Arbelo E, Protonotarios A, Gimeno JR, et al. 2023 ESC Guidelines for the management of cardiomyopathies. Eur Heart J. 2023;44(37):3503-3626. doi:10.1093/eurheartj/ehad194
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022 May 3;79(17):1757-1780. doi: 10.1016/j.jacc.2021.12.011. Epub 2022 Apr 1. PMID: 35379504.
McDonald M, Virani S, Chan M, et al. CCS/CHFS Heart Failure Guidelines Update: Defining a New Pharmacologic Standard of Care for Heart Failure With Reduced Ejection Fraction. Can J Cardiol [Internet]. 2021 Apr;37(4):531-546. doi: 10.1016/j.cjca.2021.01.017. PMID: 33827756.
Bozkurt B, Coats AJ, Tsutsui H, et al. Universal Definition and Classification of Heart Failure: A Report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J Card Fail. 2021 Mar 1;S1071-9164(21)00050-6. doi: 10.1016/j.cardfail.2021.01.022. PMID: 33663906.
McDonagh TA, Metra M, Adamo M, et al; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-3726. doi: 10.1093/eurheartj/ehab368. Erratum in: Eur Heart J. 2021 Dec 21;42(48):4901. PMID: 34447992.
Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2020 Dec 22;76(25):e159-e240. doi: 10.1016/j.jacc.2020.08.045. Epub 2020 Nov 20. PMID: 33229116.
Bozkurt B, Colvin M, Cook J, et al; American Heart Association Committee on Heart Failure and Transplantation of the Council on Clinical Cardiology; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Epidemiology and Prevention; and Council on Quality of Care and Outcomes Research. Current Diagnostic and Treatment Strategies for Specific Dilated Cardiomyopathies: A Scientific Statement From the American Heart Association. Circulation. 2016 Dec 6;134(23):e579-e646. Epub 2016 Nov 3. Erratum in: Circulation. 2016 Dec 6;134(23):e652. PMID: 27832612.
WRITING COMMITTEE MEMBERS, Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2016 Sep 27;134(13):e282-93. doi: 10.1161/CIR.0000000000000435. Epub 2016 May 20. Erratum in: Circulation. 2016 Sep 27;134(13):e298. PMID: 27208050.
Ponikowski P, Voors AA, Anker SD, et al; Authors/Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016 Jul 14;37(27):2129-200. doi: 10.1093/eurheartj/ehw128. Epub 2016 May 20. Erratum in: Eur Heart J. 2016 Dec 30. PMID: 27206819.
Hilfiker-Kleiner D, Haghikia A, Nonhoff J, Bauersachs J. Peripartum cardiomyopathy: current management and future perspectives. Eur Heart J. 2015 May 7;36(18):1090-7. doi: 10.1093/eurheartj/ehv009. Epub 2015 Jan 29. Review. PMID: 25636745; PMCID: PMC4422973.
1. Stress-induced (takotsubo) cardiomyopathy is a nonfamilial cardiomyopathy characterized by acute left ventricular (LV) dysfunction after emotional, physical, or physiologic stress. It is a form of myocardial stunning that is associated with hyperkinesis of the basal LV segments, akinesis of mid LV segments, and dyskinesis of the apical LV segments.
Clinically takotsubo cardiomyopathy can present with ST-segment elevations followed by inverted T waves associated with chest pain and elevations in serum troponin levels. As such, this is a diagnosis of exclusion after acute coronary syndrome has been ruled out. Complications can include LV outflow tract obstruction, shock, LV thrombus, as well as ventricular and atrial arrhythmias. Given the transient nature of the phenomenon, LV contractility often normalizes within days to weeks, and electrocardiography changes resolve much later, within weeks or months. For this reason classification as a cardiomyopathy is not recommended. The prognosis is often good unless complications arise.
2. LV noncompaction or LV hypertrabeculation is a ventricular phenotype characterized by prominent trabeculations in the LV myocardium due to failure of compaction of the trabeculae during gestation. Although frequently seen as a familial trait, it has also been described as acquired and associated with a transient phenomenon in athletes and during pregnancy. For this reason, it should not be considered a cardiomyopathy. Clinical features include systolic dysfunction with heart failure, thromboembolic complications, arrhythmias, and sudden cardiac death. Diagnosis is made based on characteristic features found on echocardiography (Figure 3.6-5) and confirmed by cardiac magnetic resonance (CMR) (Figure 3.6-1).
