Exposure to biologic agents is one of the primary occupational hazards in health care facilities. Preventive measures are selected based on the evaluation of occupational risk, which includes, among others, the class of harmful biologic materials; type, degree, and duration of exposure; and risk associated with the type of work performed.
Personal protective equipment (PPE) is a crucial component in the hierarchy of controls to protect health care providers (HCPs). Additional precautions are selected depending on the pathogen transmission routes and should be immediately taken if a transmissible infection is suspected.
Respiratory Protection (Masks)Top
Masks and respirators protect against infectious respiratory particles (IRPs) of various sizes, from very small (historically considered “aerosol” if diameter <5 microm) to larger particles and splashes.
Masks and respirators used in everyday practice are divided into several categories based on their filtering properties and shape (Figure 10.6-1). The most commonly used category is half-masks, which includes medical or surgical masks and respirators: N95 (European equivalent: filtering facepiece 2 [FFP2]) and N99 (European equivalent: FFP3). N99 respirators are rarely used in health care settings. The distinction between N95 and N99 and FFP2 and FFP3, respectively, is based on the filtering effectiveness and total inward leakage (the maximal proportion of particles that enter the mask due to incorrect adjustment and/or leaking of exhalation valves, if present). Full-face respirators are rarely used in health care settings and include reusable respirators with replaceable filters (Figure 10.6-2, panel C). These full-face respirators are more comfortable and can be used, for example, in the case of long exposure time or by an HCP with a beard, but they are more challenging for donning and doffing and must be decontaminated after each use.
The choice of PPE for specific medical procedures and settings as well as its maximum time of use depend on filtration features, additional properties influencing the permeability of the material, and shape of the mask. If a mask must be worn for a long time, it should be replaced with a new one when it becomes wet or when breathing becomes difficult. Nonmedical masks (made of fabric) are not considered an alternative to medical masks or worn by HCPs due to their lower level of protection.
Two-layer or 3-layer medical (or surgical) masks (half-masks) with ties or ear loops (Figure 10.6-1, panel A) can be subclassified into 3 subcategories based on their filtration activity and level of fluid resistance. These masks trap potentially infectious biologic materials on their outer surface and therefore protect the respiratory tract of a noninfected person from pathogens that may invade the mucosa. Medical masks protect primarily against pathogen-containing larger IRPs from gaining access into the oral and nasal mucosa. Although protection from smaller IRPs can be improved by choosing well-fitting medical masks (as the material itself has excellent filtration properties), fit-tested respirators are more protective against inhalation of these small respiratory particles and should be used for “airborne precautions,” while medical/surgical masks should be used to prevent what has been historically referred to as droplet infections. In addition, medical masks worn by individuals with respiratory infection can reduce the spread of IRPs and serve as source control. Therefore, patients infected with respiratory pathogens (via historic droplet or airborne routes) should wear such masks during contact with other persons and during transport.
Respirators (Figure 10.6-1, panel B, Figure 10.6-1, panel C, and Figure 10.6-1, panel D) are designed to snugly fit to the face and filter the entire inhaled air. While the European FFP2 and FFP3 do not need to be fit tested, the North American N95 respirators require regular fit testing.
Respirators with exhalation valves are particularly useful when the respirator must be worn for a long time. Valved respirators can be worn longer, as valves release a part of exhaled water vapor, and therefore less moisture accumulates under the respirator as compared with nonvalved respirators. However, valved respirators should not be used by individuals with suspected infection (contaminated air is exhaled unfiltered through the valve). Respirators should be used in the setting of what has been historically considered airborne infections and during aerosol-generating procedures (Table 10.6-1).
Wearing (Donning) and Using Masks
A mask should snugly fit to the face and cover the mouth and nose. Fit can be improved, for example, with the knot and tuck procedure as per the Centers for Disease Control and Prevention (CDC) (video available at youtube.com). A mask that covers only the mouth and leaves the nose exposed does not fulfill its function. Adjust its shape by pressing the metal clip along the upper edge of the mask against the nasal bridge. Similarly, the fit of respirators should be controlled with a seal check. Avoid touching or pulling the mask down (eg, under your nose or chin) while wearing it. Disinfect your hands before donning and after doffing the mask and every time you touch the outer surface of the mask (which should be treated as contaminated). Replace the mask with a new one if it gets damaged, damp, or potentially contaminated. Remove the mask in a way that minimizes the risk of contaminating the hands and other parts of the body. Avoid touching the front part of the mask. After doffing the mask, place it in a medical waste bin and disinfect the hands. Masks used by patients and medical personnel should be treated as contaminated materials.
