The use of noninvasive ventilation (NIV) in the acute setting requires careful supervision, as treatment failure can happen quickly and requires emergent intubation and invasive mechanical ventilation (IMV). Medical personnel must be familiar with resuscitation procedures and be able to quickly respond to changes in the patient’s status. In this section we also describe continuous positive airway pressure (CPAP), which—although technically not a ventilation modality—is often delivered using the same ventilator and interface as NIV.
IndicationsTop
1. Acute NIV: Most often used in acute hypoxic or hypercapnic respiratory failure in patients who do not have indications for immediate intubation and who do not respond or are unlikely to fully respond to standard pharmacologic treatment, oxygen therapy, and pulmonary rehabilitation. The most common indications for acute NIV include:
1) Exacerbations of chronic obstructive pulmonary disease (COPD) with hypercapnia (consider with arterial blood pH <7.35 and partial pressure of carbon dioxide [PaCO2] >45-49 mm Hg; these are approximations requiring continuous clinical correlation): Even in patients anticipated to require intubation, NIV should be trialed as intubation is arranged, because some patients may improve and avoid intubation altogether.Evidence 1Strong recommendation (benefits clearly outweigh downsides; right action for all or almost all patients). High Quality of Evidence (high certainty that we know the true effect of the intervention). Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017 Aug 31;50(2):1602426. doi: 10.1183/13993003.02426-2016. Print 2017 Aug. PMID: 28860265.
2) Cardiogenic pulmonary edema: Via positive intrathoracic pressure, NIV and CPAP reduce preload and afterload, thus exerting beneficial hemodynamic effects in addition to improving oxygenation in patients with cardiogenic pulmonary edema.Evidence 2Strong recommendation (benefits outweigh downsides; right action for all or almost all patients). Moderate Quality of Evidence (moderate certainty that we know the true effect of the intervention). Quality of Evidence lowered due to risk of bias, as some trials stopped early for potential harm. Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017 Aug 31;50(2):1602426. doi: 10.1183/13993003.02426-2016. Print 2017 Aug. PMID: 28860265.
3) Exacerbations of chronic disease causing hypercapnia, particularly chest deformity (eg, kyphoscoliosis) and neuromuscular disorders or obesity hypoventilation syndrome.
As noted above, NIV is also used as an adjunct during withdrawal of mechanical ventilation as a method to reduce extubation failure.
2. Chronic NIV (including home NIV):
1) Neuromuscular diseases, including amyotrophic lateral sclerosis (ALS).
2) Chest deformities causing respiratory failure (eg, advanced kyphoscoliosis).
3) Obesity hypoventilation syndrome.
4) COPD with significant hypercapnia, persisting despite optimization of treatment.
Application of NIV and CPAP in breathing disorders during sleep: see Sleep-Related Breathing Disorders.
ContraindicationsTop
1. Apnea: While NIV can supply a ventilatory rate, in most cases complete apnea suggests that intubation and IMV are likely required.
2. Lack of cooperation: NIV requires patients to keep the NIV interface in place. Some patients may have claustrophobia or dyspnea, which precludes successful use of NIV. Low-dose sedation may be helpful in facilitating NIV tolerance.
3. Significant disturbances of consciousness are generally an indication for intubation and initiation of IMV. The exception would be patients with a rapidly reversible cause of decline, such as those for whom the presumed cause of altered level of consciousness is hypercapnia from an acute COPD exacerbation. In such cases the patient requires very close monitoring with frequent reassessment by an experienced clinician who can definitively manage the patient’s airway in the event NIV is unsuccessful.
4. Severe hemodynamic instability: Severe shock is generally an indication for IMV.
5. Airway obstruction or presence of large amounts of mucus in the bronchial tree, requiring frequent suctioning, as NIV impedes secretion clearance.
6. Risk of aspiration of gastric contents or situations posing such a risk, for example, ongoing vomiting, large-volume gastrointestinal (GI) bleeding, recent surgery of the upper GI or respiratory tract.
7. Craniofacial deformities and skin lesions that prevent a tight fit of the mask.
8. Untreated or uncontrolled pneumothorax, as positive pressure may worsen the disease.
Techniques and PrinciplesTop
In contrast to IMV, which is delivered through either an endotracheal tube (ETT) or tracheostomy tube, NIV and CPAP can be delivered through many interfaces, including oral, nasal, oronasal, or full facial masks; a full-head helmet; or a harness securing the mask to the patient’s head (Figure 21.15-1). In acute indications an oronasal mask is frequently used, although helmet interfaces are increasingly common and may be preferred in acute respiratory failure.Evidence 3Conditional recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Low Quality of Evidence (low certainty that we know the true effect of the intervention). Quality of Evidence lowered due to very serious imprecision. Chaudhuri D, Jinah R, Burns KE, et al. Helmet noninvasive ventilation compared to facemask noninvasive ventilation and high-flow nasal cannula in acute respiratory failure: a systematic review and meta-analysis. European Respiratory Journal. 2022 Mar 1;59(3).
1. CPAP provides constant positive airway pressure, which facilitates recruitment of alveoli, thereby improving gas exchange in the lungs; reduces preload and afterload (of particular importance in pulmonary edema); and reduces the respiratory effort needed in patients with bronchial obstruction by matching airway pressures to the auto–positive end-expiratory pressure (PEEP) distal to the obstruction site (see Invasive Mechanical Ventilation). Its primary use in the acute setting is for congestive heart failure.
2. NIV: While many ventilatory modes are theoretically possible during bilevel NIV, the assist-control (AC) mode is almost exclusively used. As with the AC mode in IMV, the ventilator provides fully supportive breaths at a set rate, but if the patient’s inspiratory efforts trigger a breath, these are supported by the ventilator. A purely spontaneous ventilation mode, such as pressure support ventilation (PSV), may also be used, but it depends on the patient having an adequate respiratory drive.
