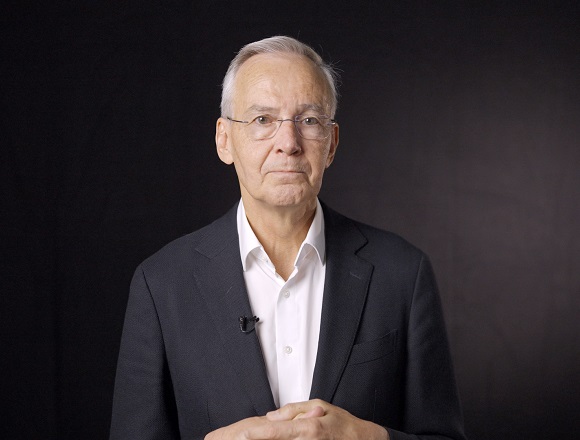
Jan Václavík, MD, PhD, is a professor of medicine and head of the Department of Internal Medicine and Cardiology at the University Hospital Ostrava, Czech Republic. He takes a special interest in arterial hypertension, multimorbidity, and cardiovascular pharmacotherapy.
Patients receive prescriptions from numerous clinicians over the years and eventually end up on several drugs, with the original rationale being frequently forgotten. How to practically achieve deprescribing?
Jan Václavík, MD, PhD: It is important to think that we should be deprescribing in the first place. Then, we always have to look at all the disorders and diagnoses the patient has and look for all the medications the patient is using, including prescription drugs, over-the-counter drugs, and other drugs. And after that, we have to have a look if all the drugs are really indicated in the patient’s age group, risk factors, and illnesses, and then we can use those systems for deprescribing, like the Screening Tool of Older People’s Prescriptions (STOPP) and Screening Tool to Alert to the Right Treatment (START) criteria, or Beers Criteria, or others.
Basically, we identify all medications that are no longer indicated, that can cause side effects or some problems to the patients, or that are not advisable in that age group, and discuss with the patient that we would like to withdraw the drugs. And my experience is that patients really welcome every [attempt] when we try to reduce the medication burden, and they’re really helpful in the process. But we also have to communicate with other health care professionals, so they know about the changes we made and the reasons we made them.
Lastly, we always have to recheck and rereview the medications on the next encounters with the patient and assess whether there were no withdrawal reactions and whether everything is going fine; and reassess the medications again.
 English
English
 Español
Español
 українська
українська