Dr James Douketis, an expert in thrombosis, joins Dr Roman Jaeschke to discuss recent changes in recommendations for prophylactic anticoagulation in patients with coronavirus disease 2019 (COVID-19).
For a Publications of the Week article discussing COVID-19 and thrombosis prevention, click here.
Roman Jaeschke, MD, MSc: Good morning. Welcome to another edition of McMaster Perspective. This edition is prompted by recent practice guidelines on using anticoagulation among people with COVID-19. I welcome Professor Jim Douketis from McMaster University.
Jim, a few days ago I had a visit of a 26, 27-year-old person who told me that our meeting was delayed because he got quite a severe COVID-19. And when I asked what he meant by severe, he said he was at home, he was really breathless, he was desaturating (he had an oximeter at home), and he had severe chest pain; and his desaturation was down to 80s. With that, I asked him how he thought, what was the cause of it, because he didn’t think he had “pneumonia,” and he said, “Oh, I probably had some pulmonary emboli.” So, this is the introduction of the problem. How common is it? And what should we be doing about thromboembolic phenomena in COVID-19, according to both these practice guidelines and, more importantly, to you?
James Douketis, MD: Well, Roman, we’re hopefully at the tail end of the pandemic, but these are questions that remain and likely will remain relevant indefinitely, that is, how to best manage patients with COVID-19 pneumonia. And in this case, we’re going to be talking about what the role of anticoagulants is.
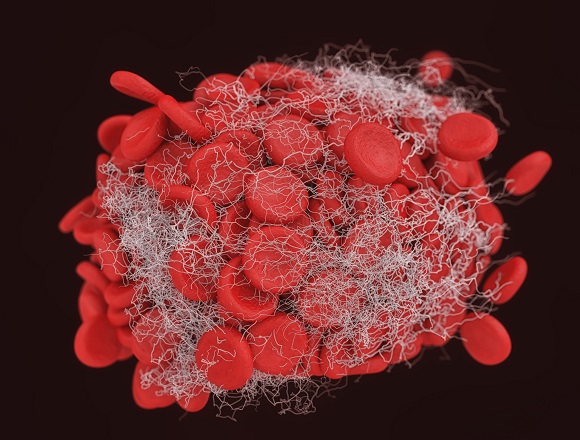
Just to step back a little bit, we all know that early on in the pandemic—in the spring and summer of 2020—it was recognized that there was a very high rate of thrombosis, pulmonary embolism, deep vein thrombosis in patients with COVID-19 who were hospitalized. This occurred despite them receiving prophylactic anticoagulation and, of course, led to the initiation of multiple—and I would say at least 50 if not more—randomized controlled trials looking at various anticoagulants, looking at various intensities of anticoagulants, looking at antiplatelet drugs, and looking at an array of other drugs with anticoagulant properties. And in the ensuing 1 to 2 years, a lot of these results from these trials became published and, of course, many medical societies looked at this evidence and rapidly mobilized efforts to develop practice guidelines to inform clinicians about best practice. So, the guideline we’re talking about today, which is from the International Society on Thrombosis and Haemostasis, is one of these guidelines from, as I said, a number of societies. And it’s probably the most up to date, although other groups are in the process of updating guidelines as part of a living guideline process. I think it’s important to put that into the context overall, vis-a-vis the pandemic, and I’m happy to discuss some of the main findings from these practice guidelines.
Roman Jaeschke: Please do.
James Douketis: I think that if you want to have a takeaway message with any kind of guideline, let’s have a look at how many of these recommendations are strong, based on high-quality evidence. And because the bar is so high these days, it’s not surprising that there are relatively few strong recommendations. And these recommendations are primarily in patients who are hospitalized but are not in a critical care setting. So, what do we mean by that? We mean that they may be receiving supportive care, they may be receiving oxygen, but they’re not receiving a high-flow nasal cannula oxygen or, of course, are not being ventilated and/or receiving inotropic support. But these are patients who are sick and maybe the case that you’ve just described would be better treated in a hospital setting, where they can receive oxygen, where they can receive an array of anti-inflammatory, antiviral, immunomodulating, and potentially anticoagulant therapy. So, the patient you’ve just described... The guidelines sort of refer to this individual and they actually make a strong recommendation that the patient should receive some form of anticoagulation, a strong recommendation in favor of prophylactic anticoagulation over no anticoagulation. And we would probably do that anyway, because this is somebody who’s a hospitalized, medically ill patient, and they typically would receive anticoagulant prophylaxis.