Instructions on wearing (donning) and removing (doffing) the mask: Figure 10.6-3 and Figure 10.6-4.
Eye and Face ProtectionTop
Face shields (Figure 10.6-2, panel B), goggles (Figure 10.6-2, panel A), or safety glasses can be used to protect the eyes and face from infectious materials. Eye and face protection equipment should be used not only if there is a risk of splash of blood or other body fluids but also with exposure to IRPs to protect the eye mucosa. A face shield provides an extra barrier that protects the respiratory tract; it should be worn along with a mask, particularly during aerosol-generating procedures. Eye and face protective equipment can be used repeatedly provided that it is properly disinfected prior to reuse. Glasses used for vision correction do not provide sufficient protection in these settings.
The sequence of donning and doffing goggles and face shields: Figure 10.6-3 and Figure 10.6-4.
Hand ProtectionTop
Medical gloves play an important protective role among the medical staff and patients. They prevent hand skin contamination with microorganisms and decrease the risk of pathogen transmission in the case of needlestick or other injury. Using sterile gloves during invasive procedures helps avoid transmission of microorganisms residing on the hand skin to the patient’s sterile body cavities. Consider using tear-resistant gloves during invasive procedures that pose a risk of infection with highly infectious pathogens.
Use of gloves is indicated in the following settings:
1) Possible skin contact with patients’ blood or other potentially infectious biologic material, mucosa, or damaged skin.
2) Possible contact with a patient infected with a pathogen that spreads through direct contact or stay in close surroundings of such a patient, which may be contaminated (eg, contact with bed, bedside cabinet, everyday objects).
3) Performing or assisting with invasive procedures.
4) Damaged hand skin in an HCP.
Wearing gloves does not replace the need for hand decontamination (washing or disinfection). After contact with an infectious patient or their surroundings, remove gloves in a proper sequence to prevent hand contamination: Figure 10.6-4. Always disinfect your hands before donning and after doffing gloves. Do not wear the same pair of gloves for the care of >1 patient. Gloves should also be changed during a single procedure and care of the same patient if you touched a contaminated area of the patient’s body (eg, near an abscess) and then a noncontaminated region (eg, face).
The sequence of donning gloves to keep them sterile: Figure 10.6-3.
Protective ClothingTop
Long-sleeve, water-resistant, full-length barrier gowns and protective suits are used to protect against infectious material (Figure 10.6-2). If barrier gowns are unavailable, gowns made of fabric are acceptable in certain settings.
Individuals in whom hair may interfere with the proper use of PPE or who are at risk of head contamination should wear a cap.
Protective clothing should be donned prior to performing medical procedures and providing care in settings where there is a risk of contaminating the clothes, splash of blood or other biologic material, or direct contact transmission of pathogens. A water-resistant foil gown or an apron can be additionally worn over a standard gown or protective suit.
Remove protective clothing in the designated doffing area before returning to a regular ward. If there are no specific recommendations regarding the area where protective clothing can be doffed after having contact with an isolated patient, remove it before leaving the patient’s room and decontaminate the hands. Remove the gown or protective suit in a way that minimizes the contamination risk (Figure 10.6-4). Do not reuse the gown or protective suit. Protective clothing intended for multiple use must be properly decontaminated prior to next use.
Hand HygieneTop
Hand hygiene is the primary method of preventing infection transmission. Infection spread by HCPs’ contaminated hands is considered the most common transmission route in medical facilities.
The hands may be decontaminated by washing them with soap and water or using alcohol-based disinfectants. Do not combine both methods, as using alcohol-based disinfectants on wet skin reduces their effectiveness and increases the risk of skin irritation. HCPs should not wear jewelry or artificial nails when caring for patients.
