Canadian Adult Clinical Practice Guidelines. Obesity Canada. Accessed January 1, 2021. https://obesitycanada.ca/guidelines/chapters
World Health Organization. Noncommunicable Diseases Progress Monitor 2017. Published September 1, 2017. https://www.who.int/publications/i/item/9789241513029
Vallis M, Piccinini-Vallis H, Sharma AM, Freedhoff Y. Clinical review: modified 5 As: minimal intervention for obesity counseling in primary care. Can Fam Physician. 2013 Jan;59(1):27-31. PMID: 23341653; PMCID: PMC3555649.
Sharma AM. M, M, M & M: a mnemonic for assessing obesity. Obes Rev. 2010 Nov;11(11):808-9. doi: 10.1111/j.1467-789X.2010.00766.x. PMID: 21182728.
Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009 Mar 28;373(9669):1083-96. doi: 10.1016/S0140-6736(09)60318-4. Epub 2009 Mar 18. PMID: 19299006; PMCID: PMC2662372.
Definition, Etiology, PathogenesisTop
The World Health Organization (WHO) defines obesity as a chronic disease characterized by an accumulation of excessive, abnormal, or excessive and abnormal adipose tissue that impairs health. It is diagnosed with a body mass index (BMI) (weight divided by height squared) ≥30 kg/m2 and further divided into class I (BMI, 30-34.9 kg/m2), class II (BMI, 35-39.9 kg/m2), and class III (BMI ≥40 kg/m2) obesity.
Individuals with a BMI ≥35 kg/m2 are defined as having severe obesity. A BMI between 18.5 and 24.9 kg/m2 is considered a healthy body weight. A BMI of 25 to 29.9 kg/m2 is overweight. The recommended BMI cutoff for overweight in adults of South, Southeast, or East Asian ethnicity is ≥23 kg/m2. Although BMI is generally accepted as a diagnostic tool for obesity, it does not directly measure adiposity-related health issues or fat distribution. Therefore, obesity should be diagnosed using BMI in conjunction with waist circumference and adiposity-related complications (eg, using the Edmonton Obesity Staging System [EOSS]; see below).
The rate of obesity is increasing dramatically across all countries. From 1975 to 2014 it increased from 3.2% to 10.8% in men and from 6.4% to 14.9% in women. It is estimated that 18% of men and 21% of women worldwide will have obesity by 2025.
The etiology and pathophysiology of obesity are complex and include interactions between genetic, biologic, behavioral, psychosocial, and environmental factors. Ultimately, however, obesity is the result of an imbalance between energy consumption and energy expenditure. When energy consumption exceeds energy expenditure, the excess energy is converted into fat and stored in adipose tissue. Specific considerations include:
1) Appetite regulation (Figure 6.5-1), which involves 3 main regions of the brain:
a) Hypothalamus (homeostatic control): Energy homeostasis (energy consumption and expenditure) is regulated by the hypothalamus. Hunger sensations and food-seeking behaviors are prompted when orexigenic neurons (agouti-related protein [AgRP] and neuropeptide Y [NPY] neurons) in the arcuate nucleus of the hypothalamus are activated by hormonal and neural signals from the gut, adipose tissue, and peripheral organs, and some other anorexigenic neurons are inhibited (eg, cocaine- and amphetamine-regulated transcript [CART] neurons). Ghrelin (produced in the stomach, labeled as “hunger hormone”) increases appetite, whereas leptin (from adipose tissues), insulin (produced in the pancreas), peptide YY (PYY), and glucagon-like peptide 1 (GLP-1) (both produced in the bowel) promote satiety.
b) Mesolimbic system (hedonic control): The mesolimbic system (hedonic area) is involved with and provides the emotional, pleasurable, and rewarding features of eating (hedonic eating), which are based on the feelings of reward and pleasure that are related to seeing, smelling, or eating food. This implies that even when an individual is fully satiated, the brain may crave or enjoy food. Dopamine and opioid neurotransmitter pathways are important in the mesolimbic system.
c) Prefrontal lobe (executive control): The homeostatic and hedonic signals converge on the prefrontal cortex, which regulates eating behavior and controls decisions about preferences for eating one food type over the other. In patients with obesity this control mechanism can become dysfunctional, resulting in altered decision-making processes.
