Arthrocentesis refers to the aspiration of fluid from a joint cavity.
IndicationsTop
1. Diagnostic: Arthrocentesis is a useful tool in diagnosing causes of joint effusion and can therefore guide therapy. Potential etiologies include septic arthritis, hemarthrosis, crystal arthropathies, inflammatory arthropathies, and noninflammatory arthropathies.
2. Therapeutic: Decompression of joint effusion for pain relief, reducing septic burden in septic arthritis, and aspiration followed by intra-articular glucocorticoid administration for osteoarthritis and inflammatory arthritides.
ContraindicationsTop
1. Absolute: Uncontrolled coagulopathy, superimposing skin or soft-tissue infection at the planned injection site.
2. Relative: Anticoagulation (especially with international normalized ratio [INR] >3.0, activated partial thromboplastin time [aPTT] >2 × upper limit of normal), thrombocytopenia (platelet count <50,000/microL), and infection in adjacent tissues.
The presence of a prosthetic joint is generally considered a contraindication to aspiration or injection, unless aspiration for suspected infection is required.
Potential ComplicationsTop
Septic arthritis, hemarthrosis, hematoma, joint cartilage injury, pain at the puncture site, adverse effects of local anesthetics or drugs administered intra-articularly (eg, glucocorticoids).
EquipmentTop
1. Sterilizing solution.
2. Needles (we suggest 22-gauge 1 1/2-inch needles for most large joints and 25-gauge 5/8-inch needles for small joints [metacarpophalangeal, proximal interphalangeal, distal interphalangeal]).
3. Local anesthetic (see Infiltration Anesthesia; skilled clinicians may skip this).
4. Sterile syringes for aspirate collection.
5. Dressing supplies.
Patient PreparationTop
Obtain informed consent. Explain the risks and benefits of arthrocentesis.
ProcedureTop
Online video demonstrations available at www.RheumTutor.com.
1. Knee: Medial approach (Figure 21.2-1):
1) The patient is lying supine with the knee extended.
2) Palpate the medial parapatellar fossa, halfway between the superior and inferior poles of the patella. Place a mark in the soft spot, anticipating that the tip of the needle will be under the patella when it is advanced (a retracted pen is useful for impressing a mark).
3) Apply sterilizing solution in a circular fashion, starting at the injection site and moving outwards. Do not bring the swab back to the middle. Repeat 2 to 3 times (or more if needed).
4) Local anesthetic may be infiltrated using a small-bore needle (eg, 25 gauge), especially if a difficult or long procedure (large volume effusion) is anticipated (see Infiltration Anesthesia). Skilled clinicians may skip this, as the discomfort of the actual procedure may be less than or equal to the pain of local anesthetic infiltration.
5) With the syringe/needle (eg, 22 gauge) held fairly horizontally, advance the needle aiming laterally. Once the needle is within subcutaneous tissue, withdraw the plunger a little to create negative syringe pressure as the needle is advanced. A “give” may be felt as the needle tip breaches the joint capsule or fluid may start flowing (if this does not happen, one should estimate the depth for the needle tip to be under the body of the patella). Aspirate as much fluid as possible, switching syringes as needed while keeping the needle in place. Medication can be administered through the same needle if needed.
2. Knee: Lateral approach (Figure 21.2-1):
1) The patient is supine with the knee extended.
2) Palpate the lateral parapatellar groove under the superior 1/3 of the patella. Make an impression in the soft spot to mark the entry point.
3) Cleaning and local anesthetic use are as in the medial approach (see above).
4) Follow other instructions as in the medial approach, advancing the syringe/needle (eg, 22 gauge) horizontally and aiming inferomedially (targeting the underside of the middle 1/3 of the patella).
3. Wrist (Figure 21.2-2):
1) The patient is sitting or lying, with the forearm/hand prone and wrist slightly flexed (this can be achieved with a small rolled towel placed under the wrist).
2) Palpate distally along the middle of the wrist, just past Lister tubercle, and a soft spot in the radiocarpal joint space should be felt. Make an impression with a retracted pen.
3) Cleaning and local anesthetic use: see above.
4) With the syringe/needle (5/8-inch or 1-inch needle is usually sufficient) held fairly vertically, advance the needle downwards into the joint space. Once the capsule is breached, fluid may be aspirated. Intra-articular medications can be then administered if needed.