Hand washing with soap and water is preferred in the following settings:
1) Visible hand contamination with, among others, blood or other biologic material.
2) After leaving the toilet.
3) After possible exposure to pathogens producing spores, including Clostridioides difficile.
Hand hygiene with alcohol-based disinfectants is preferred in the following settings:
1) Before and after contact with a patient.
2) After exposure to biologic fluids and contact with the mucosa, damaged skin, and dressings.
3) After contact with surfaces and objects in the patient’s close surroundings.
4) After contact with the patient’s nondamaged skin (eg, during palpation).
5) During examination or care of a patient if a contaminated area of the patient’s body has been touched before touching a noncontaminated one.
6) Before using instruments for invasive procedures.
7) Every time before donning and doffing gloves (sterile or nonsterile), a mask, or a respirator.
If an alcohol-based disinfectant is unavailable, wash the hands with soap and water. Wash the hands also before preparing meals and administering drugs.
The Sequence of Donning and Doffing PPETop
See Figure 10.6-3 and Figure 10.6-4.
Disinfect the hands before donning PPE. First put on a gown, then a mask. Check whether the mask fits snugly to the face (in the case of respirators, the entire inhaled air should pass through the mask; facial hair may not allow for proper mask fit). Next, put on goggles or a face shield. The goggles should be adjusted to the mask and worn over it. The last step is donning gloves, which should cover the wrists and gown’s sleeves.
Doffing PPE requires special attention, as the outer surface of PPE may be contaminated with infectious material. Improper or careless PPE removal may result in accidental self-contamination. Disposable equipment should be placed in an appropriate waste container immediately after removal. Equipment intended for multiple use (eg, face shields) should be placed in a special container and decontaminated before reuse according to internal procedures. If there is no internal procedure for doffing PPE, follow this sequence: first remove the gloves in a way that minimizes the risk of hand contamination and disinfect the hands. Grasp the gown behind your shoulders, pull it down and away from the sides of your body, roll the exposed side of the gown inward into a bundle, and turn the sleeves inside out (avoid touching the front part of the gown, which is contaminated). With high-risk pathogens such as the Ebola virus, wearing a new pair of gloves to remove the gown is recommended but in general not required. After doffing the gown, disinfect the hands. Then remove goggles or a face shield without touching their front parts and disinfect the hands again. Next remove the mask (grasp the ties and carefully remove the mask without touching its front), disinfect the hands. If clean gloves are used for the doffing of the other PPE, gloves are to be removed last and then hands are to be disinfected again. If another person assists you with PPE doffing, they also should wear PPE (gown, surgical mask, gloves, in some cases a gown made of, eg, fusible interfacing fabric) and decontaminate the hands after each step of doffing. Every health care center should adjust the sequence of donning and doffing PPE to the equipment available on site.
Isolation Methods and Other Methods of Infection Prevention in Health Care SettingsTop
A patient with a suspected transmittable disease should be immediately placed in an appropriate isolation room in order to prevent transmission of pathogens by IRPs or through direct contact. If it is not possible, bear in mind that the infected patient should not share the room with other patients in whom a possible infection is associated with a significant risk of complications. When sharing a room cannot be avoided, maximize the distance between beds and ensure that patients are separated from each other with a curtain or divider. Information about isolation precautions and the PPE used should be displayed at the entry to the room.
The decision to separate patients or nursing home residents receiving long-term and home care who are infected with a multidrug-resistant strain should be made on a case-by-case basis considering the infection risk and its consequences for other patients as well as negative psychologic effects of long-term isolation.
If an infected individual presents to an outpatient clinic, place them in a separate room. During periods of increased incidence of respiratory infections (eg, influenza), it is recommended that a separate waiting area be established for individuals presenting with infection symptoms and such patients be admitted urgently in order to minimize the risk of pathogen transmission among other patients waiting for admission.
Standard Prevention Measures in Patient Care
1. Maintaining hand hygiene.
2. Use of PPE by the medical staff.
3. Cleaning and disinfection of patient rooms and most frequently touched surfaces.
4. Frequent linen changes and acting in a way that prevents microorganism transmission to other individuals and the hospital environment.
