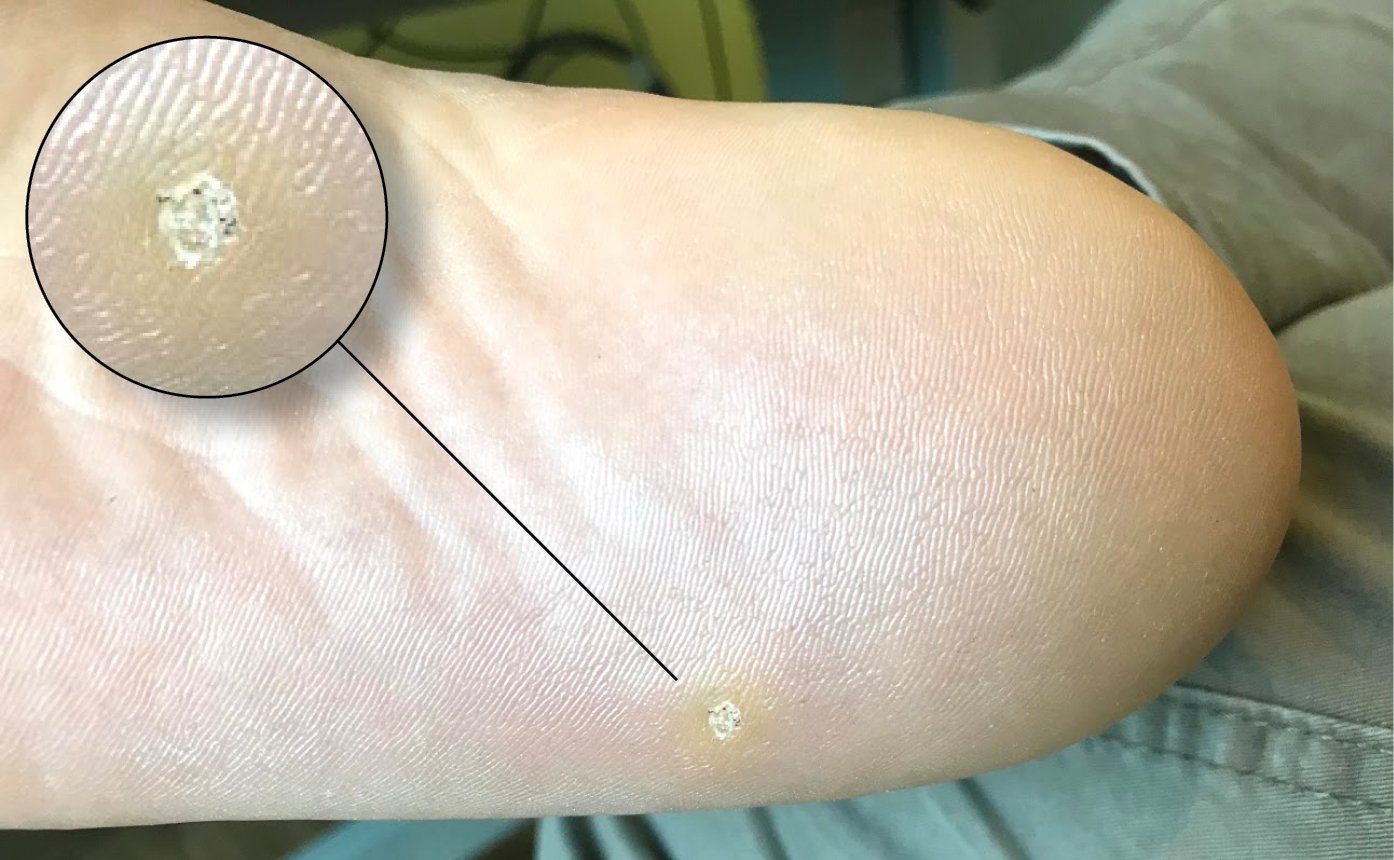
Figure 10.11-3. Human papillomavirus. Plantar wart. Black dots within the wart visible in the enlarged photo represent thrombosed capillaries seen in warts. This feature helps to differentiate plantar warts from plantar calluses.

Figure 10.11-4. Human papillomavirus. Genital warts, also known as condyloma acuminata.