Stringer T, Femia AN. Raynaud's phenomenon: Current concepts. Clin Dermatol. 2018 Jul - Aug;36(4):498-507. doi: 10.1016/j.clindermatol.2018.04.007. Epub 2018 Apr 10. Review. PubMed PMID: 30047433.
Maverakis E, Patel F, Kronenberg DG, et al. International consensus criteria for the diagnosis of Raynaud's phenomenon. J Autoimmun. 2014 Feb-Mar;48-49:60-5. doi: 10.1016/j.jaut.2014.01.020. Epub 2014 Feb 1. Review. PubMed PMID: 24491823; PubMed Central PMCID: PMC4018202.
Definition and EtiologyTop
Raynaud phenomenon is an acute reversing blanching of the fingers and toes, rarely also of the nose and ears, in response to cold, emotional stressors, or without an obvious cause. The following types of Raynaud phenomenon are distinguished:
1) Primary Raynaud phenomenon, found in ~80% of patients.
2) Secondary Raynaud phenomenon, which may develop as a result of various diseases and conditions (Table 3.19-7).
Clinical FeaturesTop
Phases of Raynaud phenomenon:
1) Ischemic phase: Whitening or blanching of the fingers or toes, rarely of entire hands or feet; sharply demarcated pallor of the affected body parts with accompanying numbness (Figure 3.19-1).
2) Cyanotic phase: Blue or purple discoloration accompanied by a feeling of numbness and pain.
3) Hyperemic phase: Reddening, mild edema, cutaneous sensation of burning and heat.
In patients with secondary Raynaud phenomenon the vasomotor symptoms are usually more pronounced than in patients with primary Raynaud phenomenon. The cyanotic phase is often dominant. Ulcerations and necrosis of the fingertips develop more frequently. The thumb is not usually involved in primary Raynaud phenomenon.
DiagnosisTop
Primary Raynaud phenomenon is diagnosed when there are no features of an underlying condition in history, physical examination, or results of specific investigations suggestive of etiology, making an idiopathic cause likely.
Secondary Raynaud phenomenon is diagnosed after identifying an underlying condition that may be causative. Secondary causes should be established through history, physical examination, and any relevant laboratory investigations. The adequacy of cancer screening should be reviewed, particularly in men and in patients with the onset of Raynaud phenomenon >30 years of age.
Differential diagnosis should include benign cold sensitivity, peripheral neuropathy, acrocyanosis, Buerger disease, vascular disease (atherosclerosis), vasculitis, toxins, cryoglobulinemia, and erythromelalgia.
TreatmentTop
1. Nonpharmacologic treatment: Avoidance of exposure to cold, smoking cessation, avoidance of caffeinated beverages, avoidance of oral contraceptives and vasoconstrictive drugs.
2. Pharmacologic treatment: In severe primary and secondary Raynaud phenomenon, treat the underlying condition (where applicable) and use a long-acting oral dihydropyridine calcium channel blocker (eg, amlodipine, nifedipine). Start at low doses (eg, nifedipine 10 mg tid) and titrate upwards (eg, to nifedipine sustained-release 60 mg daily) based on the effectiveness of treatment and adverse effects. Additional therapeutic options include topical nitrates, angiotensin receptor blockers, phosphodiesterase-5 inhibitors (eg, sildenafil, tadalafil), selective serotonin reuptake inhibitors (eg, fluoxetine), or endothelin-1 receptor antagonists (eg, bosentan). In patients with severe digital ischemia or development of necrotic lesions, urgent treatment with warming and calcium channel blockers should be initiated; prostaglandin infusion (eg, iloprost) can limit the damage and can be considered in case of secondary Raynaud phenomenon.Evidence 1Weak recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to heterogeneity, indirectness, and relying on expert opinion only. Ingegnoli F, Schioppo T, Allanore Y, et al. Practical suggestions on intravenous iloprost in Raynaud's phenomenon and digital ulcer secondary to systemic sclerosis: Systematic literature review and expert consensus. Semin Arthritis Rheum. 2019 Feb;48(4):686-693. doi: 10.1016/j.semarthrit.2018.03.019. Epub 2018 Apr 4. PubMed PMID: 29706243. Antithrombotic agents, acetylsalicylic acid, or therapeutic doses of low-molecular-weight heparin are used to treat potential thrombotic events after considering contraindications (eg, gastric antral vascular ectasia or severe gastritis, both of which are seen in systemic sclerosis).