5. Proper medical waste management.
6. Using safe medical equipment that decreases the risk of needlestick and other injuries among the staff.
Precautions for Respiratory Infections (Historically Droplet Transmission)
Patient isolation prevents transmission of pathogens through larger IRPs. Infected individuals should be placed in separate rooms with access to a washroom whenever possible; no forced air circulation is required inside. Patients infected with the same pathogen may share the room (cohorting); the doors to the room may be left open. Limit transport of infected patients to a minimum. Educate patients about cough etiquette and the necessity to wear medical or surgical masks covering the nose and mouth when other individuals are present in the room and during transport. Before entering the isolation room, HCPs should don medical or surgical masks, eye protection, gowns, and gloves.
Precautions for Airborne Transmission (eg, Measles, Chickenpox, Tuberculosis)
Infected patients should optimally be placed in separate rooms with access to a washroom, constant negative pressure, and forced air circulation, if available. The doors to the room should be closed. The isolation room should be entered through an anteroom, particularly if patients are infected with pathogens classified as the World Health Organization (WHO) risk groups 3 and 4. Air flowing out of the room should be purified using high-efficiency particulate air (HEPA) filters or similar equipment. The patient must wear a medical or surgical mask when other individuals are present in the room and during transport. Limit transport of infected patients to a minimum. Educate them about cough etiquette. Before entering the isolation room, HCPs should don respirators and also, for most pathogens, eye protection, gowns, and gloves.
Precautions for Direct Contact Transmission
Infection may occur through direct contact with an infected patient or the contaminated environment (bed, bedside cabinet, and other objects used by the patient). Infected individuals should be placed in separate rooms whenever possible; cohorting patients colonized or infected with the same pathogen is encouraged. Small, reusable medical equipment (eg, blood pressure monitor, thermometer) should be dedicated to a single patient only and kept in the patient’s room. If reusable equipment is shared by different patients, it should be disinfected between uses. Transport of patients should be limited to a minimum and, if unavoidable, the shortest route should be used. If possible, cover the infected or colonized areas of the patient’s body during transport. Cleaning the patients’ rooms, including frequently touched equipment and surfaces, should be a priority. The bed and bedside cabinet should be properly decontaminated before allowing another individual to reuse them.
HCPs should wear gloves and gowns and, if there is risk of splash, an impermeable apron. PPE should be donned before entry to the patient’s room and doffed shortly before exit, unless there is a designated area (eg, a special zone or a “dirty” anteroom) to allow the doffing process outside of the room.
Precautions for Blood-Borne Pathogens
HCPs may develop infection as a result of skin injury (needlestick or other injury caused by equipment contaminated with blood or other biologic material) or splash onto the mucosa or damaged skin (see Occupational Exposures to Blood-Borne Viral Infections). If possible, use medical devices with safety features that disable sharps after use and therefore protect against needlesticks and other injuries. Sharps should be kept in special hard-sided containers. HCPs who perform procedures that pose a risk of contact with potentially infectious materials should wear PPE, particularly gloves and PPE preventing splash into ocular, oral, and nasal mucous membranes, as applicable.
Tables and FiguresTop

Figure 10.6-1. Masks and respirators: A, 3-layer surgical mask; B, FFP2 respirator; C, respirator with an exhalation valve; D, N95 respirator.
