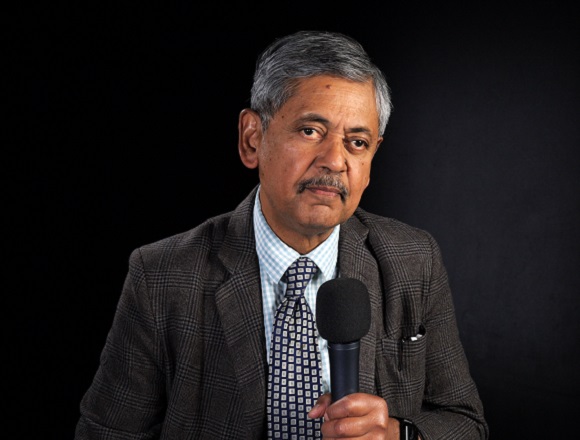
Sharon Kolasinski, MD, is a professor of clinical medicine in the Division of Rheumatology at the University of Pennsylvania, USA. As Chief of the Division of Rheumatology at Penn Presbyterian Medical Center and Director for Rheumatology at the Penn Musculoskeletal Center, she is responsible for coordination of inpatient and outpatient rheumatology services.
What’s the role of vitamin D supplementation in osteoarthritis?
Vitamin D supplementation is very interesting because there’s a broad array of investigations that have suggested that vitamin D supplementation should be a good thing in osteoarthritis. First, we know vitamin D is important in bone health. That’s adjacent tissue to the joint, so we know that it might have some implications. But in addition, more recently we’ve found that vitamin D receptors are present on chondrocytes. That’s interesting because we know that cartilage loss is the hallmark of osteoarthritis. If vitamin D receptors are on chondrocytes, maybe we have the opportunity to intervene by giving vitamin D. The question would be, though, what is vitamin D doing to chondrocytes? We don’t completely know.
Some say that they think it is related to proteoglycan synthesis, that it could amp up proteoglycan synthesis. That would be a good thing. Others have hypothesized that vitamin D could be involved in autophagy. Autophagy is the subcellular mechanism for keeping cells going, cleaning up degraded products, and helping the cells live longer and not die. That would be good, too, if vitamin D influenced autophagy, so the chondrocytes would live longer. Since they don’t replicate very well, it would be nice to have them living longer. So, that’s an interesting possibility as well. We think, mechanistically vitamin D might be helpful in osteoarthritis.
When we look at human studies, there’s quite a bit of variability across the board. In short-term studies, vitamin D supplementation at quite high doses over short periods of time has not been consistently associated with a lot of positive outcomes. The one that is most consistent is an improvement in knee pain. Several studies have suggested that knee pain can be improved by short-term vitamin D supplementation in doses ranging from 400 IU/d for, say, 2 to 3 months to doses of 50,000 IU/wk for a couple of months. So, we don’t really understand much about the appropriate dose of vitamin D that might actually lead to knee pain [relief]. But I’d say that other clinical investigations in humans have not found vitamin D to be helpful in knee pain modulation. There are 2 studies that are worth noting. The Framingham study looked epidemiologically in an observational way at vitamin D intake in patients over a several-year period and really found no correlates to structural change in osteoarthritis. So, if vitamin D was actually amping up the cartilage development or preservation, you would have hoped to have some radiographic end points at the end of a couple of years. They didn’t find any. And Tim McAlindon’s group at Tufts also looked at an interventional trial over 2 years, and they, too, were unable to find any structural changes or structural preservation associated with vitamin D supplementation.
So, there are reasons to believe that vitamin D might be helpful in some patients, but the data have been mixed. For the present, the recommendation is to check the vitamin D level in all of our patients as part of the assessment of their bone health. If vitamin D levels are low, it makes sense to supplement, and most patients benefit from 400 IU minimum per day. I would say a lot of folks are supplementing ~1000 IU to 2000 IU/d, and there is some variability in how well any given supplement dose will alleviate vitamin D deficiency. For those who are vitamin D deficient, it’s reasonable to supplement with vitamin D for overall bone and cartilage health, but as a specific intervention for osteoarthritis, the data are not there yet to support blanket recommendations for vitamin D supplementation.
 English
English
 Español
Español
 українська
українська