But the guideline goes on a step further [with] another strong recommendation [that] a therapeutic dose regimen would be advised over a prophylactic or an in-between or intermediate dose regimen, with an important caveat. And the caveat is that this would be a patient who would be at low risk for bleeding and who would have other markers that might indicate a worse prognosis. And these markers could be an elevated D-dimer. So, a D-dimer level... In most labs, the cut point is 500 nanograms per mL and in the practice, we consider a high D-dimer ≥2 times but more likely 4 times that cut point. And the second criterion is their oxygen requirement. This is something that we know portends a worse prognosis. The intent here would be that we are administering a therapeutic dose anticoagulation and the guidelines provide a strong recommendation for this in patients who are at low risk for bleeding, may have other markers of hypercoagulability like D-dimer, or may have impaired respiratory function manifested by high oxygen requirements.
And what are we doing by giving the anticoagulant? Well, we first have to understand that in no other circumstance in clinical medicine have we been administering a therapeutic dose of an anticoagulant to prevent thrombosis—in other words, in patients who don’t have a clot. And this is a big paradigm shift. But we also have to think and remember that in COVID-19 we’re not just giving the anticoagulant to prevent thrombosis, but we’re also trying to use the anticoagulant anti-inflammatory effect to mitigate this pathway of thromboinflammation where clots develop not so much in the lower extremities and then they migrate to the lungs, but they develop in situ as a result of the localized pulmonary inflammation mediated by the viral invasion. So, these strong recommendations to give an anticoagulant over nothing and to prefer a therapeutic dose anticoagulant over a prophylactic or intermediate dose, with caveats, I think are the 2 big messages.
The third message is to avoid the addition of antiplatelet drugs. That doesn’t seem like the antiplatelet agents have any additional therapeutic benefit, whether in this setting or other settings. So, that to me is the takeaway. But having said that, this has been a controversial area over the last year. And what I mean by that is that some guidelines have not been as much in favor of using therapeutic anticoagulation in noncritically ill patients. So, I think we have to recognize that a lot of the trials were not just designed to look at the effect of heparin on thrombosis, but they were looking at the effect of heparin on other clinical outcomes, most notably organ failure–free survival days. So, we have to keep that in mind and be a little bit broadly minded. And that’s why we need to select our patients, find those individuals who are at low bleeding risk. We think that the addition of heparin will favorably alter the clinical course of that individual.
Roman Jaeschke: Well, thank you for this practical information on how to identify those patients. We interacted with a number of people with COVID-19 over the last 2 years. The one other thing that struck me here is that we seem to distinguish between patients hospitalized outside of intensive care and hospitalized in the intensive care. To complement what you were saying, the tendency is obviously not to fully anticoagulate people who are in the intensive care, especially those who are ventilated invasively. The interesting thing is [management] in some people who are in between, because, for example, some people on noninvasive ventilation or on a high-flow nasal cannula in some institutions will be on the medical floor, so to speak, and in other institutions, they will be in an intensive care unit. So, it’s difficult to do it on a geographical basis—probably similar to what you mentioned. The patient I described was at home. He was young and did well. On the other hand, if he had shown up in hospital, he probably would have been at least considered for anticoagulation. So, we clearly are not in a black-and-white area and there is a lot of grayness, but less than we had 2 years ago.
And the last question: this guideline mentioned a medication, which I heard about for the first time, called sulodexide. Can you comment on it? It seems to be an oral anticoagulant.
James Douketis: It is an agent that I’m, frankly, not very familiar with because it is not used in Canada or other countries in North America; [it is used] mainly in Europe and Asian countries. So, like many clinicians, I do not have specific experience with it. I mean, I can say that a number of different drugs with anticoagulant properties have been investigated for COVID-19. This is one of them, and I would suggest that it should only be limited to clinicians who have experience with it. The fact that it’s an oral agent provides some attractions. The totality of evidence, though, is going to be considerably limited, even if individual studies suggest that there is benefit.
The other point I would like to bring out when we’re considering the context of these guidelines is that in late 2022, we’re in a very different world than we were in the spring or summer of 2020. We all remember that those patients walking into the COVID-19 unit at that time were sick and they had a rapidly progressive disease. And now we’re dealing with a population that has immunity, either through vaccination or naturally acquired through infection. And we already have an array of anti-inflammatory, antiviral, and immune modulatory treatments for COVID-19. So, it begs the question, Roman, what is the value of an anticoagulant in that context? And I think it behooves the need for further research in what we could refer to as contemporary COVID-19, whether it’s the Omicron BA.4 or BA.5 variant or evolving variants that we will probably be seeing in the coming years and indefinitely. And that is why I think we have to be very careful about extrapolating too much these data into everyday practice. And even the patient who you started off with may on paper seem like a good candidate for anticoagulation but may do well just with oral antiviral agents that will avert the need for hospitalization. So, a very different paradigm clinically and we need to place guidelines like this, which are very important, within that kind of today’s current context.
Roman Jaeschke: Well, thank you very much for raising some more doubts in my mind [laugh], but it’s very useful and thank you for your time and expertise. Goodbye.
James Douketis: It’s been my pleasure. Thank you.
Roman Jaeschke: Thanks.
 English
English
 Español
Español
 українська
українська