DefinitionTop
Work-related asthma is asthma caused or exacerbated by work-related factors. Several terms are used to define the multiple forms of this condition. Occupational asthma begins in adulthood and is induced by or causally related to specific immunologic or nonimmunologic stimuli in the work environment. Work-exacerbated asthma occurs in patients with a preexisting or concurrent diagnosis of asthma that worsens in the workplace. Irritant-induced asthma results from single or multiple exposures to a nonimmunologic irritant at a high level of intensity. Reactive airways dysfunction syndrome (RADS) is the acute form of irritant-induced asthma, which may be triggered even by a single high-intensity exposure.
Etiology and PathomechanismTop
1) Allergic (asthma caused by agents [allergens] with high or low molecular weight: see Table 17.13-1).
2) Nonallergic (asthma caused by irritants, with an acute onset [RADS] or subacute onset, and resulting from exposure to chemical irritants, occurring in high concentrations exceeding acceptable standards few folds).
Clinical FeaturesTop
Similar to other asthma phenotypes (see Asthma).
DiagnosisTop
Criteria for the diagnosis of the occupational etiology of asthma:
1) Onset of the disease in the period of exposure to the etiologic factor of occupational asthma.
2) Significant reversibility of bronchial obstruction or bronchial hyperresponsiveness during exposure to the etiologic factor of occupational asthma; a 4-fold increase in PC20 in the period without exposure to occupational factors (nonwork period), compared with PC20 in the period of work supports the diagnosis.
3) Confirmation of the cause-and-effect relationship between occupational exposure and the disease, determined on the basis of:
a) Identification of specific IgE (skin prick tests or specific serum IgE).
b) Serial measurements of peak expiratory flow (PEF) at the workplace and outside of it (for ≥3 weeks, ≥4 times/d) and information on the severity of symptoms and consumption of rescue medication during PEF monitoring. Documenting PEF worsening during work (preferably ≥2 weeks), compared with the off-work period (preferably ≥10 days), confirms the relationship between worsening asthma and work.
c) Inhalation challenge tests with the allergen.
d) An increase in the percentage of eosinophils in induced sputum in patients during their working life compared with the period outside work.
Diagnostic algorithm: see Figure 17.13-1.
Criteria for the diagnosis of irritant-induced occupational asthma:
1) Exposure to ≥1 irritant in concentrations significantly exceeding acceptable standards.
2) Onset of asthma symptoms within 24 hours of exposure.
3) Symptoms of asthma for ≥3 months after exposure.
4) Pulmonary function tests confirm the reversibility of obstruction or bronchial hyperresponsiveness.
5) Other lung diseases were excluded.
Asthma exacerbated by occupational factors can be diagnosed in patients with a low probability of occupational asthma who have shown a relationship between exposure to the work environment factors and deterioration of disease control.
