ISTH guidelines for antithrombotic treatment in COVID-19
For a McMaster Perspective interview discussing the guidelines, click here.
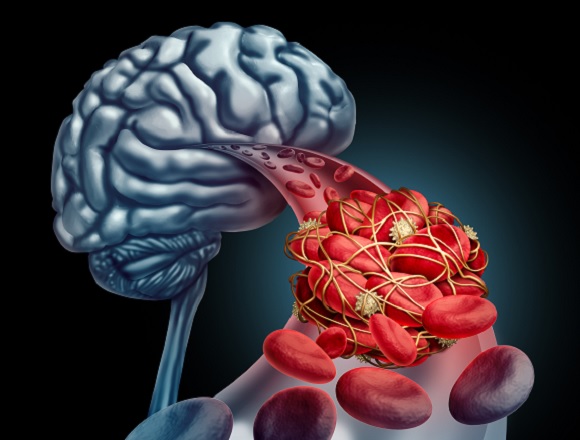
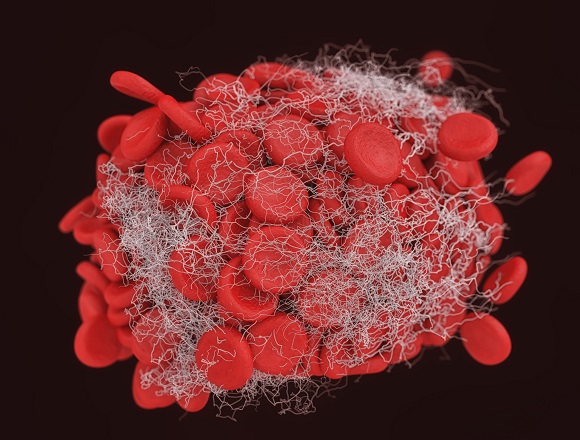
Background: Early in the pandemic it was observed that patients hospitalized for coronavirus disease 2019 (COVID-19) were at increased risk of venous thromboembolism and, to a lesser extent, other arterial cardiovascular events. The postulated pathophysiology was that the heightened immune response from COVID-19 confers a hypercoagulable state referred to as “thromboinflammation” and manifests with a markedly elevated D-dimer level, in situ pulmonary emboli, and other thrombotic events.
Over 50 randomized trials were launched, beginning in mid-2020, to assess an array of anticoagulant and antiplatelet drugs in patients with COVID-19, whether receiving critical care (intensive care units [ICUs]), noncritical care (hospital wards), or staying in the nonhospital (outpatient) setting. The putative benefits of anticoagulants, especially unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH), which have anti-inflammatory and antithrombotic properties, would be to attenuate the thromboinflammation so as to reduce morbidity and mortality related to COVID-19.
Methods: In response to rapidly evolving clinical trial evidence, in late 2021 the International Society on Thrombosis and Haemostasis (ISTH) assembled an international panel of content experts, patient representatives, and a methodologist to develop recommendations on anticoagulant and antiplatelet therapy for patients with COVID-19 in different clinical settings. The guideline methodology was based on the American College of Cardiology Foundation/American Heart Association formulation to assess the level of evidence (LOE) and class of recommendation (COR). Only recommendations with LOE A or B were included in these guidelines.
Results: The guideline provides 3 strong-level recommendations for noncritically ill patients hospitalized with COVID-19: (1) in favor of administering prophylactic-dose (low-dose) LMWH or UFH over no LMWH or UFH to reduce the risk of thromboembolism and, possibly, death; (2) in favor of administering therapeutic-dose LMWH or UFH in selected patients (eg, those at low bleeding risk and with elevated D-dimer levels or increased oxygen requirements) over prophylactic-dose or intermediate-dose LMWH or UFH to reduce the risk of thromboembolism and end-organ failure; and (3) against the addition of an antiplatelet agent, which is potentially harmful.
The panel gave 3 weak recommendations: (1) in favor of sulodexide, a glycosaminoglycan agent used in some parts of the world, in nonhospitalized patients; (2) adding an antiplatelet agent to prophylactic-dose LMWH or UFH in selected critically ill patients; and (3) prophylactic-dose rivaroxaban for selected patients after discharge.
Noteworthy, moderate-level recommendations in critically ill (ICU) patients with COVID-19 were: 1) intermediate-dose LMWH or UFH is not recommended over prophylactic-dose LMWH or UFH to reduce the risk of adverse events, including mortality and thromboembolism; and 2) therapeutic-dose LMWH or UFH is not recommended over usual-care or prophylactic-dose LMWH or UFH.
McMaster editors’ commentary: The recommendations from the ISTH, like those of other medical societies, reflect evidence accumulated during the pandemic. During that time, nonanticoagulant therapies comprising glucocorticoids, antiviral drugs, and immunomodulatory agents have become established treatments for COVID-19. In addition, the widespread use of vaccination and acquisition of infection-related immunity have altered and, in general, diminished the severity of infection with newer severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants. Consequently, further research is needed to evaluate anticoagulant strategies within the current context of other established treatments and present or emerging viral strains.
 English
English
 Español
Español
 українська
українська