Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e35-e71. doi: 10.1161/CIR.0000000000000932. Epub 2020 Dec 17. Erratum in: Circulation. 2021 Feb 2;143(5):e228. Erratum in: Circulation. 2021 Mar 9;143(10):e784. PMID: 33332149.
Miller MA, Dukkipati SR, Turagam M, Liao SL, Adams DH, Reddy VY. Arrhythmic Mitral Valve Prolapse: JACC Review Topic of the Week. J Am Coll Cardiol. 2018 Dec 11;72(23 Pt A):2904-2914. doi: 10.1016/j.jacc.2018.09.048. PMID: 30522653.
Baumgartner H, Falk V, Bax JJ, et al; ESC Scientific Document Group. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017 Sep 21;38(36):2739-2791. doi: 10.1093/eurheartj/ehx391. PMID: 28886619.
Definition, Etiology, PathogenesisTop
Mitral valve prolapse (MVP) is displacement of a part of ≥1 mitral leaflet into the left atrium during left ventricular contraction, which may or may not be associated with mitral regurgitation.
MVP syndrome (previously known as the “floppy valve” or Barlow syndrome) is a group of symptoms, including chest pain, palpitations, arrhythmias, dizziness, and syncope, which are associated with MVP.
Primary MVP results from degeneration of the leaflets, chordae tendineae, or both. It may be familial or sporadic (can be further classified as syndromic or nonsyndromic). Secondary MVP occurs in patients with connective tissue diseases (eg, Marfan syndrome), acute endocarditis (due to rupture of chordae tendineae), as well as ischemic heart disease (eg, due to rupture of a papillary muscle in patients with myocardial infarction). Rupture of chordae tendineae may present as a flail leaflet (see Mitral Regurgitation).
MVP may be accompanied by tricuspid and aortic valve disease and sometimes by an aneurysm or atrial septal defect.
Clinical Features and Natural HistoryTop
1. Symptoms: Chest pain, palpitations, dizziness, collapse, and syncope.
2. Signs: Typically a mid- or late-systolic click, late-systolic or holosystolic murmur (abnormal heart sounds are more pronounced with standing; absence of these signs argues against MVP).
3. Natural history varies from mild, asymptomatic cases to patients at high risk of death.
DiagnosisTop
Diagnosis is based on clinical features (if present) and echocardiography results.
1. Electrocardiography (ECG) is normal in the majority of patients. In some symptomatic patients, nonspecific ST-segment changes in leads II, III, and aVF (rarely in V4-V6) and arrhythmia may be observed.
2. Chest radiography is usually normal, except for severe chronic or acute mitral regurgitation (MR).
3. Echocardiography (Figure 3.18-8) is performed to diagnose MVP in asymptomatic patients with typical findings on auscultation, and to exclude MVP in patients with suspected MVP who have no typical findings on auscultation.
TreatmentTop
1. Asymptomatic patients or patients with mild symptoms and favorable echocardiographic findings: Reassure the patient of good prognosis. Recommend normal lifestyle, regular exercise, and follow-up every 3 to 5 years (unless there is significant MR).
2. Patients with paroxysmal palpitations accompanied by anxiety, chest pain, and fatigue: Beta-blockers may be beneficial.
3. Patients after a transient ischemic attack or stroke: Start an appropriate antiplatelet regimen, unless the patient otherwise qualifies for systemic anticoagulation.
4. Patient with a history of atrial fibrillation (AF) or left atrial thrombus: Start long-term anticoagulant treatment for AF as indicated by the estimated risk score for embolic stroke and regardless of stroke risk in the presence of left atrial thrombus (see Atrial Fibrillation).
5. Surgical treatment should be considered in patients with myxomatous valves and severe MR, even in the absence of symptoms, left ventricular dilatation, or systolic impairment, if the mitral valve has a high chance of repair in experienced surgical hands.Evidence 1Weak recommendation (benefits clearly outweigh downsides; right action for all or almost all patients). Weak rather than strong recommendation due to unclear generalizability of excellent results of repair obtained in experienced centers. Low Quality of Evidence (low confidence that we know true effects of intervention). Quality of Evidence lowered due to the observational nature of data. Suri RM, Vanoverschelde JL, Grigioni F, et al. Association between early surgical intervention vs watchful waiting and outcomes for mitral regurgitation due to flail mitral valve leaflets. JAMA. 2013 Aug 14;310(6):609-16. doi: 10.1001/jama.2013.8643. PMID: 23942679. In cases where mitral valve repair is not possible or fails, mitral valve replacement must be performed (see Mitral Regurgitation).
6. Percutaneous mitral valve repair using the edge-to-edge procedure (a mitral valve clip) is a less invasive method of percutaneous treatment in selected patients who are generally ineligible for surgery because of high/prohibitive perioperative risk.