2) Adipose tissue: Adipose tissue is no longer considered an inert organ dedicated solely to the storage of fat. An ongoing positive energy balance (excess calories) together with an impaired expandability of subcutaneous adipose tissue are the hallmarks of adipose tissue dysfunction. Dysfunctional adipose tissue produces fat-derived proinflammatory cytokines, or adipokines (including tumor necrosis factor alpha, interleukins, C-reactive protein, and monocyte chemotactic protein 1). This proinflammatory state can result in the development and progression of many comorbidities associated with adiposity, such as type 2 diabetes, hypertension, dyslipidemia, metabolic dysfunction–associated steatotic liver disease (MASLD) (previously known as nonalcoholic fatty liver disease [NAFLD]), polycystic ovary syndrome (PCOS), obstructive sleep apnea (OSA) (STOP-BANG questionnaire for OSA: mdcalc.com), and atherosclerotic cardiovascular disease.
3) Other factors implicated in the pathogenesis of obesity: Several medications used for the treatment of common obesity-related conditions—including diabetes (thiazolidinediones, sulfonylureas, insulin), hypertension, depression, and other psychiatric disorders (neuroleptics)—are recognized as contributing to weight gain (Table 6.5-1). Other contributors include inadequate amount of physical activity, chronic stress, poor sleep pattern, and modern energy-saving conveniences, such as cars and remote controls.
Screening and AssessmentTop
Evaluation of anthropometric parameters (BMI and waist circumference [WC]) is recommended as a screening tool to identify patients with adiposity. It is our pattern to ask the patient’s permission to discuss the topic of obesity and to conduct anthropometric measurements prior to initiating screening or assessment.
1. BMI:
1) Measurement: The patient should be barefoot and in light clothing for all anthropometric measurements. To calculate BMI, weight expressed in kilograms is divided by the square of the body height in meters (kg/m2). Most calculators allow changing between metric and standard systems (eg, calculator from the US National Heart, Lung, and Blood Institute).
2) Limitations: BMI is not a direct measure of body fat, cardiovascular risk, or health. It does not indicate body fat distribution or account for muscle mass (it overestimates body fat in muscular individuals and can underestimate body fat in people who have lost muscle mass [sarcopenic obesity]). BMI is less accurate in certain populations (eg, the elderly, people with physical disability, people <18 years of age, people with severe obesity, pregnant women, and patients with ascites or severe edema). It also overestimates or underestimates body fat in certain ethnic groups (eg, Indigenous peoples, South Asians, Chinese).
2. WC is suggested as a surrogate measure of abdominal and visceral fat, due to the limitations of BMI in assessing fat composition and distribution as well as the anatomic differences in fat deposition. A WC ≥102 cm in men or ≥88 cm in women indicates higher risk of visceral adiposity and cardiometabolic comorbidities in the United States and Canada. A lower cutoff for WC is recommended for adults of a predominantly South Asian, Southeast Asian, or East Asian ethnicity (≥85 cm in men, ≥75 cm in women).
1) Measurement: Clothing should be removed from the waistline. The patient should stand with their feet shoulder-width apart and a straight back. Palpate the abdomen to find the inferior margin of the last rib at the level of the midaxillary line. Measure the WC at the end of a normal expiration midway between the inferior margin of the last rib and the crest of the ileum in a horizontal plane using a stretch-resistant tape. A video tutorial on WC measurement is available on the YouTube channel of Diabetes UK.
2) Limitations: WC is not a direct measure of visceral fat and a less sensitive measure of visceral fat with increasing BMI. Training and standardization are required to ensure interreader and intrareader reproducibility. WC cutoffs vary among ethnic populations.
These tools are designed to help with assessing the severity and consequences of obesity:
1) EOSS (J Obes. 2015;2015:619734): A 5-stage system (stages 0-4) that takes into consideration the presence of obesity-associated metabolic, physical, and psychologic abnormalities. It helps establish the severity of the disease, predict prognosis, and tailor the intensity of treatment required.