TreatmentTop
For patients who are diagnosed with occupational asthma induced by a sensitizing agent, prompt and complete removal of the worker from further ongoing exposure is essential. Progression should be expected if ongoing exposure persists. Engineering controls and personal protective equipment (PPE) can be considered in the offending workplace only in the setting of mild disease when the patient has a strong preference for maintaining their current position. Regulatory workplace safety board should be notified in the event that other workers may also be affected. Use medical therapy as in nonoccupational asthma: Asthma.
Tables and FiguresTop
|
Etiologic agents |
Exposed occupational groups |
|
High-molecular-weight agents (>5 kDa) | |
|
Flour and flour contaminants |
Bakers, pastry cooks, millers, flour transport workers |
|
Animal allergens |
Farmers, animal breeders, employees of laboratory animal quarters and zoos, animal traders, veterinarians |
|
Plant proteins |
Greenhouse employees, farmers |
|
Fungal spores |
Farmers, persons working in moist environment, workers in the food industry, art restorers |
|
Resins (particularly rosin) |
Employees of electronic plants (especially solderers), string players |
|
Natural rubber latex |
Health-care personnel, people employed in the production of rubber items, people wearing latex gloves at work |
|
Oilseeds |
Vegetable oil producers |
|
Wood dusts |
Employees of the woodworking and furniture sector |
|
Detergents, enzymes |
Employees of washing powder and detergent production plants, laundry workers, employees of the food sector |
|
Low-molecular-weight agents (≤5 kDa) | |
|
Diisocyanates |
Polyurethane producers, persons using polyurethanes in production processes (furniture production, shoemaking, production of gaskets, floor coverings), car painters, persons employed in the production of plastics, persons working with sealants in the building industry |
|
Metals and metal salts (platinum, nickel, chrome, cobalt) |
Persons employed in chemical industry, those involved in metal refining, those working in galvanizing plants, in leather processing, in the production of knives and medical instruments, welders, construction workers |
|
Dyes |
Dye producers, persons who use dyes (furniture and textile industry) |
|
Persulfates, henna |
Hairdressers |
|
Disinfectants |
Health-care personnel, those employed in agriculture, fishing industry, and chemical and pulp and paper industries |
|
Acid anhydrides |
Persons employed in the chemical sector in the production of dyes and polyester and formaldehyde resins, plastic processing, pharmaceutical production, manufacturing of insecticides, steel industry |
|
Amines and acrylic compounds (adhesives, varnish primers, bone void fillers, dentures and bridges) |
Construction workers, dental technicians, nurses and dental assistants, dentists, orthopedists, model makers |
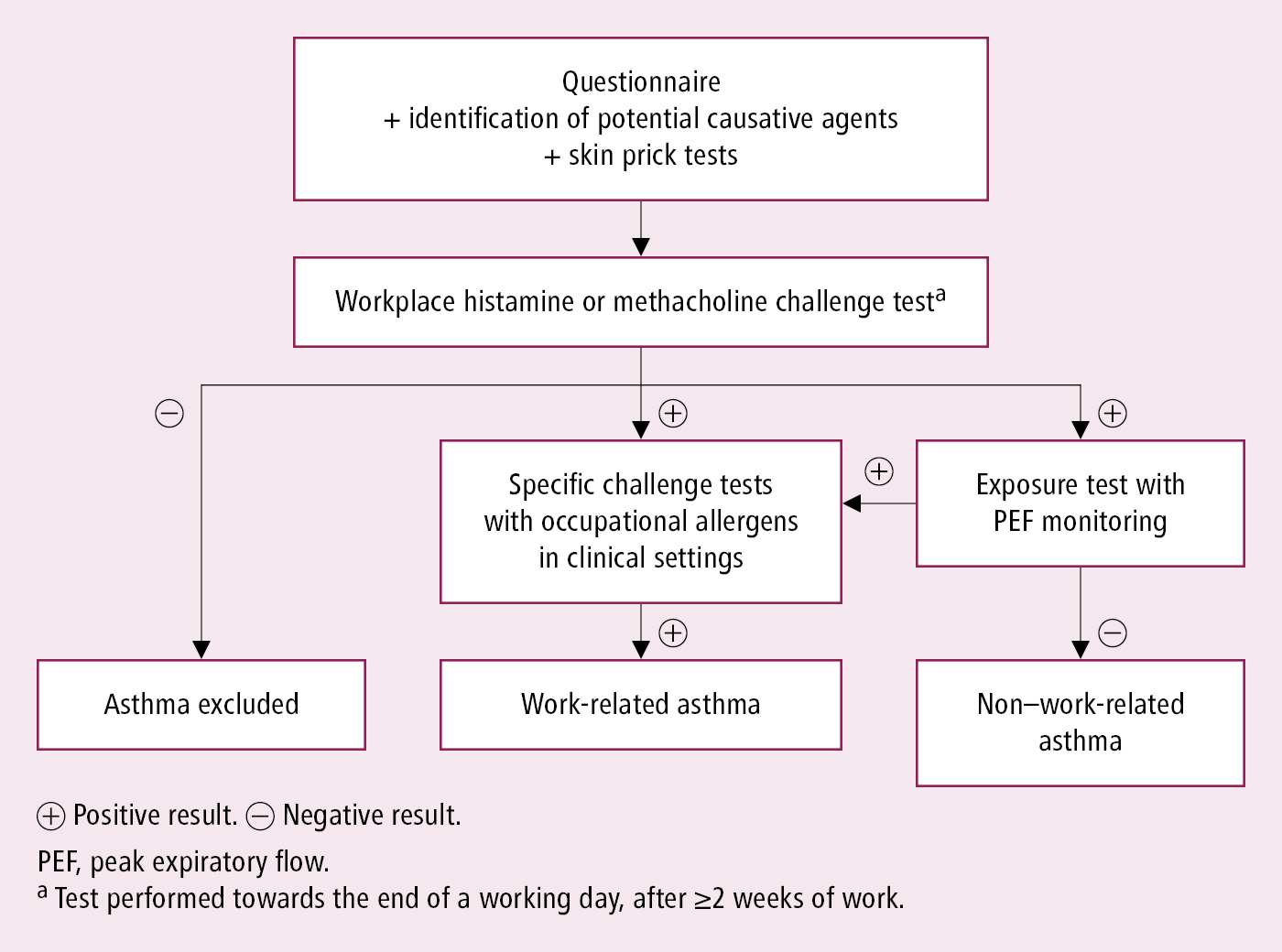
Figure 17.13-1.
Diagnostic workup of work-related asthma.