7. Ventricular arrhythmias: MVP is associated with sudden cardiac death. Multiple risk factors for malignant ventricular arrhythmias have been identified (pattern and extent of late gadolinium enhancement on magnetic resonance imaging [MRI], presence of mitral annular disjunction, burden and complexity of ventricular ectopy, severity of MR, and female sex). Prophylactic implantable cardioverter-defibrillator (ICD) placement in this patient population is not well defined.
PrognosisTop
Prognosis is generally favorable. Factors associated with an increased risk of death include severe and possibly moderate MR, left ventricular ejection fraction <50%, unfavorable echocardiographic findings (severe thickening or elongation of a leaflet, or both), and presence of pulmonary hypertension. Patients with MVP and ≥1 of the following conditions should not engage in competitive sports: history of loss of consciousness of unexplained cause, family history of sudden cardiac death in persons with MVP, paroxysmal supraventricular arrhythmias or complex ventricular arrhythmias (particularly occurring or worsening during exercise), severe MR, left ventricular dysfunction, Marfan syndrome, long QT syndrome.
FiguresTop
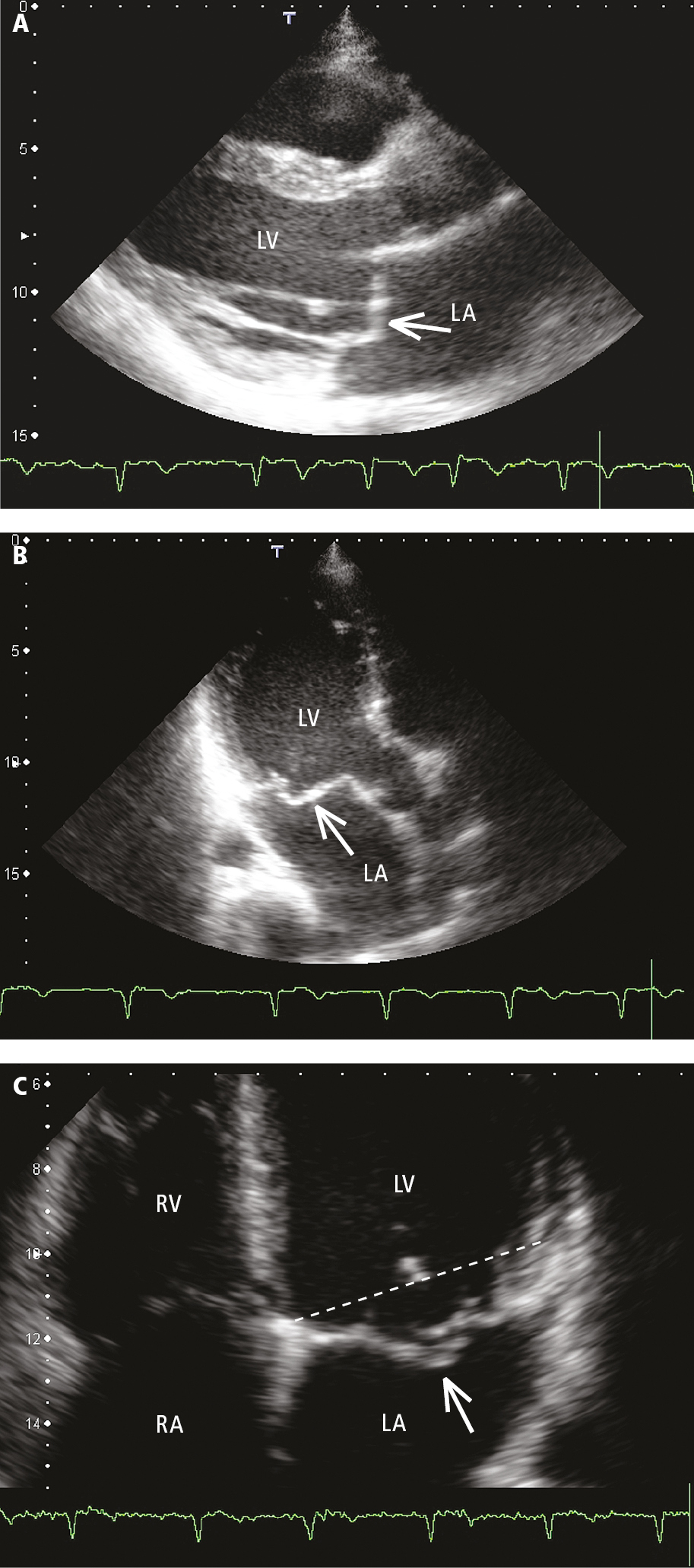
Figure 3.18-8. Transthoracic echocardiography (TTE): anterior mitral valve prolapse in parasternal (A) and apical long-axis (B) views. C, bileaflet mitral valve prolapse, apical 4-chamber view; the dotted line marks the level of the mitral annulus. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.