|
Aerosol-generating medical procedures |
|
– Intubation, extubation, and related procedures (eg, manual ventilation and open deep suctioning) – Tracheotomy/tracheostomy procedures (insertion, open suctioning, removal) – Bronchoscopy – Surgical procedures using high-speed devices in the respiratory tract – Certain dental procedures (eg, high-speed drilling and ultrasonic scalers) – Noninvasive ventilation (eg, BiPAP and CPAP) – HFOV – Induction of sputum with nebulized saline, nebulization, aerosol therapy – High-flow nasal oxygen therapy (with HFNC) |
|
Facilities in which aerosol-generating medical procedures are frequently performed |
|
– ICUs – Postoperative wards providing invasive and noninvasive mechanical ventilation – Emergency departments – Hospital wards providing noninvasive ventilation – Dental practices – Endoscopy units |
|
Based on www.publichealthontario.ca. |
|
BiPAP, bilevel positive airway pressure; CPAP, continuous positive airway pressure; HFNC, high-flow nasal cannula; HFOV, high-frequency oscillatory ventilation; ICU, intensive care unit. |
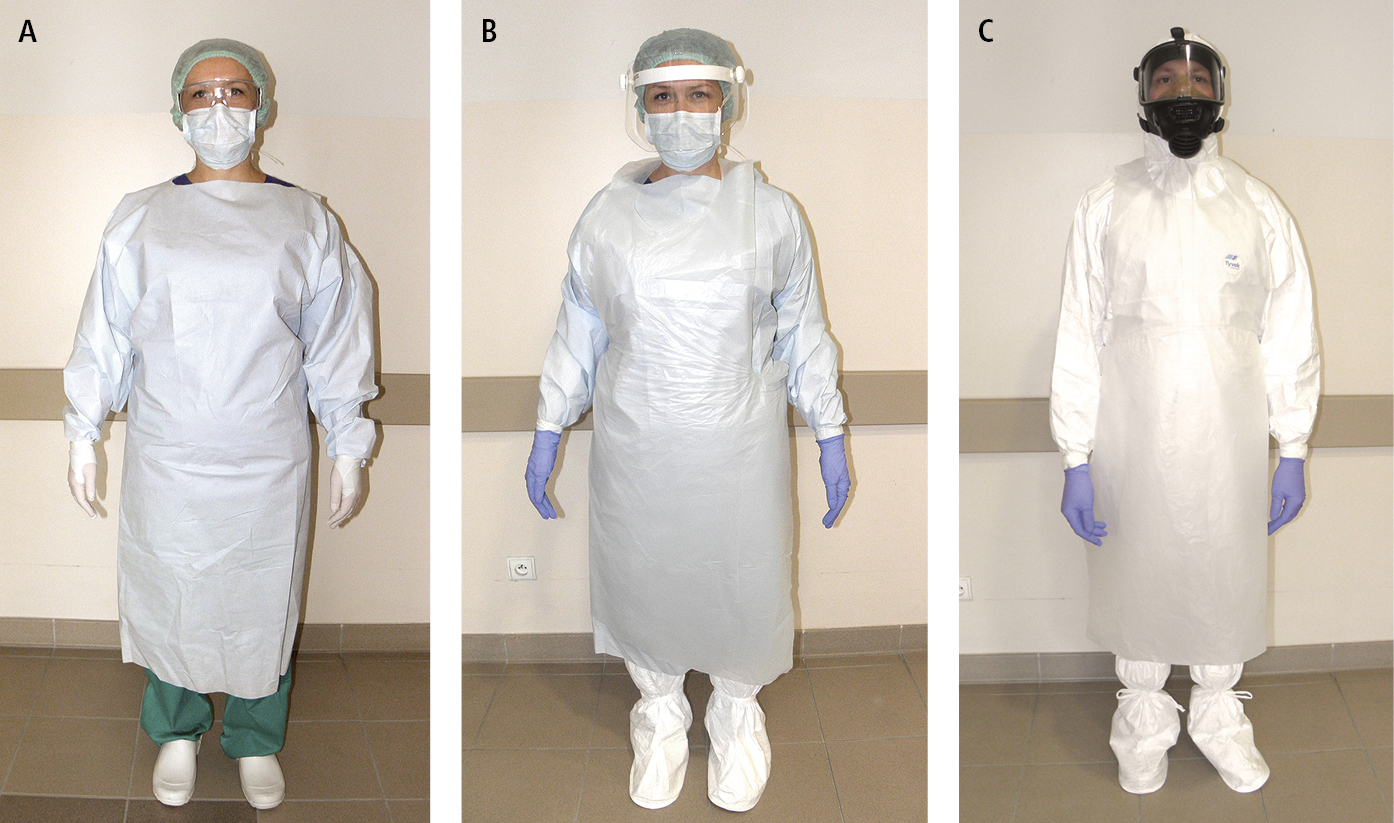
Figure 10.6-2. Personal protective equipment (PPE) for body protection: A, mask, goggles, impermeable gown (basic PPE); B, face shield, extra gown, shoe covers (additional PPE); C, reusable respirator, protective suit with hood, shoe covers (specialized PPE).