4. Ankle (Figure 21.2-3):
1) The patient is lying supine with the knee extended and the ankle in a neutral position.
2) Palpate distally along the anteromedial aspect of the tibia until the soft spot between the tibia and the talus is found. This should be medial to the tibialis anterior tendon. Make an impression to mark the site of injection.
3) Cleaning and local anesthetic use: see above.
4) With the syringe/needle (1-inch or 1 1/2-inch) held almost parallel to the sole of the foot, advance the needle aiming posteriorly and slightly laterally (imagine the middle of the joint) until the capsule is breached or the needle encounters the articular surface (in which case you should withdraw slightly). Apply negative pressure. Once the joint capsule is breached, fluid can be aspirated. Intra-articular medications can be administered through the same needle as needed.
FiguresTop
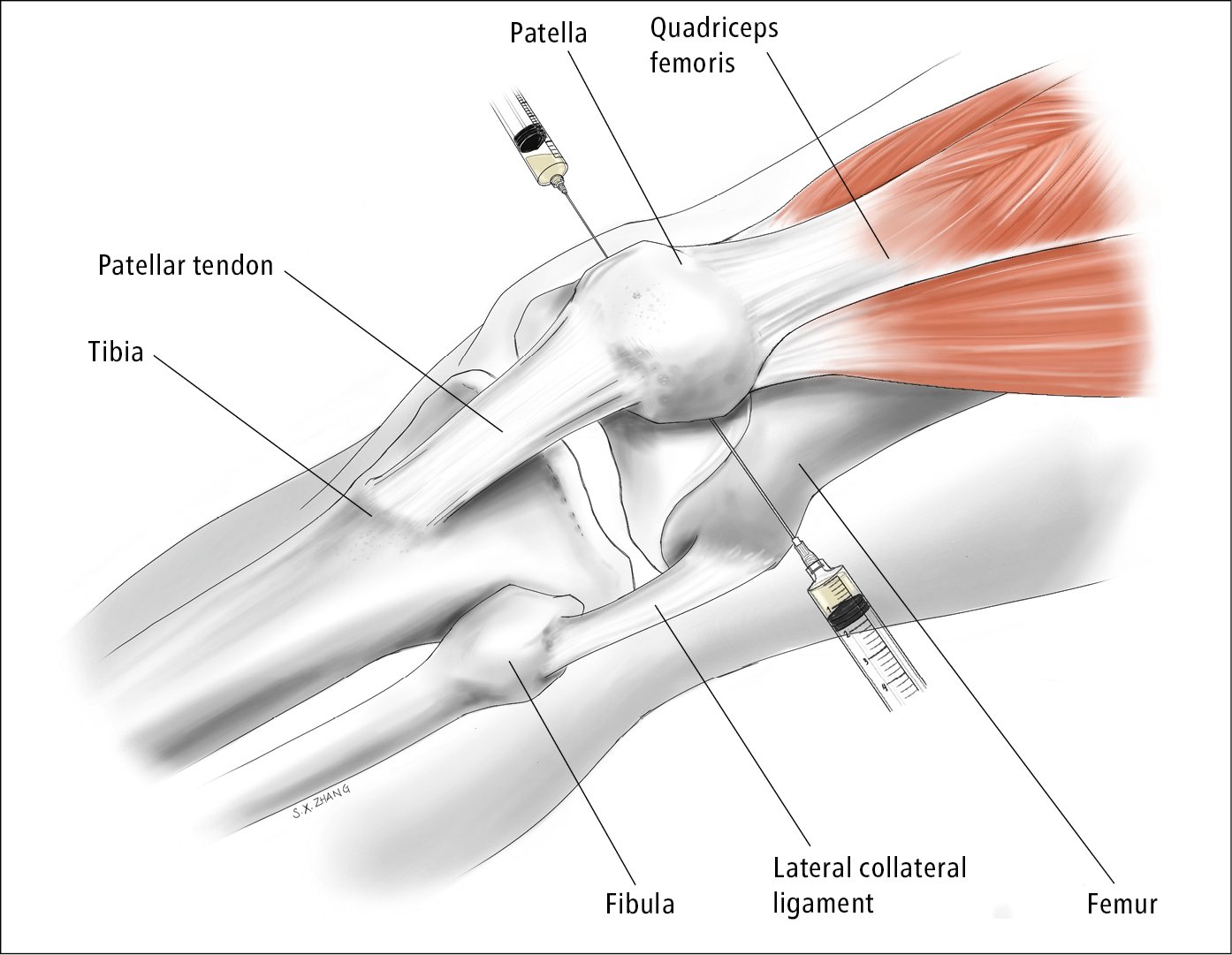
Figure 21.2-1. Knee arthrocentesis. Needle entry: medial approach underneath the mid-point of the patella; lateral approach underneath the upper 1/3 of the patella. Illustration courtesy of Dr Shannon Zhang.