2) 4M’s for interdisciplinary team weight management care (obesitycanada.ca): After diagnosis, the clinical assessment for obesity should identify possible causes leading to weight gain (primary goal), establish the extent to which weight has impacted the patient’s health, and systematically search for barriers in obesity management. The 4M’s framework (mechanical, mental health, metabolic, social milieu) is a clinical tool that allows a practical approach for primary care physicians to explore the major drivers, barriers, and complications of obesity. It can aid health care professionals in conducting an efficient and complete obesity assessment, including history, physical examination, and investigations.
Obesity-Centered Medical History
Obesity-focused history taking allows for a more individualized management. Key areas that need to be covered include:
1) Time line of life events and weight history: Standard history taking includes mapping the relevant life events associated with changes in weight, such as quitting smoking and changing marital status, on a timeline.
2) Onset of weight gain: Early onset of obesity is a predictor of severe obesity in adulthood.
3) Dietary and physical activity assessment: A comprehensive dietary and physical activity history should be obtained in all patients before offering advice.
4) Sleep hygiene: Both quality and amount of sleep should be carefully explored.
5) History of psychiatric disorders: When taking a history remember to inquire about physical, sexual, and psychologic abuse, internalized weight bias, mood and anxiety disorders, substance use disorder, and addiction. It is important to ask relevant questions about disordered eating behaviors, such as binge eating disorder, bulimia, or night-eating syndrome. Identification of psychologic conditions that may impair treatment, such as attention deficit disorder or posttraumatic stress disorder, should be an integral part of history taking.
6) Weight gain–promoting medications: Obtain a detailed history of medications that cause weight gain.
Obesity-Centered Physical Examination
Key components of an obesity-centered physical examination include:
1) Vital signs (blood pressure taken with a cuff of appropriate size, heart rate).
2) Anthropometric measurements (height, weight, WC, BMI).
3) Neck circumference measurement may help determine the risk of sleep apnea.
4) Screening for signs of Cushing syndrome, hypothyroidism, and PCOS may lead to further biochemical testing.
Investigations for Obesity Assessment
To identify metabolic problems and tailor therapy, diagnostic tests are commonly ordered at the initial stage of obesity evaluation. A baseline evaluation of glycated hemoglobin (HbA1c) or fasting blood glucose, electrolytes and renal function tests (creatinine, estimated glomerular filtration rate [eGFR]), lipid profile (total cholesterol [TC], low-density lipoprotein cholesterol [LDL-C], high-density lipoprotein cholesterol [HDL-C], and triglycerides [TGs]), alanine aminotransferase (ALT), as well as age-appropriate cancer screening are recommended by the Canadian guidelines in most patients.
Patients at high risk of MASLD should also be screened by abdominal ultrasonography, and/or other noninvasive scoring tools such as the Fibrosis-4 Index. It may be appropriate to refer patients with abnormal scores to a gastroenterology or hepatology specialist. If clinically indicated, complete blood count (CBC) and the measurement of thyroid-stimulating hormone (TSH), ferritin, and vitamin B12 and vitamin D levels may be warranted.
In women with obesity and symptoms of PCOS (menstrual irregularities, possible androgen excess), luteinizing hormone (LH), follicle-stimulating hormone (FSH), total testosterone, dehydroepiandrosterone sulfate (DHEAS), prolactin, TSH, and 17-hydroxyprogesterone levels should be measured.
A 1-mg overnight dexamethasone suppression test is recommended in patients with a clinical suspicion of Cushing syndrome.
ComplicationsTop
The effects of obesity on the health of a person are heterogeneous in both presentation and severity due to individual differences in body composition, body fat distribution, and function. Obesity increases the risk of developing a number of complications:
1) Metabolic complications can include type 2 diabetes, hyperlipidemia, nutritional deficiency (eg, protein, vitamin D, and iron deficiency), gout, hypertension, PCOS, hypogonadism, infertility, cardiovascular disease, gastrointestinal disease, MASLD, cancer, and skin problems. A defective insulin signal and chronic tissue inflammation due to increased macrophage infiltration into adipose tissue are thought to be the 2 key mechanisms linking obesity and cardiometabolic risk.
Obesity is an independent predictor of coronary artery disease, with a stronger relationship in younger individuals. Cardiovascular complications associated with obesity are related to overall body fat mass but also largely dependent on individual differences in regional body fat distribution. Excess visceral (abdominal) adipose tissue has been identified as a strong predictor in the development of cardiovascular disease over time, independent of total body fat mass.