3. Surgical treatment: In selected patients not responding to pharmacologic treatment, in particular those at high risk for necrosis of the fingers, digital or axillary sympathectomy may be considered.
Tables and FiguresTop
|
Systemic connective tissue diseases |
– Systemic sclerosis – Systemic lupus erythematosus – Rheumatoid arthritis – Sjögren syndrome – Antiphospholipid syndrome – Eosinophilic fasciitis – Mixed connective tissue disease – Juvenile idiopathic arthritis – Myositis – Primary biliary cirrhosis |
|
Vasculitides |
– Behçet disease – Buerger disease – Takayasu disease – Polyarteritis nodosa – Other systemic vasculitides – Atherosclerosis (rare) – Diabetic microangiopathy – Microembolization – Giant cell arteritis – Granulomatosis with polyangiitis (Wegener granulomatosis) |
|
Occupational exposure |
– Vibration and repetitive mechanical finger injuries – Exposure to cold |
|
Intoxication and chemical agents |
– Vinyl chloride poisoning – Cocaine – Heavy metal poisoning (lead, thallium) – Nicotine – Acrylic artificial nails |
|
Blood disorders |
– Leukemia and lymphoma – Cold agglutinin disease – Polycythemia vera – Monoclonal and polyclonal cryoglobulinemia – Cryofibrinogenemia – Essential thrombocythemia – Multiple myeloma – Disseminated intravascular coagulation |
|
Central nervous system disorders |
– Syringomyelia – Tabes dorsalis |
|
Compression syndromes |
– Thoracic outlet syndrome – Carpal tunnel syndrome – Compression syndrome following use of forearm crutches |
|
Drugs |
– Beta-blockers – Oral contraceptives – Vincristine – Bleomycin – Cyclosporine – Interferon alpha – Interferon gamma – Ergot derivatives |
|
Infectious diseases |
– Leprosy – Cytomegalovirus infection – Parvovirus infection – Mycoplasma pneumoniae infection – Helicobacter pylori infection – Hepatitis B – Hepatitis C |
|
Other disorders |
– Anorexia nervosa – Cancer – Frostbite – Primary or secondary pulmonary hypertension – Arteriovenous shunts (including those related to dialysis) – Familial cold urticaria – Carney complex |
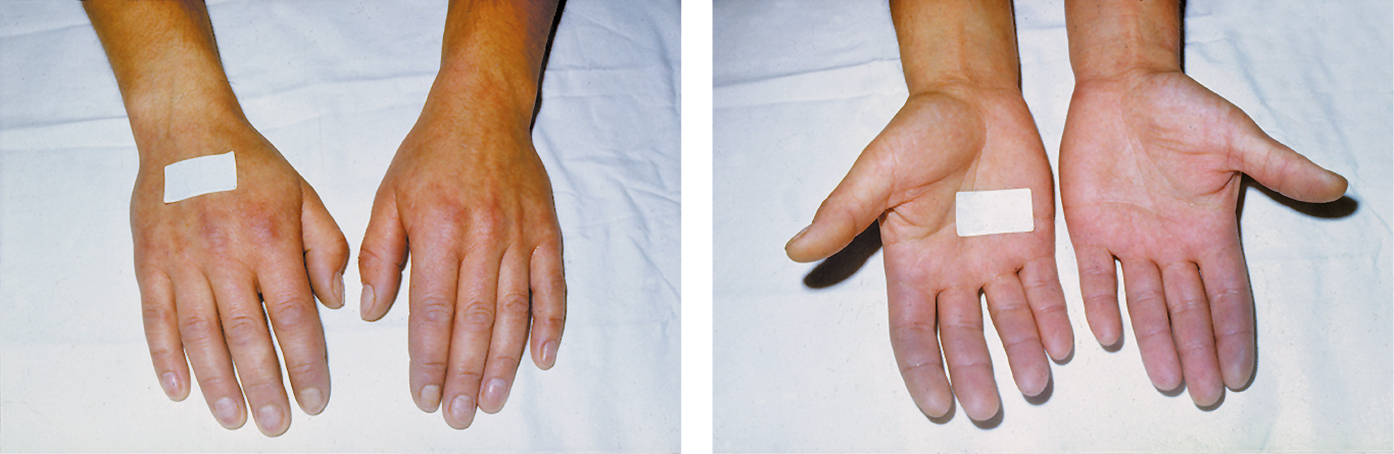
Figure 3.19-1. Raynaud phenomenon. Cyanosis affecting fingers of both hands. Figure courtesy of Dr Leszek Masłowski.