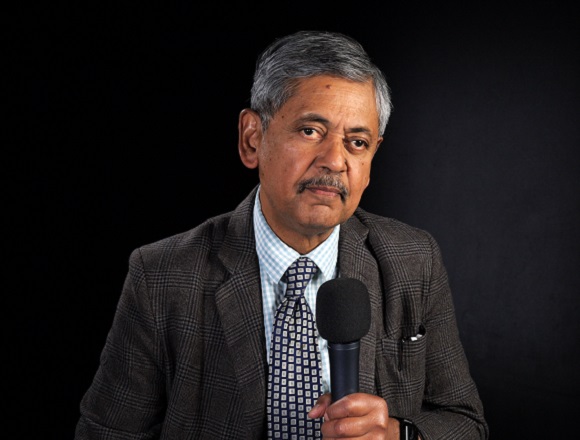
Andrzej Maciejczak, MD, PhD, is a professor and head of the Department of Neurosurgery at the University of Rzeszów, Poland.
When should we urgently qualify a patient with back pain syndrome for surgery?
Back pain is usually managed conservatively because the vast majority of patients will be treated conservatively unless you diagnose or find a red flag in such a patient.
Red flags could be, first, neurological deficits, namely paresis. It often happens in patients with sciatica, which is a leg pain produced by disk herniation or disk prolapse. Normally, sciatica doesn’t present with paresis, but when it happens, you need to send that patient to surgery as soon as possible because there is a real and proven association, which is this correlation between the timing of surgical nerve decompression and improvement of motor deficits. I recommend testing muscle strength in all patients with sciatica. You need to ask the patient to walk or stand on their toes or heels to check whether the patient has any motor deficits or not. Once you detect it, send the patient timely to surgery.
Of course, other red flags are those conditions like spine tumor, which produces very characteristic back pain that aggravates at night and is progressive in nature. You should suspect the neoplastic nature of low back pain in a patient with the history of cancer disease who develops new or [aggravated] usual back pain.
There is also a very common condition called osteoporotic fractures of the spine, which are commonly seen in primary care. Patients with osteoporotic fractures are mostly affected at an older age. [The management of] the osteoporotic fracture should be started with conservative treatment, but don’t drag out this treatment. In [the case of] patients with osteoporotic fracture, after 2 or 3 weeks of inefficient treatment, you need to send them to a specialist for the augmentation of the vertebral body with the use of bone cement. Elderly patients suffer from back pain in such a way that they are normally bedridden for a few days. But if it prolongs, you need to encourage the patient to avoid bedrest. Bedrest carries thromboembolic complications and pneumonia, so it’s better to send the patients after 3 or 2 weeks of ineffective treatment for vertebroplasty.
Vertebroplasty is a procedure that is commonly used and that is one of the most effective procedures I have ever seen in spine surgery. Injection of semiliquid bone cement into the vertebral body does the trick and provides immediate pain relief and, in addition, prevents the fracture site against kyphotic deformity, which may complicate further illness.
Another condition that requires urgent treatment is cauda equina syndrome. Cauda equina syndrome is usually produced by massive disk prolapses, which produce bowel retention and bladder retention, bowel and bladder incontinence, distal leg paresis, and sexual dysfunction. These patients require emergency treatment even at night on call.
These are roughly the red flags you need to exclude before you start conservative management because, as I mentioned, the vast majority of patients with back pain will require conservative management. Once you exclude the red flags, you may treat them safely. But if there is a red flag, you need to send the patient to surgery as soon as possible and very timely.
 English
English
 Español
Español
 українська
українська