FiguresTop
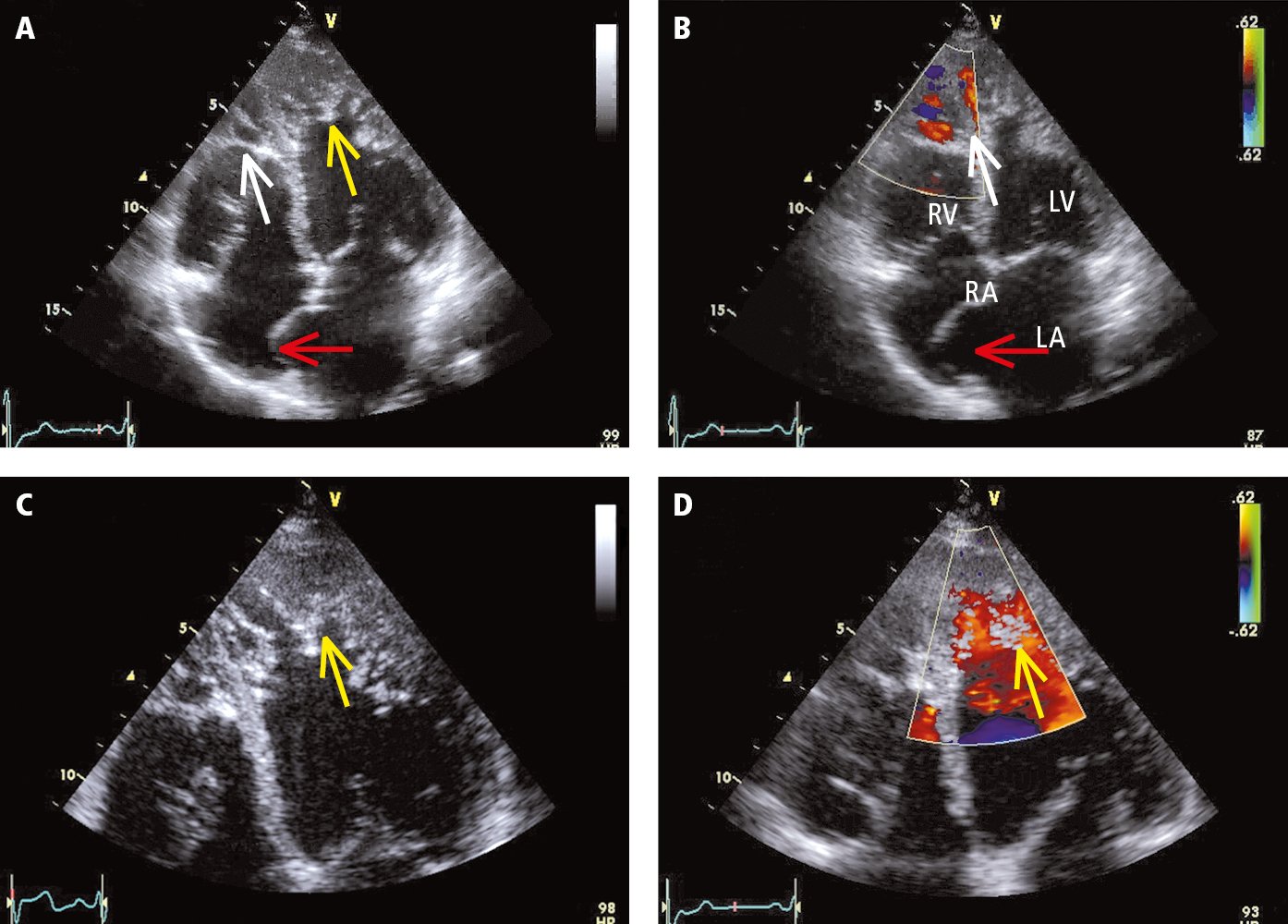
Figure 3.6-5. Transthoracic echocardiography (TTE) of a patient with left ventricular noncompaction (apical 4-chamber view, standard probe placement): A, 2D imaging; B, color Doppler examination; C, enlarged panel A; D, color Doppler examination. Yellow arrows mark the spongiform structure of the myocardium in the mid and apical segments of the left ventricle (LV). The layer of the abnormal cardiac muscle is more than twice as thick as the healthy compact layer. A healthy apex of the right ventricle (RV) usually has numerous myocardial trabeculae. For this reason, despite the significantly increased trabeculation (white arrow), it is not clear if this finding can be considered abnormal. Color Doppler revealed blood flow penetrating deep into both ventricular apexes, which indicates that tissue in this area is not solid (a solid tissue structure would be typical for apical hypertrophic cardiomyopathy or ventricular cavities filled with thrombi or other masses). The interatrial septum is markedly protruding to the right (red arrow), which meets the diagnostic criteria for atrial septal aneurysm. LA, left atrium; RA, right atrium. Figure courtesy of Dr Andrzej Gackowski.

Figure 3.6-1. Left ventricular (LV) hypertrabeculation on cardiac magnetic resonance (CMR). The major marker is the presence of several prominent trabeculations in the LV with topographic involvement of apical and mid segments of the lateral and inferior walls. A noncompacted-to-compacted ratio >2.3 on CMR is considered the cutoff for the diagnosis of left ventricular noncompaction. Figure courtesy of Dr Danielle Walker.