In addition to the respiratory rate, the clinician sets the inspiratory positive airway pressure (IPAP) and the expiratory positive airway pressure (EPAP). Due to the lack of a definitive airway and the increasing risk of air leaks, the maximum values for EPAP are ~10 to 12 cm H2O and for IPAP, ~20 to 24 cm H2O. Beyond this level many patients do not tolerate NIV and there is an increasing risk of gastric insufflation, which could lead to vomiting and aspiration.
The greater the difference between these pressures (IPAP-EPAP, ie, the drive pressure), the greater the tidal volume (Vt) generated. In patients with or at risk of hypercapnia (eg, in COPD), it is preferable to keep the IPAP-EPAP gradient high to facilitate ventilation. Higher IPAP and EPAP levels also result in higher mean airway pressure compared with CPAP, and thus may improve oxygenation. In addition to the IPAP and EPAP values, other settings are based on the selected mode but are generally similar to those used during IMV.
For patients requiring NIV for a short time only, the device can be provided without humidification, but in patients who are going to use the device longer than a few hours a heated humidifier is often used to increase patient comfort.
NIV is generally delivered in a sitting or semirecumbent position. To encourage tolerance of the device, it is important to explain the interface and purpose of the treatment to the patient before initiation and to let them know that the positive pressure may initially feel uncomfortable. The patient should be encouraged to breathe evenly and calmly.
Ventilation is usually started with an EPAP of 3 to 4 cm H2O (in practice this is the lowest pressure that can be set in individual models) and an IPAP of 10 cm H2O in order to get the patient accustomed to NIV. The pressure is then gradually increased by 2 to 3 cm H2O to the target values every few minutes. In general, the minute ventilation may be further affected by the difference between IPAP and EPAP as well as inspiratory time and oxygenation by FiO2 and EPAP. The patient’s condition should be closely monitored (clinically for respiratory rate and respiratory effort as well as through oximetry and arterial or venous blood gas analysis) and, in the event of worsening, intubation and mechanical ventilation should not be delayed. The first hour of NIV is crucial, as the NIV failure rate is highest during this time, and in most indications for NIV (COPD, congestive heart failure) patients generally respond rapidly to treatment. In significantly agitated patients for whom tolerance is a challenge, administration of a very low dose of a sedative drug (eg, IV midazolam) may be considered, but this requires very close monitoring in an appropriate setting to avoid or at least detect early excessive suppression of respiratory efforts.
After an initial trial of NIV, many patients will require a break for comfort, oral hygiene, or nutritional support. Nasal high-flow therapy may be preferred over conventional oxygen therapy during such breaks.Evidence 4Conditional recommendation (benefits likely outweigh downsides, but the balance is close or uncertain; an alternative course of action may be better for some patients). Low Quality of Evidence (low certainty that we know the true effect of the intervention). Quality of Evidence lowered for very serious imprecision. Oczkowski S, Ergan B, Bos L, et al. ERS Clinical Practice Guidelines: High-flow nasal cannula in acute respiratory failure. Eur Respir J. 2022 Apr 14;59(4):2101574. doi: 10.1183/13993003.01574-2021. Print 2022 Apr. PMID: 34649974.
ComplicationsTop
Complications are usually local and caused by the mask (pressure ulcers and abrasions on the nose and other parts of the face, rhinitis, nasal congestion) or air leakage (conjunctivitis). Hypotension and pulmonary barotrauma (rarely) as well as gastric distension may also occur. Nutrition may be compromised, as many NIV interfaces prevent reliable enteral access.
FiguresTop
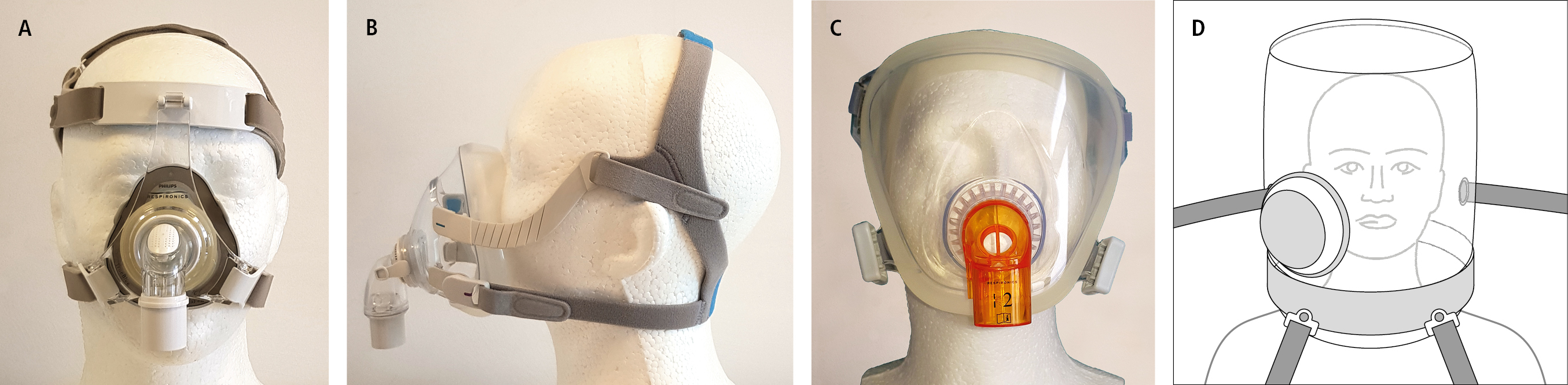
Figure 21.15-1. Masks used for noninvasive ventilation. A, nasal; B, naso-oral; C, full face (courtesy of Dr Tadeusz Przybyłowski); D, helmet.