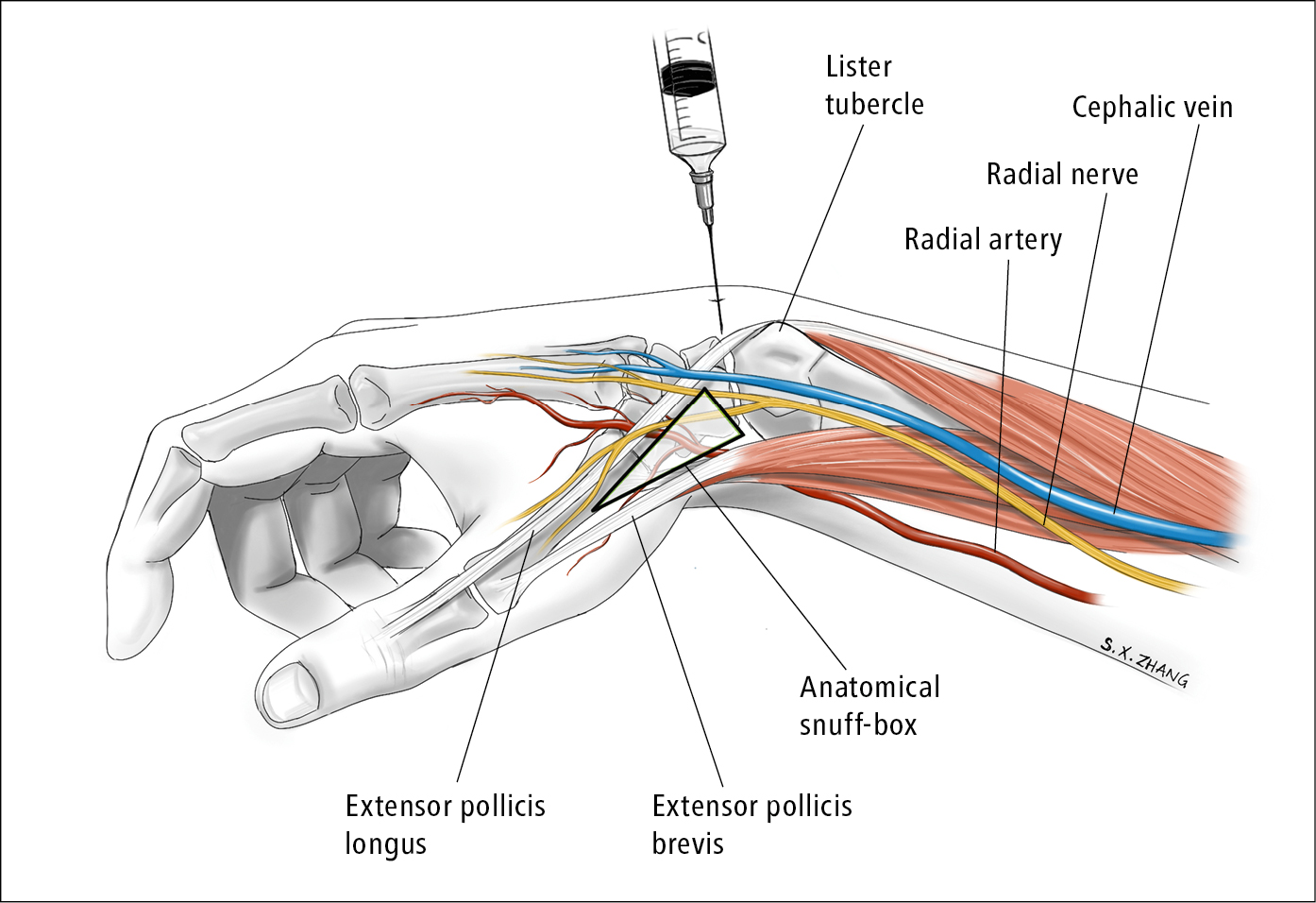
Figure 21.2-2. Wrist arthrocentesis. Illustration courtesy of Dr Shannon Zhang.