Some authors postulate that 20% of all cancers are related to obesity, with higher risk of colon, kidney, pancreatic, and esophageal cancer in both sexes and endometrial and postmenopausal breast cancer in women. The higher risk of many forms of cancer is linked to adiposity through the release of growth factors and inflammatory adipokines.
2) Mechanical complications include osteoarthritis, gout, sleep apnea, plantar fasciitis, gastroesophageal reflux, urinary incontinence, intertrigo, thrombosis, and idiopathic intracranial hypertension (IIH). IIH has a strong association with obesity, although the exact pathophysiology is unclear. Possible mechanisms include raised intra-abdominal pressure with increasing cardiac filling pressure and impeding venous return from the brain.
Individuals with obesity are challenged with activities of daily living and spend a considerable amount of time on activities such as dressing, bathing, meal preparation, and medical appointments.
3) Mental health complications: Mood or anxiety disorders, addiction, internalized weight bias, self-image, expectations, sleep, attention, personality, and knowledge/cognition may all be associated with or affected by obesity. Physical conditions and functional limitations (osteoarthritis, avoidance of physical activity due to pain and discomfort) are contributing factors.
4) Monetary health/“milieu” complications: Obesity and obesity-related complications may be correlated with socioeconomic status, education, and food insecurity. Stigma and weight bias limit access to weight loss programs as well as pharmacotherapy, surgery, and vitamins. Obesity may have a negative effect on health, quality of life, and likely leads to reduced life expectancy, which, depending on the excess weight, can be lowered by 2 to 10 years, primarily due to cardiovascular disease.Evidence 1Moderate Quality of Evidence (moderate confidence that we know true effects of the intervention). Quality of Evidence lowered due to the observational nature of data. Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009 Mar 28;373(9669):1083-96. doi: 10.1016/S0140-6736(09)60318-4. Epub 2009 Mar 18. PMID: 19299006; PMCID: PMC2662372.