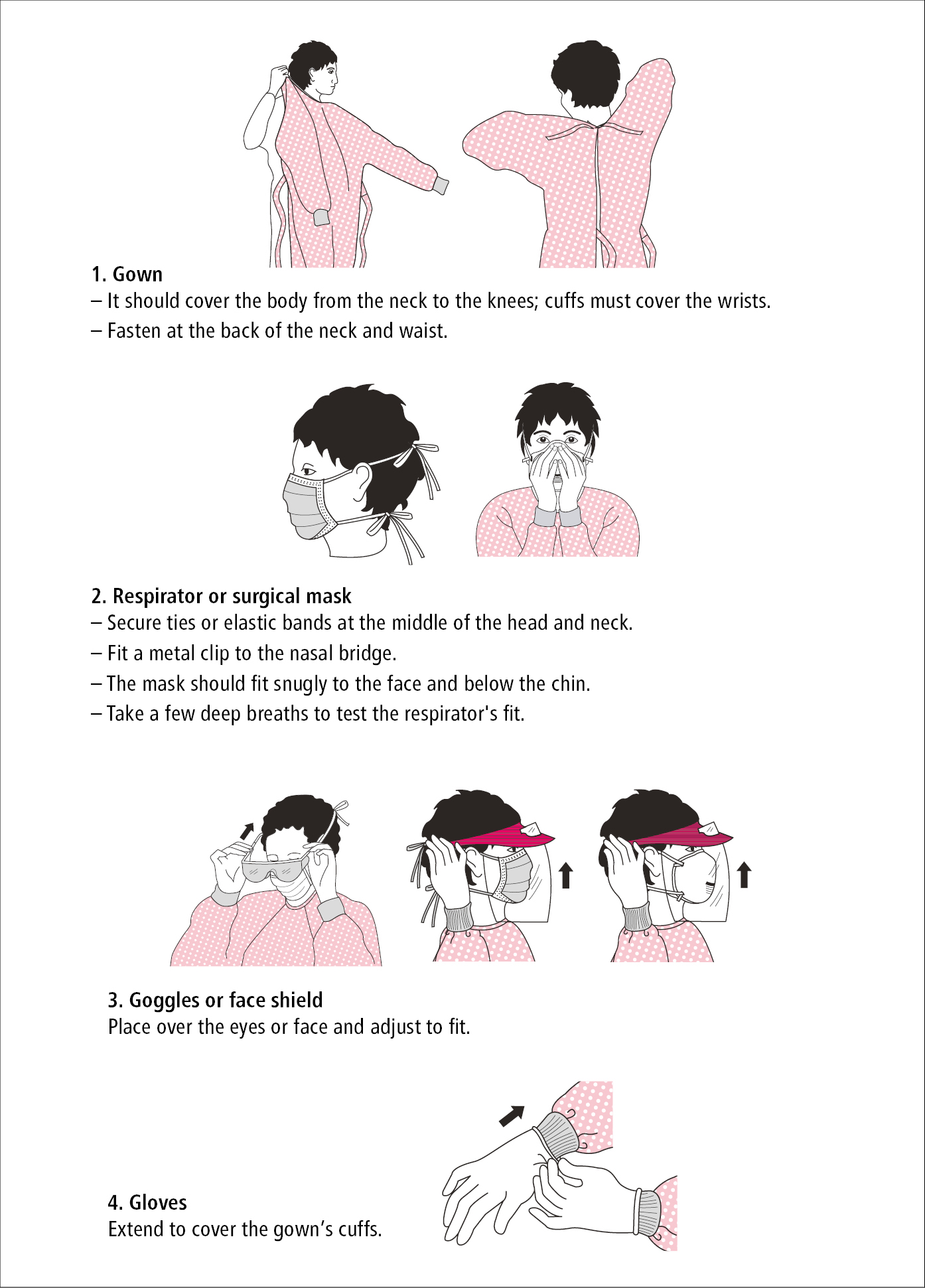
Figure 10.6-3. The sequence of wearing (donning) personal protective equipment (PPE). Based on the Centers for Disease Control and Prevention (CDC) instructions.