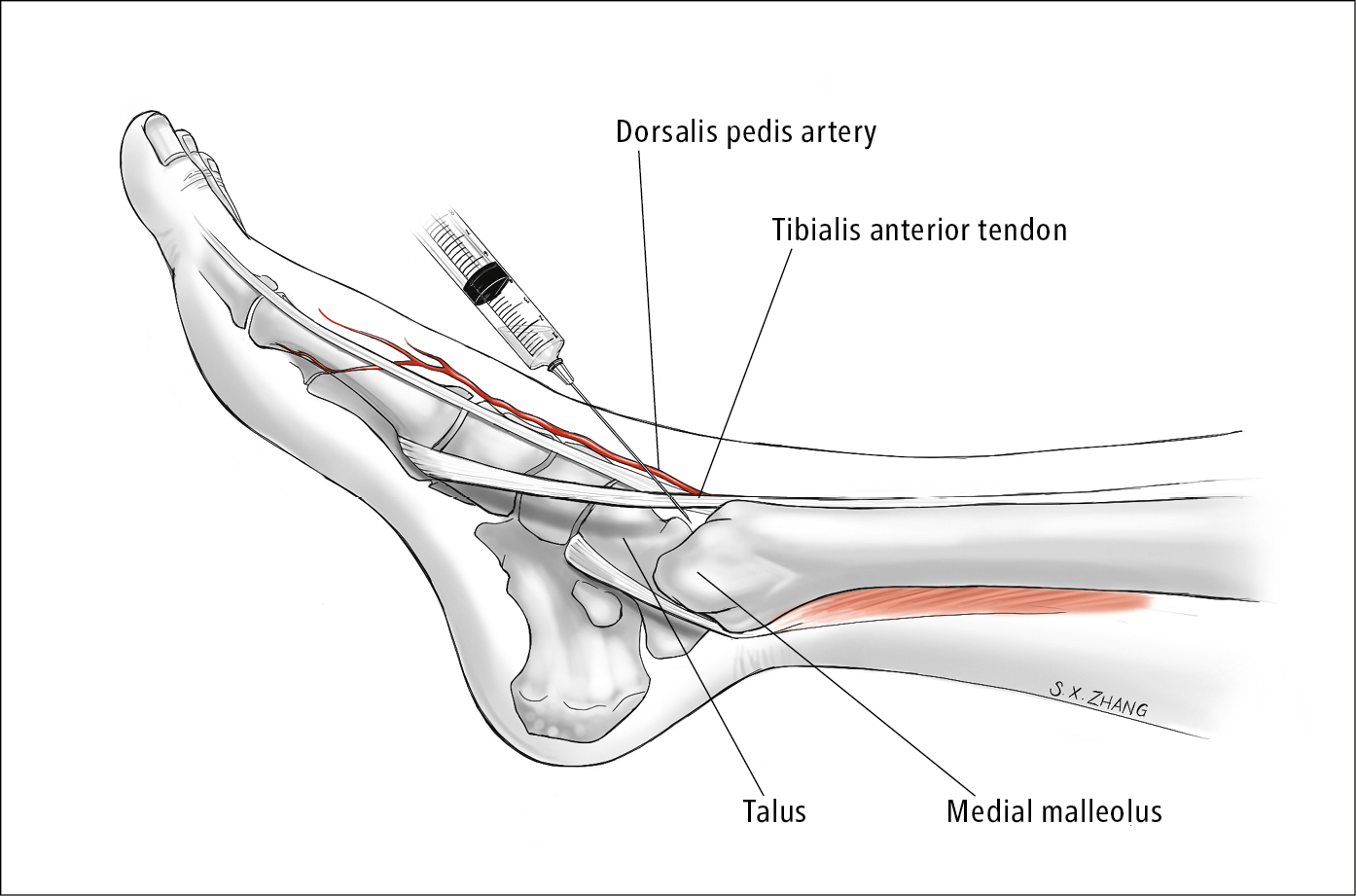
Figure 21.2-3. Ankle arthrocentesis. Illustration courtesy of Dr Shannon Zhang.