Obesity is a stigmatized disease, with the general public and health care professionals often responding negatively to people with overweight. Beliefs about personal irresponsibility and lack of will power as well as casting blame and shame on individuals with obesity are reinforced by the cultural narrative about obesity, which results in higher anxiety and depression, economic inequities (eg, education and employment), avoidance of health care professionals, unfair treatment received in the health care system, and social inequalities.
Tables and FiguresTop
|
Drug class |
Drugs associated with weight gain |
Alternatives (associated with weight loss or weight neutral) |
|
Antihistamine agents |
Diphenhydramine |
Oxymetazoline |
|
Antihyperglycemic agents |
Insulin, TZDs, sulfonylureas, meglitinides |
Metformin, GLP-1 analogues, DPP-4 inhibitors, SGLT-2 inhibitors, acarbose |
|
Contraceptives |
Depo-medroxyprogesterone |
Oral contraception, barrier methods |
|
Antidepressants |
– MAOIs: Phenelzine – TCAs: Amitriptyline, nortriptyline, imipramine – SSRIs/SNRIs: Paroxetine, citalopram, escitalopram, sertraline – Atypical: Mirtazapine |
Trazodone, nefazodone, duloxetine, venlafaxine, desvenlafaxine, fluvoxamine (variable weight effect), bupropion
|
|
Antihypertensive agents |
– Atenolol, metoprolol, propranolol – Diltiazem – Central alpha agonists: Clonidine |
– Diuretics – ACEIs/ARBs – Amlodipine, felodipine, nifedipine |
|
Antipsychotic agents, neuroleptic agents, mood stabilizers |
Clozapine, olanzapine, quetiapine, haloperidol, perphenazine, risperidone, lithium |
Lamotrigine, aripiprazole, ziprasidone |
|
Glucocorticoids |
Prednisone, dexamethasone, prednisolone (in higher than physiologic doses) |
Budesonide, NSAIDs |
|
Anticonvulsant agents |
Valproic acid, gabapentin, carbamazepine |
Lamotrigine, topiramate, phenytoin, levetiracetam |
|
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; DPP-4, dipeptidyl peptidase 4; GLP-1, glucagon-like peptide 1; MAOI, monoamine oxidase inhibitor; NSAID, nonsteroidal anti-inflammatory drug; SGLT-2, sodium-glucose cotransporter 2; SNRI, serotonin-norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant; TZD, thiazolidinedione. | ||
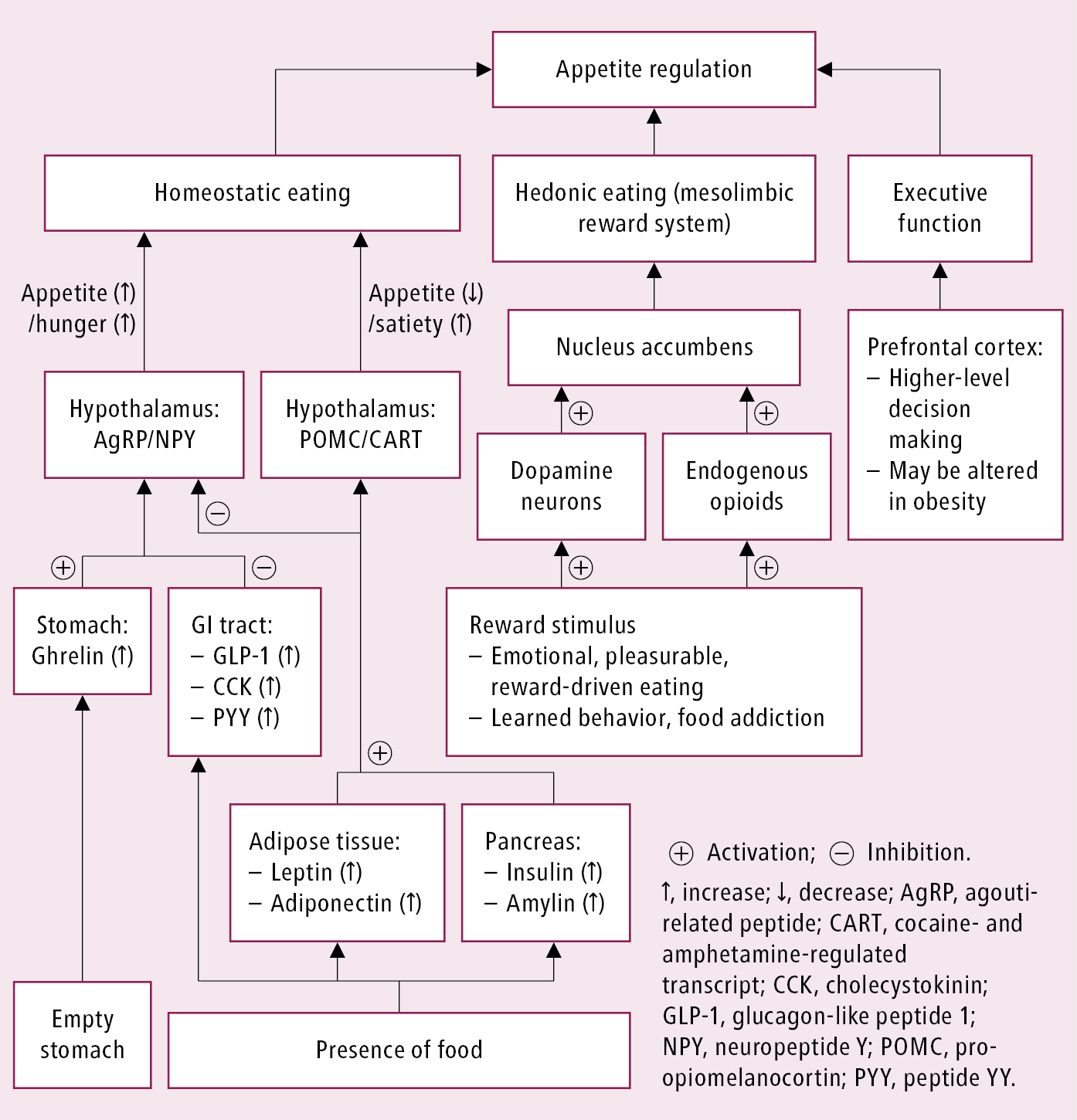
Figure 6.5-1. Appetite regulation in the brain.