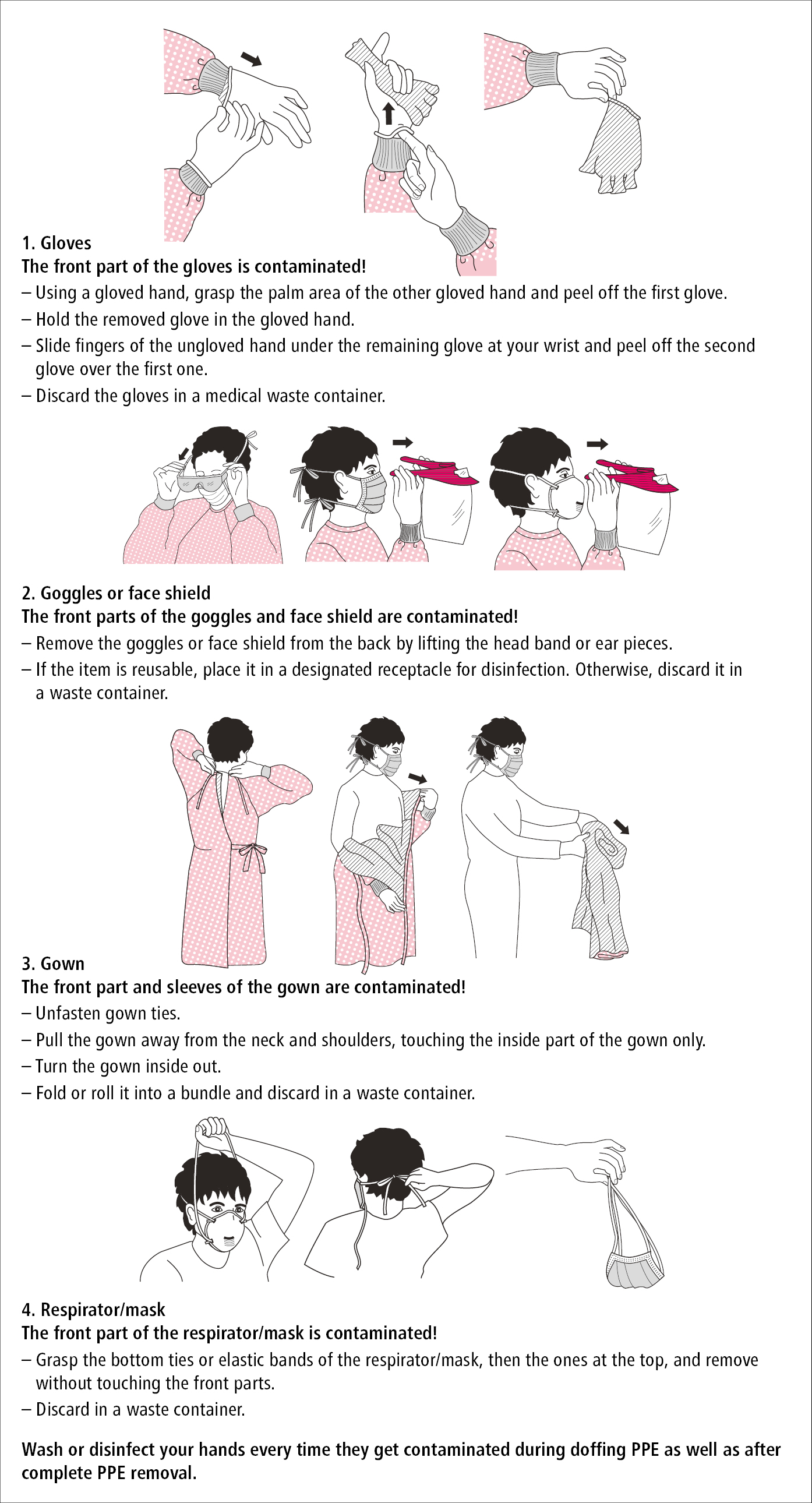
Figure 10.6-4. The sequence of removing (doffing) personal protective equipment (PPE). Based on the Centers for Disease Control and Prevention (CDC) instructions.