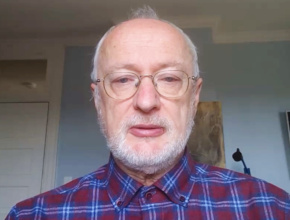
Dr Miłosz Parczewski, professor of medicine, head of the Department of Infectious Diseases, Tropical Diseases, and Acquired Immunodeficiency at Pomeranian Medical University, and head of the Polish Scientific AIDS Society, joins Dr Roman Jaeschke to review some hypotheses about SARS-CoV-2 and take a closer look at the potential drugs under investigation.
Roman Jaeschke, MD, MSc: Good morning. Welcome to another edition of McMaster Perspective. I have the pleasure of talking to Professor Miłosz Parczewski.
Professor Parczewski, maybe let’s have a few words of introduction first.
Miłosz Parczewski, MD, PhD: I’m Miłosz Parczewski. I’m an infectious disease physician, professor of medicine, head of the Department of Infectious Diseases, Tropical Diseases, and Acquired Immunodeficiency at Pomeranian Medical University in Szczecin, Poland. I’m also head of the Polish Scientific AIDS Society, where we’re leading research and guidelines.
Roman Jaeschke: Let me start with the following question: the mortality from coronavirus disease 2019 (COVID-19) in Poland seems to be quite a bit lower than in a number of other countries. Do you have any hypothesis to explain this phenomenon?
Miłosz Parczewski: This is the exact question that we’ve been asking ourselves. As you know, the mortality rate in Spain or Italy, for example, approaches 10% or 11%, while in Poland it’s approximately 3%, depending on the day. In Germany, though, it’s 2.3% to 2.5%. So we could say not only that Poland has a better survival rate, or a lower mortality rate, than southern Europe, but also that there are huge discrepancies in mortality in northern versus southern Europe.
Why is that? I think one of the reasons is that populations in the south are markedly older. We know that there’s an almost linear association between mortality and age. So in these elderly or aging societies mortality will be higher.
There may be some unknown genetic factors [differing] between the north and the south. We don’t know that yet. But there’s also a speculation that the virus is slightly different and that there’s a different viral clade in the north and in the south, which may be slightly attenuated. We will have to sequence the virus. We have applied for our project using exactly this perspective. We will be sequencing the spike protein and genome to see if there are differences in mortality, virus infectivity, and pathogenicity based on the origin of the virus.
Roman Jaeschke: Fascinating. I hope we’ll learn something from it. That’s amazing. Questions will follow whether treatments will be similarly effective in different areas.
Let’s switch gears to something that is of major interest to me. I have interviewed people from different parts of the world and I see that we are behaving differently depending on the country we live in. I’ll try to phrase it as 2 extremes, but there’s a lot of in-between.
There’s one school of thought saying that we cannot wait for the results of randomized controlled trials (RCTs) and have to use “something.” The other school of thought is that it’s precisely the opposite: because we don’t know the efficacy or harms of different treatments, we should not use unproven therapies. The proponents of those views say it’s either unethical not to use “something” other than supportive therapy or that supportive therapy is all that we should be using because it’s unethical to use something that is unproven and may be harmful. I’m too old to say who is right here. I wonder if you could share with us your views on this.
Miłosz Parczewski: These are both very fair points, especially for treating physicians, like us. On the one hand, there’s the primum non nocere principle, firstly do not do harm. But on the other, we are faced with a completely new virus introduced into the populations. There are no data whatsoever on treatment. All treatment perspectives are only now developing.
Obviously you could think that there will be results of RCTs coming back, but so far these data are very limited. Of course, we are doing something that isn’t really most adequate: we are guiding treatment very often based on in vitro or in silico data that a drug might work, that there’s some sequence compatibility or protein compatibility in the drug action. We try to do that, but there’s no good data for many of the drugs we use.
I’m more optimistic about the approach “do as little harm as possible but try to introduce experimental therapy.” We do this quite a lot. We use a lot of experimental agents. We are based on Polish guidelines, but at the same time we’re in line with international guidelines. The Infectious Diseases Society of America (IDSA) guidelines, which have been just published, are very similar and even more cautious, saying we should “do something in the context of clinical trials but otherwise be very careful.” We use chloroquine, hydroxychloroquine, tocilizumab. We do not have remdesivir available, so we haven’t used it yet. But we try to apply to clinical trials from this perspective. We are also introducing the serum of people who have recovered with specific IgG antibodies. These therapies are evolving. Obviously this is not RCT-based. But otherwise, if we do not have anything [else], there’s case-series data, which are being published. I think it is also important to show practitioners worldwide these data on this very common and widespread disease.
Roman Jaeschke: I’m really grateful for presenting this point of view. We’ll talk about it a little bit more.
You are the first virologist I have the pleasure of interviewing. For the sake of both myself and the audience, could you educate us in a couple of minutes about different classes of drugs that are being considered? How do you see the landscape?
Miłosz Parczewski: The landscape is very difficult. If you want some virological background, we would have to go back to coronaviruses. We know this is a third major zoonotic transmission. We’ve had severe acute respiratory syndrome coronavirus 1 (SARS-CoV-1); SARS-CoV-2, which we’re experiencing right now; and Middle East respiratory syndrome coronavirus (MERS-CoV). There have been no drugs available that worked for the previous SARS-CoV-1 and MERS-CoV. Also nobody really developed drugs for coronaviruses, because these viruses are ubiquitous in nature. They result in self-limiting, mild symptoms, so nobody was focusing on them.
What people are trying to do now is to model the possibility of action of various drugs in vitro or in silica, in the computer, to see whether a drug can have inhibitory properties to various viral molecules.
One of the drugs that we have been discussing is lopinavir/ritonavir, or HIV protease inhibitors. They have some similarity to coronaviral proteases, but this similarity is on the amino acid level only, not on a genetic level, and it’s more theoretical, in vitro rather than practical. We know there have been first placebo-controlled trials saying that there’s no benefit from lopinavir/ritonavir treatment, at least statistically. The numbers are slightly better, but statistically there’s no difference.
Similarly, even remdesivir—basically the only directly antiviral drug from the agents that have been discussed—is for now also tested in vitro only. The in vivo studies are being implemented. There’re very limited data, and these limited data on the clinical use have been published without any control group, so they have to be interpreted with great caution.
Then we have the whole class of immunomodulators. This is why we use chloroquine, hydroxychloroquine, azithromycin: these are immunomodulators that are supposed to limit the cytokine storm.
As the last step, we have monoclonal antibodies, like tocilizumab, which are used when this cytokine storm, or the inflammation, is severe, when our interleukin-6 levels are increased. We try to implement this drug—experimentally, of course—to limit the inflammation and in this way limit the immunologic damage caused by the virus.
So these are the approaches. There’s the direct antiviral approach, without a drug that really works, immunological approach, and inflammatory approach. Let’s put it this way.
Roman Jaeschke: It’s a fascinating review of the field. I guess we still have the sera from the convalescent people.
Miłosz Parczewski: Exactly.
Roman Jaeschke: What you’ve also mentioned to me is a review of RCTs, which are taking place in Canada and around the world. Maybe we’ll have another discussion about what is happening in Poland at the moment, but we’ll leave it for next time.
I really appreciate your time and hope at least one of these classes of drugs you mentioned will be of major use for our patients. Thank you very much.
Miłosz Parczewski: We hope so too. Thank you very much. It was a pleasure.
 English
English
 Español
Español
 українська
українська